Keywords
INTRODUCTION
Arrhythmogenic right ventricular dysplasia (ARVD) is a disease of the cardiac muscle characterized in its final stages by replacement of normal myocardial tissue with fatty or fibroadipose tissue, leading to conduction and wall motion abnormalities in the myocardium. Both ventricles may be impaired, though the right ventricle (RV) is affected more often.1,2
The most common clinical manifestations are those caused by ventricular tachycardias (typically with left bundle branch block morphology) secondary to electrical instability of the RV myocardium. Tachycardias may range from ventricular premature beats with no clinical repercussions to sustained tachycardias that can degenerate into ventricular fibrillation. In advanced stages, right heart failure has also been described but this is very rarely the first manifestation of ARVD.3,4 The disease is most common in young men (in their twenties or thirties), and a third of the patients have a family history.1,5 The incidence of ARVD is estimated to be 1/5000, although this value will probably rise as clinical awareness of the disease is raised.6
Diagnosis of the disease is based on electrocardiographic, arrhythmic, histopathologic, genetic, and structural and functional criteria proposed by the Working Group for ARVD of the European Society of Cardiology.7 These criteria are classed as major or minor, and are accepted internationally. Those that provide information on RV function and structure play the most important role in diagnosis. Different imaging techniques can be used, such as echocardiography, angiography, and, more recently, cardiac magnetic resonance imaging (cardiac MRI). Echocardiography is of limited use for assessing RV regional wall motion abnormalities, and the patient may also be a poor candidate for echocardiographic study,8 but it remains a useful technique. Angiography is considered the gold standard and can also be complemented by taking biopsies to detect fatty infiltration but it is an invasive technique with possible complications. Cardiac MRI imaging is a noninvasive technique which provides a suitable assessment of the RV and so has been proposed as the imaging technique of choice for diagnostic assessment of patients with clinical suspicion of ARVD. Nevertheless, application of cardiac MRI in such patients is still questioned and its usefulness for detecting ARVD has not been confirmed.9-13
The primary objective of our study was to assess the diagnostic usefulness of cardiac MRI in patients with clinical suspicion of ARVD in our hospital, and to compare cardiac MRI and echocardiographic findings in patients who were studied with both techniques.
MATERIALS AND METHODS
In this retrospective study, we reviewed all requests for cardiac MRI between January 1993 and December 2002 in our hospital, and selected those that were done in patients with suspicion of ARVD. This process yielded 46 cardiac MRI studies, corresponding to patients who had presented with ventricular arrhythmias with left bundle branch block morphology and who had been referred to our hospital with suspected ARVD. The study population had a mean (SD) age of 42±19 years (range, 11-73 years), and comprised 25 men and 21 women.
These 46 patients had undergone cardiac MRI studies with a Siemens Magnetom 1.0T (January 1993 to May 2001) or a Philips Intera 1.5T (June 2001-December 2002). Both units were fitted with cardiac coils. To study the structure and fatty infiltration of ventricular walls, in particular in the RV free wall and outflow tract with the Siemens unit, we recorded T1-weighted spin-echo sequences (variable repetition time [RT] according to the patient's heart rate; echo time [ET], 30 ms; field of vision, 400 mm; section thickness, between 8 mm and 10 mm; matrix, 128x256). In the Philips unit, black blood sequences were recorded (RT, 1 ms; ET, 4.5 ms; flip angle, 90°; section thickness, 7 mm; matrix, 256x256). In both units, these sequences were recorded in axial thoracic and oblique sagittal planes referenced on the RV outflow tract. For study of RV and left ventricular function, and to detect overall or regional wall motion abnormalities, we recorded long- and short-axis cine images of the left ventricle using gradient-echo sequencing in the Siemens unit (RT, 50 ms; ET, 12 ms; flip angle, 60°; 16 phases) and balanced fast field echo sequencing (RT, 3.2 ms; ET, 1.6 ms; flip angle, 60°; section thickness, 10 mm; matrix, 160x256) in the Philips unit.
Abnormalities in the cardiac MRI studies were classified according to the diagnostic criteria for ARVD established by the working group of the European Society of Cardiology7 (Table 1), which are divided into major and minor criteria. Two cardiologists with extensive experience in cardiac MRI analyzed the images and agreed on a consensus finding. Both specialists were aware that ARVD was clinically suspected. The RV diameters were measured in the 4-chamber long-axis plane.
