Keywords
INTRODUCTION
Measurement of the carotid intima-media thickness (CIMT) with ultrasound can detect thickening of the artery wall during the initial phases of atherosclerosis before the lumens become compromised.1 It has been shown that CIMT bears a relation to the incidence and prevalence of atherosclerosis in all its clinical forms2-4 and cardiovascular risk factors are predictors of CIMT.5 Likewise, it has been seen that CIMT regresses after pharmacological treatment for different cardiovascular risk factors.6 Therefore, CIMT is considered a surrogate marker of cardiovascular disease, an independent risk factor, and a tool for early detection of atherosclerosis.1
The main objective of the study was to determine the average and maximum CIMT in the 3 best studied segments of the carotid arteries in atherosclerosis— common carotid artery (CCA), carotid sinus (CS), and internal carotid artery (ICA)—in a population with no known cardiovascular risk factors, to serve as a reference for normal CIMT and also to identify patients with greater atherosclerosis in our population. The secondary objective was to study factors determining CIMT in individuals without any traditional cardiovascular risk factors.
METHODS
Between January 2006 and June 2008, 218 subjects were recruited from among staff of the Hospital Universitario Miguel Servet, Zaragoza, Spain, and staff and students of the University of Zaragoza, Spain, with the Faculty of Medicine particularly strongly represented, and the "University of Experience" training program aimed at individuals aged over 60 years. The objective was to obtain a sample that included at least 10 men and 10 women in each of 6 preestablished age groups between 18 and 80 years. The inclusion criteria were no personal history of cardiovascular disease, no premature cardiovascular disease in first-degree relatives, cigarette consumption less than 15 pack- years (number of cigarettes smoked per day in packs, multiplied by the number of years of smoking), no diagnosis of dyslipidemia, arterial hypertension, or diabetes mellitus, and no serious illness requiring admission to hospital in the past year. Written informed consent was obtained from each participant according to the protocol approved by the ethics committee of our hospital.
The clinical and laboratory data collected are presented in Table 1. The procedure for obtaining these data has been described previously.7
Measurement of CIMT was performed in the posterior wall of both carotid arteries by mode B ultrasound with an Acuson Sequoia ultrasonography device equipped with a linear 8 cm probe operating at 8 MHz. Images of 6 territories were taken: final centimeter of the CCA, the CS, and the first centimeter of the ICA on both sides.1 A single investigator (AMB), accredited by the vascular imaging laboratory of the Academic Medical Center of Amsterdam, the Netherlands, took the readings using eTRACK1 dedicated software.
Subjects with a BMI >30, blood pressure >160/90 mm Hg, low-density lipoprotein cholesterol (LDL-C) >160 mg/dL, high-density lipoprotein cholesterol (HDL-C) <30 mg/dL, triglycerides >200 mg/dL, blood glucose >125 mg/dL, creatinine >2 mg/dL, or thyrotropin >6 µU/mL were excluded.
Continuous variables with a normal distribution were expressed as means (SD) whereas those without a normal distribution were expressed as median [interquartile range]. The difference in mean values between men and women was tested using the Student t test or the Mann-Whitney U test. Analysis of variance was used to test the differences in means between CCA, CS, and ICA. To determine which variables were predictive of CIMT, a multivariate linear regression model was used. A general linear model was used to fit the values to the variables independently associated with CIMT.
RESULTS
In total, 221 subjects were selected and 138 were included in the final analysis (64 men and 74 women). Eighty-three subjects (46 men and 37 women) were excluded for the following reasons: 41 for LDL-C >160 mg/dL, 25 for cigarette consumption >15 pack-years, 10 for BMI >30, 10 for arterial blood pressure >160/90 mmHg, and 2 for other reasons.
The clinical, laboratory, and ultrasound variables are presented in Table 1. Men had higher average and maximum CIMT compared to women. The differences between sexes tended to diminish in patients aged over 50 years (Figure 1).
Figure 1. Comparison of the mean maximum carotid intima-media thickness (CIMT) among age groups according to sex.
