Keywords
INTRODUCTION
Neurological complications (NC) are a major cause of morbidity and mortality during the immediate postoperative period following cardiac surgery. They add to the consumption of health care resources and lead to functional limitations in surviving patients. The understanding of their etiology, pathogenesis, prevention, and management on the part of the clinicians who treat patients who develop these complications is under constant development. A number of studies have demonstrated an incidence of ischemic stroke with motor deficit ranging between 2% and 6% among patients who have undergone myocardial revascularization, with even higher rates following valve replacement.1-5 The proposed etiologic and pathogenic mechanisms include perioperative embolism originating in the cardiac chambers or aorta, systemic hypoperfusion or a combination of these 2 processes. Several risk factors associated with stroke have been identified, in particular, age over 75 years, diabetes, hypertension, congestive heart failure, recent myocardial infarction, prior stroke, carotid disease, chronic renal failure, low cardiac output, the need for balloon counterpulsation, prolonged ventilation, and atrial fibrillation.6
Aside from stroke, differing degrees of decrease in the level of consciousness (which we will refer to as encephalopathy), a more or less evident deterioration in neuropsychological function and convulsive seizures may be observed during the immediate postoperative period following cardiac surgery. Up to 10% of the patients present encephalopathy, which can range from prolonged emergence, confusion or stupor with no focal motor deficit, to a state of prolonged cognitive deterioration.7 Among the etiologic factors involved in these conditions, cerebral microemboli, cerebral edema, hypoperfusion, cerebral hypoxia and the effects of pharmacological agents utilized in anesthesia and during the perioperative period have been considered.
The diagnosis and prognostic evaluation of these complications involves the use of brain neuroimaging studies. Until recently, these studies have added little to the understanding of the pathogenesis of the neurological dysfunction; cranial computed tomography (CT) is employed to rule out hemorrhagic lesions but, in stroke, it is only useful in those cases involving a large cerebral artery (which suggests an embolic event as the cause). In contrast, brain magnetic resonance imaging (MRI), a more sensitive technique, has revealed lesions in up to a third of the patients who have undergone surgery, although in some of the few studies published in the medical literature, there is no correlation between the anatomical lesion encountered and the clinical features.
In this report, we describe the NC in a surgical series and analyze the neuroimaging studies performed and discuss the value of brain MRI in patients presenting a focal motor deficit or postoperative encephalopathy in whom cranial CT failed to substantiate the clinical signs.
MATERIALS AND METHODS
We describe the NC that develop during the immediate postoperative period and their course in a series of patients who had undergone cardiac surgery--with cardiopulmonary bypass (CPB)--in our center between 1 May 2002 and 31 December 2003. We analyze the value of brain MRI, using T1-weighted, T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences in patients with postoperative stroke or encephalopathy in whom CT scanning revealed no abnormalities substantiating their clinical condition. The data was collected prospectively.
The anesthetic technique was similar in all the patients. Pulsatile CPB at a flow rate of 2.4 to 4.8 L/min/m2 was established using a roller pump (Sarns® 9000). Hypothermia was maintained between 28ºC and 32ºC, except in those cases in which circulatory arrest was required, in which it was reduced to 18ºC.
Selected information was collected from the clinical histories and from a specific database. The incidence, clinical features and presentation of the NC were analyzed. The procedure-related variables analyzed were the type of surgery and the duration of CPB, aortic cross-clamping (ACC), and circulatory arrest, when the latter was necessary. The postoperative course was also analyzed. The patients with and without NC were compared in terms of the hours of mechanical ventilation required and the number of days spent in the intensive care unit (ICU), and their clinical condition on discharge from the ICU and the hospital was analyzed.