We then reviewed the medical histories of these 46 patients to check how many met the criteria of the European Society of Cardiology for diagnosis of ARVD and recorded which of these criteria were based on MRI findings.
Thirty-one of these 46 patients also underwent echocardiographic study in our hospital. We compared the ability of cardiac MRI and echocardiography to detect RV disease. To do this, we recorded the major and minor criteria met for both techniques in these 31 patients, as well as RV diameters. We also checked for differences in the final diagnosis when only one imaging technique was used. The echocardiographic RV end-diastolic diameter was measured in the parasternal long-axis view.
Statistical Analysis
The means of quantitative variables were compared with the Student t test, with statistical significance set to P<.05.
The sensitivity and specificity of the presence of fatty infiltration as a diagnostic criterion for ARVD were defined as the proportion of patients with or without dysplasia according to cardiac MRI with respect to the total number of patients with and without confirmed disease, respectively. The corresponding positive and negative predictive values were calculated from the ratios of true results/false positives and true results/false negatives, respectively. From these data, the 95% confidence intervals (CI) were calculated.
RESULTS
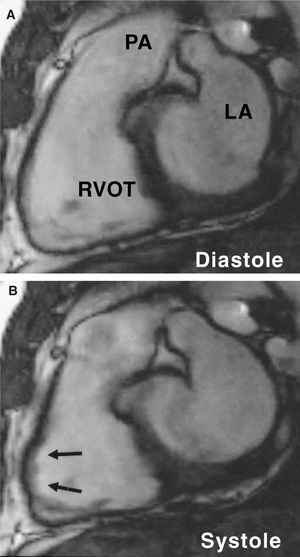
Assessable magnetic resonance images were obtained for all patients included in the study. No complications were reported and all patients tolerated the apneic periods satisfactorily. Right ventricular abnormalities in the cardiac MRI (whether major or minor criteria) were detected in 24 patients (52%), whereas no pathological findings were reported in the remaining 22 patients (48%) (Table 2). The most common finding in the cardiac MRI was regional akinesia/dyskinesia of the RV wall (14 patients) (Figure 1), but we did not detect any cases of severe segmental RV dilatation.
Figure. 1. Diastolic (A) and systolic (B) images from a cine-MRI (B-FFE) sequence from a long vertical plane of the right ventricular outflow tract. The images obtained allow motion abnormalities to be analyzed in detail. In this case, regional impairment can be seen with a clearly dyskinetic zone (arrows). LA indicates left atrium; PA, pulmonary artery; RVOT, right ventricular outflow tract.
Review of the medical histories of the 46 patients studied by cardiac MRI showed that only 5 of these finally met the general criteria required for ARVD (3 men and 2 women; mean age, 30 years). Four of these had at least one major criterion in the cardiac MRI and the other patient had 2 minor criteria (Table 3).
The RV end-diastolic diameter was significantly greater in the 5 patients diagnosed with ARVD (45 [3.08] mm) than in the remaining 41 patients (36.6 [5.16] mm) (P<.01).
Fatty Infiltration of the Right Ventricle
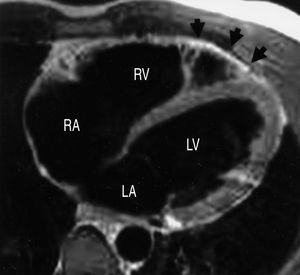
T1 spin-echo sequences or black blood images compatible with fatty infiltration of the RV were identified for 9 patients (Figure 2). This was the only pathological finding in 6 of these patients, whereas in the other 3, the finding was associated with RV wall motion abnormalities or RV dilatation. These latter 3 patients belonged to the group meeting the diagnostic criteria for ARVD. The sensitivity of the presence of fatty infiltration of the RV as a diagnostic criterion for ARVD was 60% (3/5) (95% CI, 23%-88%) and the specificity was 85% (35/41) (95% CI, 71%-93%). The positive predictive value was 33% (3/9) (95% CI, 12%-65%) and the negative predictive value was 95% (35/37) (95% CI, 82%-99%).
