Following the publication of the Spanish Position Paper on Cardio-Oncology,1 Hematología, in order to evaluate the current status of the field of cardio-oncology in Spain, our National Cardio-Oncology Working Group, composed of representatives of the Spanish Societies of Cardiology (SEC), Medical Oncology (SEOM), Hematology and Hemotherapy (SEHH) and Radiation Oncology (SEOR), conducted a nationwide survey aiming to analyze the perceived importance of the screening and management of cancer-related cardiovascular (CV) complications and the institutional relationship among specialists involved in the care of cancer patients (supplementary material).
Following the publication of the Spanish Position Paper on Cardio-Oncology,1 Hematología, in order to evaluate the current status of the field of cardio-oncology in Spain, our National Cardio-Oncology Working Group, composed of representatives of the Spanish Societies of Cardiology (SEC), Medical Oncology (SEOM), Hematology and Hemotherapy (SEHH) and Radiation Oncology (SEOR), conducted a nationwide survey aiming to analyze the perceived importance of the screening and management of cancer-related cardiovascular (CV) complications and the institutional relationship among specialists involved in the care of cancer patients (supplementary material).
We designed an electronic survey distributed nationwide through the 4 above-mentioned scientific societies. Only 1 questionnaire was delivered to division chiefs; however, answers by heads of section and assistants were accepted. The study period was from September 2016 to June 2017. Multiple electronic reminders were sent to nonrespondents during this period.
A total of 202 answers were received: 58 (29%) from medical oncologists, 36 (18%) from hematologists, 51 (25%) from radiation oncologists, and 57 (28%) from cardiologists. The overall response rate was 39%. Most of the responses came from tertiary hospitals (65.3%).
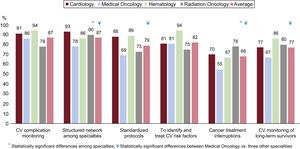
The survey asked the responder to score the perceived importance of various key points related to cardiotoxicity from 1 (least important) to 10 (most important). The Figure reflects the percentage of respondents from each specialty who considered each issue very important (score 8 to 10). Most participants (87%) agreed that potential CV complications related to cancer therapy must be monitored and felt that a structured network among specialties and standardized protocols might improve the complex care of patients with cancer and CV disease (87% and 79%, respectively). They recognized the value of identifying and treating CV risk factors (82%), and 77% of them considered the development of long-term survivorship programs highly important. The existing literature suggests that early cancer treatment interruptions had a negative impact on cancer prognosis2; however, the perceived importance of this issue was less consistent across respondents (ranging from 55%-78%).
Average number of respondents from each specialty who considered each question as very important (score 8 to 10) on a scale from 1 to 10 points. Questions: 1. How important is monitoring patients for CV complications during cancer treatment period? 2. Do you think it is necessary to implement a structured network among the distinct specialties involved in the care of cancer patients? 3. Do you think the development of a standardized protocol for the follow-up of CV complications is important? 4. Do you consider it essential to identify and treat CV risk factors in cancer patients? 5. How important is the impact of cancer treatment interruptions in cancer prognosis? 6. Do you believe long-term monitoring cancer survivors for CV complications is valuable?
CV, cardiovascular.
While most respondents felt that cardiotoxicity had a strong impact on cancer patients, only 24 centers (12%) reported the existence of a structured cardio-oncology unit. Thirty additional respondents (14.8%) had a dedicated cardiologist in charge of the care of patients with cancer-related CV complications. Unfortunately, the remaining 148 centers (73.3%) offered no specific cardio-oncology services, but 76 (13.4%) participants planned to add them in the near future.
Most of the centers reported that the main barriers to the establishment of a cardio-oncology unit were departmental priorities (38.6%), lack of funding (5.9%), and the absence of evidence-based guidelines and attending physicians with specialized training (17%).
