Keywords
INTRODUCTION
Scimitar syndrome is characterized by an anomalous connection of the right pulmonary veins to the suprahepatic portion of the inferior vena cava or to the right atrium above the junction with this vein. Associated anomalies include dextroposition of the heart due to dextrorotation, hypoplasia of the right lung, hypoplasia of the right pulmonary artery, systemic anomalies of the right lung arterial irrigation (aortopulmonary collateral arteries that can cause a left-to-right shunt), bronchopulmonary sequestration with agenesis of the upper right or middle bronchus, as well as other extracardiac and cardiac anomalies. Twenty-five percent of patients present cardiac malformations, with the most frequent being an atrial septal defect.1-4
The presumptive diagnosis is made on radiographic findings. Echocardiography allows identification of the anomalous drainage of the right pulmonary veins toward the curved collector, the presence of obstructions, and the connection site in the suprahepatic portion of the inferior vena cava. The transthoracic technique has diagnostic limitations in up to 33% of cases; hence, it is important to perform a transesophageal study as well.5,6 The interest of this report lies in the fact that cases reported among the adult population are rare.
The aim of this study is to report the clinical and echocardiographic findings in a series of 7 adult patients with scimitar syndrome, examined at the Instituto Nacional de Cardiología Ignacio Chávez from 1985 to June 2004.
PATIENTS AND METHODS
This retrospective study included 7 women with a diagnosis of scimitar syndrome examined in an adult congenital heart disease clinic. A complete clinical history, chest x-ray, transthoracic and transesophageal echocardiography, as well as left and right cardiac catheterization were performed in all patients. In 2 patients, computed tomography scanning was done to determine the site of connection of the right pulmonary veins and exclude the possibility of bronchiectasis or pulmonary hypoplasia. Three patients underwent magnetic resonance imaging, in 2 cases to define the type of connection and in 1 case to determine the site of obstruction in a tube placed during surgery.
The echocardiographic study was performed with Philips Sonos 1000 and 5500 systems, using a 2.5-mHz transthoracic probe, and biplane and multiplane transesophageal probes. Previously described specific and non-specific echocardiographic features were used for the analysis.4,6 The diameters of the pulmonary artery and branches were determined in the parasternal slice in both arteries. Apical and subcostal four-chamber sections obtained by two-dimensional transthoracic echocardiography were used to assess the characteristics of the atrial septal defect, pulmonary vein connections, inferior vena cava drainage, presence of obstruction in the venous collector, and dilation of the right chambers, and to detect aortopulmonary collateral vessels. Using continuous wave color Doppler in an apical four-chamber view, the sample volume was placed at the height of the tricuspid valve and the pressure gradient between the right atrium and ventricle was determined using Bernoulli's method. The result was multiplied by a correction factor of 1.23 to obtain the pulmonary artery systolic pressure.
With the use of a four-chamber transesophageal technique, the size and location of the atrial septal defect, the manner in which the pulmonary veins were connected, and the repercussion on the right chambers were assessed. The pulmonary artery diameter was measured in the 70º longitudinal section and the pulmonary branches in the 0º section. Arterial hypoplasia was defined as a diameter of <18 mm for the pulmonary artery and <10 mm for the pulmonary artery branches.6
RESULTS
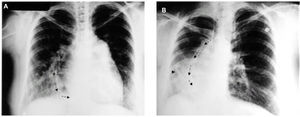
The patients' demographic characteristics are shown in Table 1. The most frequent symptoms were respiratory manifestations (chronic cough, decreased exercise tolerance, to exercise, and recurrent respiratory tract infection) and progressive dyspnea on heavy and moderate exertion in 90% of the cases. The scimitar sign was seen on the chest x-rays in 4 patients (57%) (Figure 1 A and B).
Figure 1. A: anteroposterior chest x-ray showing curved course of the collector (arrows), grade II cardiomegaly with bulging of the right pulmonary artery branch and mild hypoplasia of the lower lobe of the right lung. B: chest plain film showing dextrorotation of the heart and hypoplasia of the lower and middle lobes of the right lung. Arrows show the curved course of the collector. Arrowhead indicates an aortopulmonary collateral vessel.
The transthoracic and transesophageal echocardiographic studies allowed the diagnosis to be established in 86% of the cases. The cardiac anomalies encountered are shown in Table 2. Five patients had dextrocardia, 5 dilation of the right chambers and hypoplasia of the pulmonary arteries and branches, and 5 "blunting" of the right side of the atrium (absence of right pulmonary veins draining to the left atrium).