After a systematic neurological examination, stroke was defined as a motor-sensory deficit localized to a focal region of the brain, with or without a decreased levels of consciousness, and encephalopathy as a decrease or fluctuations in the level of consciousness, with cognitive deterioration, in the absence of focal motor deficits, after recovery from anesthesia. These definitions are adaptations of those accepted by the Society of Thoracic Surgeons.8
With the exception of 1 patient, who presented partial convulsive seizures, and 6 with mildly decreased levels of consciousness and rapid recovery, all the patients underwent initial cranial CT within the first 48 hours after surgery, mainly to rule out the presence of intracranial hemorrhage. In those cases in which clinical neurological changes persisted and the initial CT was not diagnostic, the scan was repeated using conventional helical CT (HiSpeed ZX/i, GE Medical Systems).
On the basis of the hypothesis that brain MRI may be more sensitive in identifying small ischemic lesions that are not detected by CT, but that substantiate the clinical condition of the patients, in those with focal motor-sensory deficits and CT findings (initial and follow-up) that did not explain their clinical condition, MRI was also performed, using T1-weighted, T2-weighted and FLAIR sequences in the 3 orthogonal planes (1.5 T Signa scanner, GE Medical Systems). Brain MRI was also carried out in 7 patients with clinical signs of encephalopathy, severe in 3 cases, in whom CT revealed nothing abnormal. All the neuroimaging studies were analyzed by an expert neuroradiologist.
Although MRI can be performed safely in patients with temporary epicardial pacemaker leads, cut short at the skin,9 in our series, it was carried out after they had been withdrawn.
The statistical analysis consisted in calculating the means and standard deviations of the descriptive data for the series. In the categorical variables corresponding to the postoperative period in which the group of patients who developed NC was compared with the group that did not, Student's t test and Fisher's test were used, while the quantitative variables were compared by analysis of variance. Statistical significance was set at P<.05. The analysis was carried out with the SPSS statistical software package, version 8.0.
RESULTS
Of the 688 consecutive patients undergoing cardiac surgery with CPB in our center, a total of 57 developed NC during the immediate postoperative period, for an incidence of 8.3%. The mean age of the group of patients was 65.8±11.3 years (range, 37-83 years); 51% were women. The surgical intervention was carried out as illustrated in Figure 1. The procedures involved a mean CPB time of 122±54 minutes, a mean ACC time of 92±43 minutes and, in 4 patients, circulatory arrest (mean duration, 53.5 minutes).
Figure 1. Surgical procedures performed. Valve indicates valve replacements (aortic, mitral, or both); aorta, procedures in aorta (3 valved conduits with coronary reimplantation and 4 supracoronary conduit interpositions); coronary artery bypass grafting (CABG), coronary revascularization; others, 1 heart transplantation, closure of 1 atrial septal defect, 2 pulmonary endarterectomies, and implantation of 1 pulsatile left ventricular assist device.
The NC presented clinically as stroke in 25 patients, corresponding to 3.6% of the overall group, and as encephalopathy in 24 (3.5%). Although the majority involved mild cases of prolonged emergence, self-limited delirium or agitation which were corrected within the first 48 postoperative hours, 3 patients presented prolonged severe encephalopathy. Seizures were observed in 20 patients (2.9%), 5 of whom presented isolated seizures; in the remainder, they were associated with stroke or encephalopathy, brain death (2 cases, 0.29%) and posterior fossa hematoma (1 case, 0.15%).
In this group of patients, there was a high incidence of other postoperative complications, such as left ventricular failure (44%), perioperative myocardial infarction (12%) and atrial fibrillation (54%). The length of time elapsed before weaning from mechanical ventilation and extubation (106.8±210.4 hours) and the ICU stays of these patients (10.4±15.4 days) were longer than those of the group that did not develop NC (thus entailing a greater utilization of resources). The period of mechanical ventilation, the ICU stay and the mortality in the 2 groups are compared in Figure 2. Five patients died in the ICU: the 2 in whom brain death had been diagnosed (secondary to hypoperfusion and cerebral edema due to low cardiac output in the context of preoperative cardiogenic shock in 1 patient and to circulatory arrest in the other) and another 3 whose deaths were not related to the neurological problem.
Figure 2. Overall course during ICU stay. Comparison of patients who presented NC with those who did not. ICU indicates intensive care unit; MV, mechanical ventilation; NC, neurological complication.
