Substantial progress in transcatheter cardiac interventions has allowed the treatment of a large number of patients with poor surgical prognosis. Comorbidities, frailty, and concurrent cardiac diseases in elderly patients often limit the option of surgery. Some patients with these factors are considered inoperable while others are deemed at high surgical risk. The indication for intervention in this latter group of patients is subject to debate, as the decision depends on assessment of a given multidisciplinary team and agreement by a specific surgical team. We describe the case of an inoperable female patient with several cardiac diseases who was successfully treated by percutaneous intervention, with subsequent clinical improvement.
A 70-year-old woman, diagnosed with long-standing obstructive hypertrophic cardiomyopathy and in New York Heart Association functional class II was admitted to hospital for the first time in March 2013 with heart failure (HF) associated with atrial fibrillation. Electric cardioversion was effective. Subsequently, in the same year, she was hospitalized once again due to HF with preserved sinus rhythm. The electrocardiogram showed severe, asymmetric, septal, and obstructive left ventricular hypertrophy (baseline dynamic subaortic pressure gradient, 80mmHg), preserved left ventricular ejection fraction, severe mitral regurgitation, and severe pulmonary hypertension with mild right ventricular dysfunction. A dual mitral valve regurgitation mechanism was observed by transesophageal echocardiography, with a functional component resulting from systolic anterior motion of the mitral valve, and another predominant regurgitation jet along the anteroseptal direction due to posterior mitral leaflet prolapse (Figure 1A, Figure 1B, and Figure 1C). In addition, a coronary angiography was performed before the patient was referred for surgery. This showed severe ostial stenosis of the left main coronary artery, a mild distal lesion in the left anterior descending artery, and dominant right main coronary artery with no lesions (Figure 1D, solid arrow). Right cardiac catheterization showed severe reactive postcapillary pulmonary hypertension, transpulmonary gradient of 39mmHg, pulmonary capillary pressure of 23mmHg, and significantly increased pulmonary vascular resistance (8-9 UW). It was decided to perform myectomy, coronary revascularization, and mitral valve repair, but surgery was ruled out due to the high surgical risk (EuroSCORE II, 11.4%; Society of Thoracic Surgeons score, 6.8%), principally because of severe pulmonary hypertension with a fixed component and the need for emergency surgery with 3 surgical procedures. A percutaneous coronary intervention was therefore considered. The diseased coronary artery was treated by placement of a drug-eluting stent (everolimus 4 × 12mm) in the left coronary artery (Figure 2A, solid arrow). Subsequently, the patient twice required readmission for HF. Three months after coronary artery revascularization, the left ventricular obstruction was treated by alcohol septal ablation (2mL) of the first septal perforator of the left anterior descending artery (Figure 2A, dashed arrow). This procedure was effective (maximum creatine kinase 1360 U/L; ultrasensitive T troponin 4804 pg/mL), although she required permanent DDDR pacemaker placement due to advanced second degree atrioventricular block. The patient improved clinically, with disappearance of the dynamic subaortic obstruction and systolic anterior motion of the mitral valve (Figure 2B, red arrow). However, she was readmitted for HF twice more. The mitral valve was therefore repaired using a MitraClip device in view of the satisfactory anatomical condition of the valve. This procedure was successfully performed using 2 mitral clips; the residual transmitral pressure gradient was not significant (< 4mmHg), with grade II/IV residual mitral valve regurgitation (Figure 2C and Figure 2D). She was discharged with no further incidents after the procedure. After 2 years of follow-up, a significant decrease in N-terminal pro-brain natriuretic peptide (from 32 512 to 3072 pg/mL) was observed, as well as improved New York Heart Association functional class (to functional class II). There were no further hospitalizations.
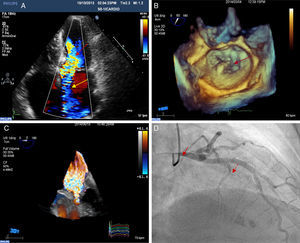
A: transthoracic echocardiogram showing dynamic obstruction of the left ventricle (red arrow) and mitral valve regurgitation in the anteroseptal direction due to organic valve disease (yellow arrow). B: 3-dimensional transesophageal echocardiogram with 3-dimensional zoom showing posterior mitral leaflet prolapse (arrow). C: 3-dimensional, full volume, color Doppler transesophageal echocardiogram showing severe mitral valve regurgitation. D: coronary angiography, 30° right anterior oblique view showing severe stenosis of the left main coronary artery (solid arrow) and septal branch treated with alcohol ablation (dashed arrow).
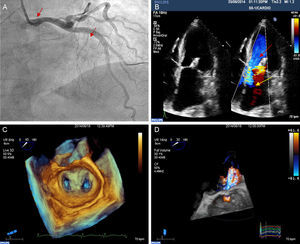
A: coronary angiography right performed in the 30° right anterior oblique view showing percutaneous revascularization of the left coronary artery (solid arrow) and lower visualization of the septal branch after alcohol ablation (dashed arrow). B: transthoracic echocardiogram showing disappearance of the left ventricular obstruction (red arrow) and reduced mitral valve regurgitation in the anteroseptal direction due to organic valve disease (yellow arrow). C: transesophageal echocardiogram with 3-dimensional zoom of the implanted MitraClip device. D: 3-dimensional, full volume, color Doppler transesophageal echocardiogram showing a significant decrease in mitral valve regurgitation after septal ablation and percutaneous repair of the valve.
This case is exceptional because of the percutaneous cardiac intervention for coronary heart disease, valve disease, and myocardial disease despite an established surgical indication.1 With this palliative approach, the different factors responsible for the refractory HF were treated sequentially, rather than simultaneously, as would have been the case with a surgical intervention. The sequential approach may have contributed to decreasing the risk associated with the intervention.2
The present case highlights 2 essential aspects of current treatment of cardiac patients. First, there is a broad evidence base derived from randomized studies, meta-analyses, and registries pointing to similar clinical outcomes with similar safety for percutaneous treatment and surgical treatment for many cardiac diseases.3–5 We believe that, at present, it is important to assess the percutaneous approach for complex patients when the case for surgery is not clear, with an established multidisciplinary team that takes individualized decisions, given that the percutaneous approach may be the only appropriate option for patients with a poor prognosis in the short- to mid-term. Second, as the indication for transcatheter valve treatment might be expected to become broader, the present case highlights the importance of performing an exhaustive assessment with imaging techniques of the pathophysiological and anatomical mechanism underlying valve disease. The most suitable repair strategy can be determined on a case-by-case basis with a view to ensuring a successful outcome.6