Figure 2. Axial black-blood image of the right ventricle, in which fatty tissue appears hyperintense (white). In this case, the hyperintense signal indicated with the arrows shows the presence of fat that has infiltrated the apical region of the right ventricular myocardium. RA indicates right atrium; LA, left atrium; RV, right ventricle; LV, left ventricle.
Echocardiography Versus Cardiac Magnetic Resonance Imaging
In the subgroup of 31 patients who were studied by both imaging techniques, echocardiography detected RV abnormalities (major or minor criteria) in 18 patients (58%), whereas cardiac MRI detected such abnormalities in 19 (61%) (P=1, NS). Both techniques detected a similar number of minor criteria--19 with cardiac MRI and 18 with echocardiography--but cardiac MRI detected twice as many major criteria as echocardiography--8 versus 4. After review of the medical histories, it was found that 4 of these 31 patients were diagnosed with ARVD. Table 4 shows the diagnostic criteria identified by cardiac MRI or echocardiography in these 4 patients with final diagnosis of ARVD. As seen in the table, if echocardiography had been the only diagnostic imaging test, 2 of these 4 patients would not have met diagnostic criteria for ARVD.
On the other hand, both techniques detected significant RV dilatation in the 4 patients diagnosed with ARVD. The RV end-diastolic diameter in patients with ARVD was 45.5 (3.31) mm versus 38.11 (5.08) mm in patients without (P<.05) when measured by cardiac MRI, and 33 (3.46) mm versus 27.25 (7.5) mm, respectively (P<.05), when measured by echocardiography.
DISCUSSION
In this study, cardiac MRI provided assessable data in all patients with clinical suspicion of ARVD. Cardiac MRI is a noninvasive reproducible technique which can be used for a very accurate assessment of RV function and structure in patients with clinical suspicion of ARVD.14,15 It is probably the best imaging technique for detecting RV structural and functional abnormalities.16 The main advantage of this technique for RV assessment is that it is possible to record images along any axis, and so regions such as the outflow tract, which are hard to visualize with other techniques, can be assessed with great precision.
In 48% of the patients in our study population, diagnosis of ARVD could be ruled out by cardiac MRI. This is because all patients with diagnostic criteria for ARVD have RV structural or functional abnormalities potentially detectable by cardiac MRI. It is important to note that, in accordance with our results, the presence of fatty infiltration on its own does not imply diagnosis of ARVD--the finding has to be associated with other RV structural abnormalities or RV wall motion abnormalities.
Comparison of echocardiography and cardiac MRI as techniques for studying ARVD shows that both can be useful for early diagnosis of ARVD, although a more precise and complete structural and functional assessment of the RV can be obtained with cardiac MRI, and so fewer additional tests are needed.
Structural and Functional Abnormalities of the Right Ventricle
In this study, the most common findings among the 5 patients who met the diagnostic criteria for ARVD were RV wall motion abnormalities (5/5), regardless of whether RV intramyocardial fatty infiltration was present (Table 3). Furthermore, and in accordance with other studies that have been published,17 cardiac MRI was able to detect RV dilatation in patients with ARVD.
Value for Detecting Intramyocardial Fat
With cardiac MRI, the presence of RV intramyocardial fatty infiltration can be detected noninvasively.9,10,17-20 However, fatty infiltration alone does not allow definitive diagnosis of ARVD. Indeed, several studies have shown that RV fatty infiltration occurs in a high proportion of healthy people, particularly elderly subjects.21-23 In our study population, 9 of the 46 patients studied by cardiac MRI presented RV fatty infiltration. This finding was the only diagnostic criterion identified in 6 of these patients, none of which belonged to the group diagnosed with ARVD. Similarly, after excluding the 5 patients diagnosed with ARVD, 14% of the patients studied (6/41) had RV fatty infiltration of indeterminate clinical significance--it might have corresponded either to a variant of normality or to the disease in its early stages such that the patients did not as yet meet the required diagnostic criteria. Given the low number of patients in this study and the lack of follow-up, we cannot say with any certainty which is the case. Several authors have reported a diagnostic sensitivity of RV fatty infiltration in patients with ARVD of between 11% and 100%, suggesting to us that this question should be studied in more detail.9,17,24 In agreement with results published in the medical literature,17,20 we found a sensitivity of 60% (3/5) for the presence of RV fatty infiltration in the diagnosis of ARVD. We should highlight that the presence of fatty infiltration in our population was associated with RV structural abnormalities or RV wall motion abnormalities in all patients diagnosed with ARVD.