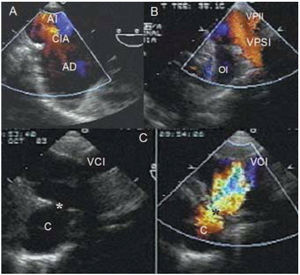
The site of the pulmonary venous connection was determined by color Doppler: in 2 patients it was found in the lower portion of the right atrium, in 2 others in the inferior vena cava through a venous collector, and in the remaining 3 patients at the junction of the right atrium with the inferior vena cava. Three patients showed narrowing of the collector at the site where it connected with the inferior vena cava (Figure 2 A-D) (Table 3).
Figure 2. A: transesophageal echocardiogram with color Doppler showing the interatrial shunt. B: transesophageal color Doppler echocardiogram depicting the left pulmonary veins draining to the left atrium above the auricular appendage. C: two-dimensional and color Doppler images show turbulent flow in the collector, which drains at the site of the junction of the inferior vena cava and the right atrium. RA indicates right atrium; LA, left atrium; C, collector; IAC, interatrial communication; RD, right ventricle; LV, left ventricle; LAA, left auricular appendage; IVC, inferior vena cava; PV, pulmonary vein; ILPV, inferior left pulmonary vein; SLPV, superior left pulmonary vein. *Site of collector obstruction.
The echocardiographic diagnosis showed close agreement with the findings obtained by cardiac catheterization (Figure 3), and catheterization allowed assessment of the aortopulmonary collateral circulation observed in one case.
Figure 3. Angiographic study showing the curved course of the collector (arrows).
Six patients underwent surgery to correct the associated cardiac anomaly and place a bypass from the right pulmonary veins to the left atrium. In only one of these patients, reimplantation of the right pulmonary veins to the left atrium was performed in a second surgical stage. One patient was reoperated for significant obstruction of the tube placed for the reimplantation.
The remaining patient had a small atrial septal defect and was in NYHA functional class I; hence, surgery was not performed (Table 2).
All the patients who underwent surgery were in functional class I at the time of writing.
DISCUSSION
Scimitar syndrome is divided into 3 groups according to the age of the patients, as defined in a multicenter study involving 122 patients aged 1 to 58 years. Group I comprises the adult form, which shows no pulmonary artery hypertension (PAH) and involves a small septal defect; it is the best tolerated, as was seen in one of our patients. Group II is characterized by an association with complex congenital abnormalities that modify the symptoms and natural history of the syndrome; the remaining patients in our series fell into this category. Group III is the infantile form and is characterized by severe PAH and a poor prognosis.2,4,5,7
The most common symptoms, respiratory manifestations and progressive dyspnea,4,5,8 were present in all our patients. In some cases the scimitar sign is not observed because of cardiac dextrorotation or because the venous collector is not wide or curved, but instead, straight, thin or multiple. This sign presents in 70%, generally because right lung hypoplasia is absent in adults.1,2
The echocardiographic diagnosis correlated well with the cardiac catheterization findings. Transthoracic echocardiography has greater value in children with scimitar syndrome, whereas in adults transesophageal echocardiography should also be performed to assess the posterior structures, such as the atrial septum to determine the size, number, morphology, and location of defects as well as the pulmonary vein connections, which cannot be well-assessed with the transthoracic technique. Transesophageal echocardiography is also useful for detecting obstruction of the tubes placed for reimplantation, as occurred in one of the cases studied, which was confirmed by magnetic resonance imaging.2,4,6,7 It is very important to determine the subdiaphragmatic areas of connection for better surgical treatment. A surgical alternative would be to reimplant the collector at the posterior wall of the left atrium with off-pump circulation.5,8-10
On the basis of our study, we conclude that scimitar syndrome is rare and the diagnosis is established by echocardiography in most cases. With the development of non-invasive techniques,11,12 the diagnosis is complemented by cardiac catheterization only in some cases.
Correspondence: Dra. N. Espinola Zavaleta.
Departamento de Ecocardiografía.
Instituto Nacional de Cardiología Ignacio Chávez.
Juan Badiano, 1. Colonia Sección XVI. Tlalpan 14080. México, DF.
E-mail: niesza2001@hotmail.com
Received September 16, 2004.
Accepted for publication June 10, 2005.