Keywords
INTRODUCTION
Given the elevated morbidity and mortality of patients with ischemic cardiomyopathy (IM), the diagnosis of myocardial viability (MV) in these patients is relevant as this can change the therapeutic strategy and improve prognosis.1 Myocardial viability has been studied using different imaging techniques such as single-photon emission computed tomography (SPECT),2 positron emission tomography (PET),3 ultrasonography,4,5 magnetic resonance imaging,6 and multidetector computed tomography.7 The prognosis of patients with a given level of MV according to gated-SPECT and technetium-labeled contrast agents varies depending on the treatment received. This work analyzes the effects of coronary revascularization (CR) and medical treatment (MT) on cardiac mortality (CM) in patients with AMI satisfying MV criteria according to gated-SPECT imaging performed at rest using technetium-labeled contrast agents.
METHODS
Patients
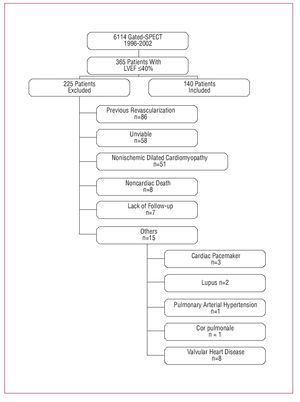
Between July 1996 and July 2002, our nuclear cardiology unit assessed myocardial perfusion in 6114 consecutive patients using gated-SPECT with technetium-labeled contrast agents. The present study included 140 consecutive patients with AMI who fulfilled the selection criteria (patients with ischemic heart disease and an ejection fraction [EF] £40% in the absence of any other associated heart disease who satisfied MV criteria and who had not undergone previous revascularization) (Figure 1).
Figure 1. Flowchart of patients included in this study.
Gated-SPECT Myocardial Perfusion at Rest
All patients were studied at rest using gated-SPECT. Each patient was administered a dose of 24 mCi of 99Tc-tetrofosmin (n=123) or MIBI (n=17). The equipment used was a 90o dual-head gamma camera (E.cam, Siemens Medical Systems, Erlangen, Germany) provided with a high resolution collimator, 180o semicircular orbit, in step-and-shoot mode, starting at 45o right anterior oblique projection with image acquisition every 3o (25 s). Image acquisition was synchronized with the electrocardiogram R wave and the cardiac cycle was divided into 8 intervals. The reconstruction method was filtered back-projection (5th-order Butterworth filter; cutoff frequency, 0.4). Attenuation and scattering corrections were not performed. Myocardial viability was analyzed in akinetic and dyskinetic regions as well as in those with severe hypokinesia. All patients studied at rest using gated-SPECT satisfied the viability criteria accepted in our unit. That is, out of 17 myocardial segments, less than 3 had perfusion and wall thickening scores III-IV (severe dysfunction or absence of thickening) in the akinetic and dyskinetic regions.8
Follow-up
Mean clinical follow-up after gated-SPECT (2.4 [1.2] years; median, 2.3 [25th percentile = 1.4; 75th percentile = 3.2]) was conducted by the cardiologist in the hospital outpatient service (n=30) and by telephone (n=110). Cardiac mortality and the CR procedure (surgery or coronary angioplasty) were evaluated.
Study Design
This was a retrospective clinical study which analyzed the clinical characteristics of patients at rest using gated-SPECT and the effects of CR (surgery or coronary angioplasty) at follow-up. The effect of treatment on CM was also studied.
Statistical Analysis
Continuous variables were compared using the Student t test for independent samples and expressed as mean (standard deviation). Differences between 2 proportions were compared with the c2 test or Fisher's exact test, and results given as percentages.
The effect of CR and MT were analyzed using Cox regression controlling for confounding and interaction. Interactions were assessed (CR and AMI [previous acute myocardial infarction], CR and RSCD [regions with severe contractility dysfunction] and CR and women) using an overall test of significance (chunk test) according to the likelihood ratio, without reaching statistical significance. The model included significant variables from the univariate analysis, plus the variables history of hypertension and diabetes. The relative risk of CR and of MT was expressed as hazard ratios (HR). The survival curves were compared using log-rank and Breslow tests (Kaplan-Meier method). A P value less than .05 was considered significant. The statistical analysis was performed using SPSS for Windows software, version 13.0. (SPSS, Chicago, Ill., USA)
RESULTS
Table 1 shows the clinical characteristics of the total population and those obtained with gated-SPECT at rest as well as these when grouped by CR and MT.