It is noteworthy that, except in 1 case of persistent vegetative state, clinical improvement was observed in the remaining NC in terms of level of consciousness and partial or total recovery of mobility by the time the patients left the ICU. At hospital discharge, all the patients showed a marked recovery of mobility and were capable of performing their usual activities on their own. Only 5 presented motor sequelae (mild monoparesis or hemiparesis).
The initial CT study was performed during the first 48 hours in 50 patients. Only 1 study revealed the presence of cerebral hemorrhage, despite the potential risk associated with the high-dose anticoagulant therapy that these patients require during the surgical procedure and the coagulopathy secondary to the use of a CPB circuit. In this first study, relevant findings that would substantiate the clinical condition were not detected in 35 patients (70%). In 23 of these patients, the clinical neurological signs persisted more than 24 hours and follow-up CT was carried out (7 to 10 days later, either in the ICU or the hospital ward) to search for possible ischemic lesions. Five of the studies revealed ischemic regions consistent with the clinical condition; as the remaining 18 were nondiagnostic, brain MRI was performed. In 11 of these patients, the images revealed the presence of a focal motor deficit; in all but 1 of these cases (corresponding to an individual who, at the clinical level, presented only transient mixed dysphasia), MRI showed areas of acute or subacute infarction at different sites; they were mainly small lesions, distributed in watershed territories, that could explain the clinical findings (Table 1). These images exhibited hyperintense signal on T2-weighted and FLAIR sequences. MRI was also performed in 4 patients with mild-to-moderate encephalopathy in whom CT revealed no radiological abnormalities. One of these studies showed no significant changes but, in the other 3, lesions similar to those described above in stroke patients were observed, with hyperintense signal suggestive of acute or subacute infarctions. Finally, MRI was carried out in 3 patients with clinical signs of severe encephalopathy and coma lasting more than 48 hours. The studies revealed multiple areas of infarction at the cortical level, that appeared to indicate an overall hyperintense signal in cortex, with edema of the gyri. Figures 3 and 4 present MRI corresponding to patients with postoperative stroke in whom CT scans had been normal. Figure 5 shows the MRI results in a patient who exhibited prolonged emergence and subsequent decreased level of consciousness lasting approximately 36 hours, in whom brain CT had demonstrated nothing remarkable.
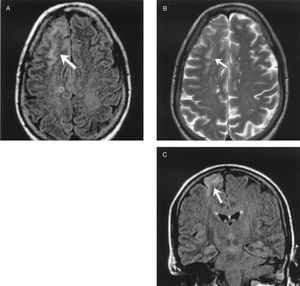
Figure 3. Patient subjected to aortic valve replacement. Left hemiparesis and decreased level of consciousness. Two cranial computed tomography scans revealing no abnormalities. Brain magnetic resonance shows a hyperintense lesion in right frontoparietal region in T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences.
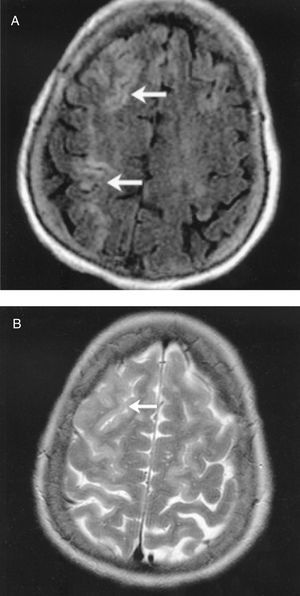
Figure 4. Patient who underwent mitral valve replacement. Left hemiparesis. Cranial computed tomography scans revealed no abnormalities. Brain magnetic resonance shows a hyperintense lesions in right frontoparietal region in T2-weighted and fluid-attenuated inversion recovery (FLAIR) sequences.