In 71% of centers, the baseline assessment of cardiotoxicity risk and the decision to refer patients to the cardiology outpatient clinic were performed by cancer specialists. Follow-up focused on cardiotoxicity was scheduled according to a specific protocol in only 25% of the centers; accordingly, in up to 58% of the centers, this monitoring was carried out without a specific protocol. In all, 94% of participants confirmed the use of echocardiography as the first technique for cardiac monitoring. However, 37% of them reported that they still used isotopic ventriculography due to the lower availability of echocardiography in their centers. Only half of the participants reported the use of cardiac biomarkers in their clinical practice and there was wide heterogeneity among specialties. Once cardiotoxicity occurs, 27% of participants reported that all patients were evaluated by the cardio-oncology team or referred to the cardiology clinic. However, 60% stated that only selected patients were referred to a cardiologist (Table).
Main Results Regarding Cardiotoxicity Risk Assessment, Methods for Monitoring, and Management
| Medical oncology, % | Radiation oncology, % | Hematology, % | Cardiology, % | Overall, % | |
|---|---|---|---|---|---|
| Baseline evaluation of CTX risk is performed by a cancer specialist | 68.9 | 74.5 | 77.1 | 67.2 | 71.3 |
| Cardiac monitoring during cancer treatment with no protocol | 56.9 | 47.5 | 61.1 | 66.7 | 58.5 |
| Echocardiography is used for CTX screening | 98.3 | 85.4 | 94.4 | 98.2 | 94.5b |
| Echocardiography is the imaging technique of choice used for CTX screeninga | 64 | 31.4 | 58 | 86 | 63.4b |
| Isotopic ventriculography is used for CTX screening. | 41.4 | 52 | 23 | 28 | 36.9b |
| Isotopic ventriculography is the imaging technique of choice used for CTX screeninga | 24.1 | 41.1 | 17.6 | 5.2 | 25.2b |
| 11.1 Biomarkers are used for CTX screening | 34.5 | 31.8 | 72.2 | 59.6 | 48.2b |
| Patients with overt CTX are assessed by cancer and cardiology specialists jointly | 47.4 | 21.6 | 19.4 | 17.5 | 27.4b |
| Patients with overt CTX are assessed by a cancer specialist and only selected individuals are referred to a cardiologist | 47.4 | 56.9 | 66.7 | 71.9 | 60.2b |
| Less than 100 new cancer patients referred for cardiology consultation annually | NA | NA | NA | 52.6% | NA |
| Number of echocardiography studies done in cancer patients | NA | NA | NA | < 100: 24.6% 100-500: 47.4% 500-1000: 19.3% > 1000: 7.0% Don’t know/no answer: 1.7% | NA |
| Number of cardiac imaging studies done in cancer patients | NA | NA | NA | < 100: 28% 100-500: 31.6% 500-1000: 12.3% > 1000: 10.5% Don’t know/no answer: 17.5% | NA |
CTX, cardiotoxicity; NA, not applicable.
Our results reflect a meaningful awareness of the detrimental impact of cardiac toxicity on the outcome of cancer patients. This is in the same line as previous surveys, in which most participants acknowledged CV toxicity from cancer treatments.3,4 36% Nevertheless, the percentage of centers with an established cardio-oncology unit is far lower in our country (12%) compared with the rate of 27% reported in hospitals in the United States.3 Since baseline assessment of cardiotoxicity risk is generally performed by noncardiologists in our setting, local monitoring protocols are mandatory to improve CV care. Our survey underscores the need for close collaboration between cancer specialists and cardiologists, further specific education, and more resources to allow the existence of a well-established cardio-oncology structure.
The limitations of our study are the response rate and the heterogeneous distribution of respondents among the specialties.
We gratefully acknowledge the collaboration of members of the Spanish National Cardio-Oncology working group: Dr Pascual Marco Vera, Dr Juan José González Ferrer, Dr Ángel Montero Luis, Dr Juan Antonio Virizuela Echaburu, Dr Sebastia Sabater, and Dr Andrés Iñiguez Romo.