In men, the upper limit of normal (75 percentile of the distribution) of the average CIMT in the 6 territories ranged from 0.59 mm in those under 25 years to 0.95 mm in those aged over 65 years (Table 2). In subjects aged 25-45 years, this value was 0.66 mm. From 45 years onwards, a noteworthy increase in CIMT was observed. In women, the upper limit of normal for average CIMT ranged from 0.52 mm in those under 25 years to 0.93 mm in those aged over 65 years (Table 2). The upper limits (75 percentile of the distribution) of CIMT of the mean maximum values of the 6 territories by age group ranged from 0.81 mm to 1.11 mm in men and from 0.66 mm to 1.13 mm in women (Table 3). With regard to the study by segments, in all age groups and in both sexes, the highest average and maximum CIMT were recorded in the sinus (Tables 2 and 3).
Age was the main determining factor for carotid thickening of all segments. The average CIMT of the 6 segments was the strongest predictor in the model (adjusted r2 = 0.669). In addition to age (b=.662; P<.001), other predictive variables were male sex (b=.120; P=.027), systolic blood pressure (SBP) (b=.135; P=.029), and LDL-C (b=.131; P=.029). However, HDL-C level was not an independent predictor. For each year of life, an increase in the mean average CIMT of 0.005 mm in the 6 segments was found. For mean maximum CIMT, the increase was 0.008 mm for the 6 segments.
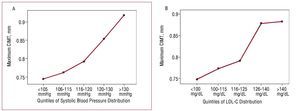
On adjusting the CIMT values for age and sex, a positive association was observed between carotid thickening and SBP levels and LDL-C levels (Figure 2). The increase in CIMT occurred for any increase in SBP, but was more marked above 120 mmHg. A similar situation was observed for LDL-C levels >125 mg/dL.
Figure 2. Estimated marginal means of maximum carotid intima-media thickness (CIMT) adjusted for age, sex, and low-density lipoprotein cholesterol (LDLC) by quintiles of systolic blood pressure (A) and estimated marginal means of maximum CIMT adjusted for age, sex, and systolic blood pressure by quintiles of LDL-C (B).
DISCUSSION
The values obtained allow the distribution of CIMT to be determined in subjects without traditional cardiovascular risk factors. The CIMT in this population is strongly dependent on age and, to a lesser degree, sex, and so we present the values by age group and sex. The study population corresponds, by and large, to a high sociocultural stratum. However, we believe that this bias does not affect the validity of the results. We have chosen as the limit of normal the mean and maximum CIMT values of 6 carotid segments for each age group because this provides a more consistent and complementary information than the data that only use the CCA.2-5 However, we chose the 75 percentile as the upper limit of normal with reference to other population studies.2,4 Our values for normal are within the first 2 quintiles of the CIMT distribution of the Cardiovascular Health Study.3 In the groups in that study, the risk of infarction and stroke was very low (1.1%/year) as subjects were aged over 65 years, with a mean age of 72.5 years. On the other hand, our values are lower than those for subjects who did not develop cardiovascular disease in the ARIC study, which had a similar age distribution to our sample.2 Junyent et al8 studied a group of subjects with a normal lipid profile but, unlike our study, these authors did not exclude subjects with other risk factors and only measured the CCA. The values for CCA in our study were largely in line with their values.8
Age is the main variable related to carotid thickening in all segments, both in men and women, in our study and most studies of the general population.2-5 The changes observed did not follow a linear model. CIMT thickening is more marked from the age of 40 years onwards in men and 50 years onwards in women, in agreement with that observed in other populations.2 SBP and LDL-C are associated much more weakly with CIMT progression, though the association is stronger for SBP above 120 mmHg and LDL-C levels above 125 mg/dL. This reinforces the role of these 2 risk factors, even in the range currently not considered as pathological.
ACKNOWLEDGMENTS
The authors thank Johan Gort and Eric de Groot (Academic Medical Center, Amsterdam, the Netherlands).
FIS: PI06/0365 and RTIC C06/01 (RECAVA), SAF2005-07042 and Professionals With Specialist Healthcare Training (Spanish state bulletin [BOE] July 8, 2005).
Correspondence: Dr. F. Civeira.
Hospital Universitario Miguel Servet.
Avda. Isabel la Católica, 1-3. 50009 Zaragoza. España.
E-mail: civeira@unizar.es
Received December 18, 2008.
Accepted for publication March 23, 2009.