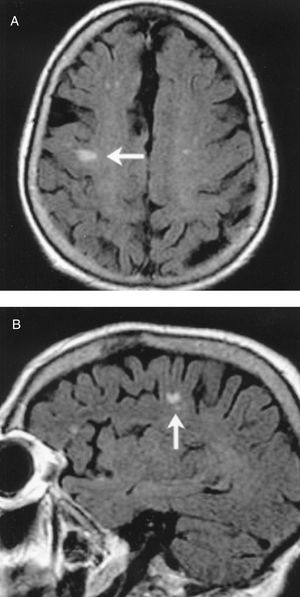
Figure 5. Patient subjected to aortic valve replacement and coronary revascularization. Prolonged emergence from anesthesia and subsequent decreased level of consciousness lasting approximately 36 hours. Cranial computed tomography scans revealed no abnormalities. Brain magnetic resonance shows a small lesion with well-defined margins in right parietal region.
DISCUSSION
During the immediate postoperative period following cardiac surgery, several types of central nervous system lesions or dysfunctions can be observed. The incidence of transient neurological deficits, according to different authors, ranges between 7% and 61% and that of permanent deficits between 1.6% and 23%,3,10 depending on the type of study (prospective or retrospective), the definitions, the complementary tests utilized and the variables analyzed.8 Clinicians have yet to fully understand the etiology, pathogenesis and clinical course of these lesions. The studies performed appear to demonstrate that cerebral infarction, or ischemic stroke, is secondary to small emboli originating in the cardiac chambers or the CPB circuit, or to particles from the atheromatous plaques in the aortic arch. This embolic material, combined with the attenuation of the "washout" phenomenon due to cerebral hypoperfusion, may provoke the ischemic lesions, mainly distributed peripherally in watershed areas.11,12 The lesions can be bilateral in 25% to 65% of cases. Other mechanisms proposed to explain the cerebral dysfunction include the development of postoperative cerebral edema, the activation of the inflammatory cascade14 and gaseous microemboli or microemboli formed by lipid particles. Moody et al15 observed dilation of cerebral arterioles and capillaries following bypass surgery and demonstrated that it was due to microscopic emboli, the composition of which could not be fully identified. On the other hand, the development of postoperative encephalopathy and delirium has been associated with a number of contributing factors, including the adverse effects of the anesthetic drugs, hypotension, ischemic lesions and hypoperfusion, metabolic changes, etc.
To date, neuroimaging studies have added little to the understanding of the pathogenesis and course of the neurological lesions occurring after cardiac surgery. In those cases in which stroke is very clearly involved, CT reveals lesions related to an arterial territory, a fact that suggests an embolic phenomenon. Salazar et al16 found CT evidence of stroke in 72% of their cases; but, on many occasions, the CT scan is not indicative of radiological changes in patients with clinical signs of monoparesis or hemiparesis or presenting decreases in the level of consciousness of varying degrees. Now, however, in addition to the fact that MRI is a technique that does not expose the patient to ionizing radiation, it offers a higher anatomical resolution, with greater sensitivity for small ischemic lesions. Conventional MRI techniques revealed new ischemic lesions in up to one third of the patients in which it was performed prior to and after cardiac surgery.17 Moreover, diffusion-weighted MRI detects ischemic lesions in very early phases and enables the differentiation between acute and chronic ischemia.18 Sellman et al19 studied 29 patients before and after coronary revascularization. They point out that, in the preoperative study, 59% had age-related hyperintense focal white matter lesions on T2-weighted images that remained unchanged in the postoperative study. As new findings in the immediate postoperative period, they reported 2 cerebral infarctions. Toner et al20 described 4 patients (27%) with lesions related to the neuropsychological deficits that were observed on MRI 1 week after surgery and concluded that there was a correlation between cerebral structural lesions and postoperative brain function. Vanninen et al21 studied the results of MRI performed before and after revascularization surgery in 38 patients and compared the results with a group of 20 control patients who had undergone vascular surgery. The postoperative MRI study revealed new small ischemic lesions in 8 patients in the cardiac surgery group, whereas there were no new lesions in the control group. Khon also found new focal lesions that correlated with the clinical findings on MRI carried out after revascularization.