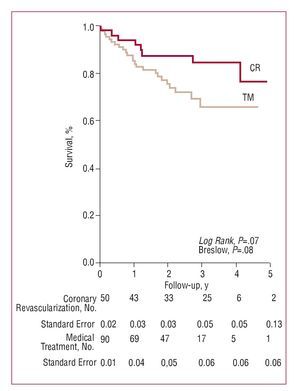
Following gated-SPECT, CM was 22.8% (n=32) during follow-up (2.3 [1.2] years). In revascularized patients (n=50), CM was 16.2% (n=8; 5.9/100 patients/y), and in MT patients (n=90) CM was 26.7% (n=24; 12.9/100 patients/y). The nonadjusted Kaplan-Meier analysis (Figure 2) showed that there were lower survival rates among MT patients, with the results almost reaching statistical significance. The adjusted treatment effect by Cox regression analysis (Table 2) showed a marginally significant protective effect against CM among the CR patients. Coronary revascularization multiplied the risk of CM by 0.42 compared to MT (95% confidence interval, 0.17-1.01; P=.05). No significant differences were found in CM in relation to the type of revascularization (surgical vs angioplasty, 17% vs 13.3%, respectively; P=.73).
Figure 2. Kaplan-Meier survival analysis in patients with viable myocardium undergoing coronary revascularization (CR) and medical treatment (MT). "Standard error" refers to the cumulative survival rate.
DISCUSSION
A metaanalysis assessing different techniques showed that MV is a prognostic variable of CM and that mortality is lower among CR patients.9 However, to date, no studies have been conducted on the prognostic effect of CR in patients with AMI who satisfy MV criteria assessed by gated-SPECT at rest and technetium-labeled contrast agents. Positron emission tomography is the standard technique for studying MV, but it is expensive and rarely available in most hospitals. Thus, a good alternative is gated-SPECT with technetium-labeled contrast agents, which currently is the most widely used technique for assessing myocardial perfusion. Using this methodology, Levine et al10 observed that the sensitivity and diagnostic accuracy of myocardial viability improved when SPECT was synchronized with ECG.
In our series, the MT patients who satisfied MV criteria according to gated-SPECT imaging at rest had greater CM than the CR patients, although the results were just below the limit of statistical significance. Annual mortality was double in MT patients with AMI and MV compared to that in CR patients. These results are compatible with those found in previous studies conducted with echochardiography,9 magnetic resonance imaging,11 PET,3,12 and TI-201 myocardial perfusion scintigraphy.13 Studies that have used technetium together with PET to analyze myocardial metabolism have found a significant reduction in cardiac event rates (death, acute myocardial infarction, unstable angina, cardiac transplantation, and survived resuscitation) only in patients with viable myocardium.14 A metaanalysis conducted by Allman et al,9 and a more recent one by Bourque et al,15 included studies with SPECT, PET and echocardiography with more than 1000 patients and found a close relationship between MV and significantly improved survival rates after a CR procedure.
Our study is based on a retrospective clinical analysis where the physician's decisions and some patient characteristics (age, comorbidity, unsuitable coronary anatomy) may have influenced therapeutic decisions regardless of the results obtained with gated-SPECT relating to MV. Although the hazard ratio is very high, the association of mortality with the type of treatment received is marginally significant, and so these results should be interpreted with caution. This is a limitation in our series and is also found in other published studies.
Based on our results, we conclude that coronary revascularization has a protective effect on patients with ischemic cardiomyopathy who satisfied myocardial viability criteria assessed by gated-SPECT myocardial perfusion imaging.
This study has been partially financed by a fellowship grant from the Carolina Foundation and by funds from RECAVA (Thematic Networks and Cooperative Research), Instituto de Salud Carlos III, Spain (RED C03/01, RECAVA).
Correspondence:
Dr. J. Candell-Riera.
Servei de Cardiologia. Hospital Universitari Vall d'Hebron. Universitat Autònoma de Barcelona.
Pg. de la Vall d'Hebron, 119-129. 08035 Barcelona. España.
E-mail: jcandell@vhebron.net
Received October 5, 2007.
Accepted for publication October 24, 2007.