Some studies suggest that the findings of studies of fatty infiltration vary greatly from observer to observer,25,26 therefore diagnosis should be done carefully by experts to avoid erroneous diagnosis of ARVD, particularly as fatty infiltration is a major criterion. Fat-suppressed sequences may be useful for confirming diagnosis in doubtful cases. Diagnosis of ARVD should always be made according to the criteria proposed by the European Society of Cardiology (Table 1) and never according to the findings from a single test such as cardiac MRI in this case.13 This approach avoids repeated erroneous diagnosis of ARVD due to lax application of established diagnostic criteria.26
Cardiac Magnetic Resonance Imaging Versus Echocardiography
Comparison of the usefulness of echocardiography and cardiac MRI for diagnosis of ARVD shows that both techniques are equally sensitive for identifying patients with RV disease. Cardiac MRI can, however, detect a greater number of RV pathological abnormalities, particularly those corresponding to major diagnostic criteria, and so diagnosis of ARVD is pos sible in a larger number of patients. Thus, of the 4 patients diagnosed with ARVD who were studied by both techniques, 2 would not have been diagnosed with ARVD if only the echocardiographic findings had been considered (Table 4). However, it is important to highlight that some sort of abnormality in RV function is observed by echocardiography in all patients diagnosed with ARVD, and so the technique could be important for early detection of the disease. Nevertheless, given the lower diagnostic value of echocardiography, cardiac MRI should be considered when clinical suspicion is strong, even though the echocardiographic findings for the RV are normal.
Limitations
The main limitations of this study are the low number of patients and cross-sectional design of the study with retrospective data collection. Furthermore, inter- and intraobserver variability was not analyzed. Ventriculography and RV biopsy are considered the gold standard for diagnosis of ARVD, but the patients in this study did not undergo these invasive techniques (at the time, angiography and biopsy were not recommended to confirm diagnosis of ARVD).20 In our opinion, however, this limitation is not of overriding importance because studies have been published that show a good correlation between findings of cardiac MRI and ventriculography for study of the RV.9 Likewise, the lack of biopsies should not be considered an important limitation when assessing the results as there is not always a good correlation between detection of fatty infiltration by cardiac MRI and by biopsy.20 A couple of explanations for this are possible. First, the region most affected by myocardial degeneration and fatty infiltration is the so-called "triangle of dysplasia," formed by the outflow tract, the apex, and the inferobasal region of the RV wall (subtricuspid region), whereas biopsies are normally taken from the apical part of the ventricular septum in order to minimize the risk of perforation. Second, biopsy samples are taken from random sites, which may or may not coincide with a region of fatty infiltration.
In addition, a possible relationship between the finding of intramyocardial fat and the course of the disease cannot be ruled out without follow-up, and so conclusions on the prognostic usefulness of the finding cannot be drawn.
Double inversion-recovery fat-suppressed fast spin-echo (SE) MRI can detect fatty infiltration of the RV when 30% to 40% of the myocardial thickness is affected,20 but fat-suppressed images were not recorded systematically for confirmation in our study. The operators often did not consider fat-suppressed SE MRI necessary, particularly in the case of patients studied with the Siemens Magnetom because of the excellent spatial resolution of the SE T1-weighted sequences obtained with this unit.
CONCLUSIONS
Diagnosis of ARVD is complex and cannot be unequivocally established with a single test and so a series of internationally accepted major and minor criteria have to be evaluated.
Among the imaging techniques used, cardiac MRI stands out because of the quality of information obtained. In our study, RV structure and function of patients with suspected ARVD could be accurately assessed with cardiac MRI, thus avoiding the need for angiography or biopsy, which are still considered the gold standards, despite their limitations.
Even though echocardiography and cardiac MRI were equally sensitive for identifying patients with RV structural or functional abnormalities, the diagnostic benefit of cardiac MRI was greater, as ARVD could be diagnosed in a larger number of patients thanks to the identification of more diagnostic criteria.
Correspondence: Dr. F. Carreras.
Servicio de Cardiología. Hospital de Sant Pau.
Sant Antoni M.a Claret, 167. 08025 Barcelona. España.
E-mail: fcarreras@santpau.es