On the basis of the limited experience published in the medical literature, and assuming that cerebral structural changes that explain the cerebral dysfunction and clinical course of these patients can be detected postoperatively (although they may not be sufficiently evident to be diagnosed by means of CT), we selected a group of patients with neurological deterioration in whom, moreover, CT revealed nothing to substantiate it. In this group, 16 of the 18 MRI studies showed ischemic lesions that correlated with the clinical signs. The most significant finding was the demonstration of ischemic lesions not only in the patients that presented the clinical features of focal motor deficit, but in 3 of 4 patients with mild-to-moderate encephalopathy. The presence of structural lesions in these conditions is of interest since it indicates that the clinical signs are not only explained by the functional impact of the surgical procedure. The size and distribution of these postoperative lesions suggest that the pathogenic mechanism would be small emboli in distal cerebral arterial territories. Similar to the findings reported in the medical literature, a high percentage of our patients presented preoperative lesions, probably related to age and cardiovascular risk factors, that affect the cerebral vessels.
In contrast to our observations, some studies involving MRI, such as those carried out in small numbers of patients by Schmidt et al23 and by Simonson et al,24 have reported the failure to detect the brain lesion causing the postoperative encephalopathy.
Diffusion-weighted MRI studies present a greater sensitivity for the early detection of acute ischemic changes in the tissues.18,25,26 Wityk et al27 observed images of acute infarction in 10 of 14 patients following cardiac surgery (whereas only 5 cases were detected by cranial CT).
Recently, Bendszus et al28 reported new infarctions in 26% of the diffusion-weighted MRI studies performed early in the postoperative period in 35 patients who had undergone myocardial revascularization. In contrast, Anderson et al29 found no focal ischemic changes in any of the 17 patients studied after revascularization, although they did observe changes consistent with an increase in brain extracellular water.
The importance of our findings lies in the demonstration of the existence of ischemic brain lesions that aid the clinician that manages these patients to understand the development and course of these complications; in addition, this may help in the design of prevention measures. Nonetheless, we are aware of the limitations of the study, mainly, the need to increase the number of patients studied, if possible, including collaboration with other centers and a longer follow-up period. Although we did not perform diffusion-weighted MRI in our patients, the ischemic lesions detected with conventional MRI, in the sequences used, were clearly visualized. Moreover, they correlated with the clinical findings, despite the fact that they were not visible in the CT studies. On the other hand, the only advantage is the early detection of the ischemic lesion, a measure that we do not consider indispensable. In the majority of cases, transporting a patient for the performance of a lengthy imaging study during the immediate postoperative period entails considerable risk, and the possible findings are not followed by an immediate change in the therapeutic approach.
In short, in our series, the results of which are similar to those published elsewhere, we observed that the incidence of NC during the postoperative period following cardiac surgery was relatively high and that they occurred more frequently in patients subjected to valve or aortic replacement. The low incidence of intracranial hemorrhage is noteworthy. Brain CT may not reveal existing lesions in a high percentage of cases. In selected patients, MRI, in the sequences used, is more sensitive and can result in findings of interest, showing ischemic areas that aid in the understanding of the etiology, pathogenesis, pathophysiology, clinical features and course of these neurological deficits. The understanding of the etiology and pathogenesis alone can serve as a basis for the design of effective prevention strategies.
In any case, studies of the neurological dysfunction occurring after cardiac surgery are limited by the difficulties in recruiting large, homogeneous series to ensure the robustness of the results, as well as the difficulties in defining the events and quantifying the encephalopathy and cognitive deterioration, the differences in the results of the application of the diagnostic techniques and the evaluation of the possible interventions (technical or pharmacological) aimed at the prevention of NC. The establishment of standardized definitions of the events and systematized diagnostic management, and the development of multicenter studies that would ensure a large number of patients, would aid in the design of effective prevention strategies.
Correspondence: Dr. J.L. Pérez-Vela.
Atardecer, 3. 28223 Pozuelo de Alarcón. Madrid. España.
E-mail: perezvela@yahoo.es