Keywords
INTRODUCTION
Cardiac resynchronization therapy (CRT) has been clinically demonstrated to improve functional class and quality-of-life, reduce hospital admissions and increase survival in patients with heart failure.1
Current guidelines give CRT a class I indication for patients in NYHA functional class III or IV, with QRS complex ≥120 ms and left ventricular ejection fraction (LVEF) £35%.2 However, the vast majority of the >4000 patients included in randomized clinical studies of CRT have cardiomyopathy of ischemic or idiopathic etiology. Little data is available about the usefulness of CRT in heart failure due to other etiologies, like congenital heart disease or valvular heart disease.
The objective of this study is to describe the mid-term (6 months) clinical efficacy and effect of CRT on left ventricular remodeling in patients with advanced heart failure of valvular etiology.
METHOD
We included 40 consecutive patients diagnosed with valvular cardiomyopathy and with classic indications for CRT.
In diagnosing valvular cardiomyopathy, we included patients with a history of mitral valve disease and/or aortic valve surgery, documented previously or post-surgical left ventricular dysfunction, and heart failure with no other obvious etiology. All patients had undergone surgery at least 6 months prior to device implantation and ischemic heart disease had been ruled out by coronary angiography (coronary arteries without angiographic lesions >50%). No patient had a history of myocardial infarction or angina. We excluded patients undergoing surgery for a diagnosis of severe mitral valve failure secondary to mitral ring dilatation due to non-ischemic dilated cardiomyopathy.
At baseline and 6-month follow-up, we recorded the clinical history of all patients and results of physical examination, electrocardiogram (ECG), 6 minute walking test, quality-of-life test (Minnesota Living with Heart Failure Quality of Life Score), echocardiogram, and study of aerobic functional capacity with metabolic analysis of exhaled gases.
By echocardiography, we determined EF using Simpson's rule, ventricular diameters and volumes, E/E' ratio (tissue E wave), aortic flow integral, systolic pulmonary artery pressure (sPAP), Tei index, and parameters of interventricular and ventricular dyssynchrony (septo-posterior and septo-lateral wall delay by tissue Doppler) using previously described techniques.3 Using tissue Doppler, septo-lateral delay was calculated as the difference in milliseconds between QRS complex onset and maximum systolic velocity for each ventricular region on the apical 4-chamber axis.
Patients in atrial fibrillation (AF) were discharged with the right ventricle trigger algorithm activated and at 1 month we checked the percentage of pacing. If it was <85%, we indicated an atrioventricular node (AVN) ablation.
We considered patients non-CRT responders if they met one or more of the following criteria at 6-month follow-up: a) cardiac death; b) inclusion on a heart transplantation waiting list; and c) <10% increase in 6 minute walking test distance.
Numerical results are expressed as mean (SD). Qualitative variables were tested with c2 and quantitative variables with Student's t test. A P value less than .05 was considered significant.
RESULTS
Patient clinical and demographic characteristics are in Table 1.
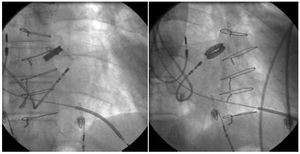
The left ventricular electrode was successfully deployed in 37 (92.5%) patients. Implantation failure was caused by the inability to cannulate the coronary sinus (CS) in 2 patients and the inability to advance the guiding catheter due to the severe angle of the ostium in 1 (Figure 1). Final CS electrode position was lateral region in 22 patients; posterolateral, 8; anterior, 4; and anterolateral, 3.
Figure 1. Severe angle of coronary sinus ostium (2 projections) that prevents the guide catheter from advancing.
Three major complications occurred (8.1%): 1 substantial hematoma, 1 early CS electrode displacement, and 1 transitory ischemic event.
At 6-month follow-up, we considered 31 (83.7%) patients had responded to CRT. Of the 6 non-responders, 2 died of terminal heart failure, and 2 received transplants. Moreover, 5 had sPAP >50 mm Hg. Among those who responded to CRT, 1 died suddenly 4 months after pacemaker implantation.
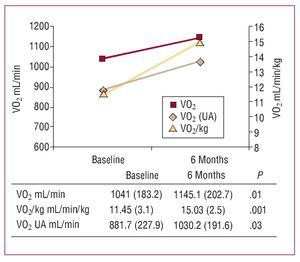
At the end of the follow-up, NYHA functional class (3.2 [0.7] vs 2.1 [0.8]; P=.01), quality-of-life (44 [16] vs 20 [12]; P=.03) and 6 minute walking test distance (244 [119] vs 413 [54] m; P=.001) had improved. The metabolic study identified increased maximum oxygen consumption (Figure 2).
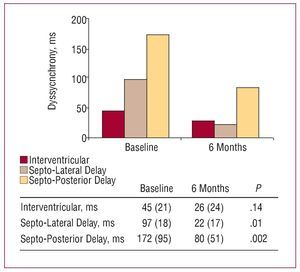
Figure 2. Parameters of interventricular and ventricular dyssynchrony prior to implantation and at 6 months.
Of 20 patients in AF, 7 (35%) underwent AVN ablation. Among patients without ablation, 91% (6%) received pacing. Rates of responders in AF (16/20 patients) and in sinus rhythm (15/17 patients) were 80% and 88.2%, respectively (P=.125).
Effects of CRT on electrocardiographic parameters and parameters of dyssynchrony appear in Table 2 and Figure 3, respectively.
Figure 3. Maximum oxygen consumption obtained at baseline and at the end of the follow-up. AT indicates anaerobic threshold; VO2, oxygen consumption.
DISCUSSION
The present study describes the clinical efficacy of CRT in patients with valvular cardiomyopathy and advanced heart failure, a subpopulation underrepresented in randomized studies, as demonstrated by the CARE-HF study, in which valvular cardiomyopathy was the etiology in only 19 (2%) of 813 patients.4
In valvular heart disease, ventricular dysfunction is generally due to the absence of ventricular remodeling regression after corrective surgery.5 Frequently, behavior disorders develop—often causing mechanical dyssynchrony—and contribute to the situation. However, at present, some aspects of this type of cardiomyopathy— eg, incidence of sudden death or response to resynchronization, which are better defined for other types of cardiomyopathy—remain unknown. The clinical efficacy of CRT in our patients is clearly reflected in improved classical parameters and substantially increased maximum oxygen consumption—a more objective parameter that is less likely to be subject to a hypothetical placebo effect. Moreover, the rate of CRT responders, close to 84%, is in consonance with these findings and similar to that found in patients with idiopathic dilated cardiomyopathy.6 In our study, this also clearly demonstrates the effect of CRT on ventricular remodeling, with improvements in EF and ventricular diameters and volumes, as well as in noninvasive hemodynamic parameters (Tei index, aortic flow integral, and E/E' ratio), comparable to data on CRT in other cardiomyopathies.7
As in earlier studies, parameters of ventricular dyssynchrony became practically normal after device implantation but interventricular delay was not modified. Essentially, this may be explained by the limited interventricular dyssynchrony observed in our patients (45 [21] ms; cutoff at 40 ms), and the lengthened pulmonary preejection period in patients with pulmonary hypertension that is prevalent (87.5%) in our study.8
Finally, our study indicates that management of this subpopulation of patients has its own peculiarities. The greater incidence of AF and substantial atrial dilatation that are usually present can prejudice the implantation success rate.9 However, precise management of antithrombotic treatment is vitally important due to the possible appearance of surgical hematomas and high risk of embolic events that the change of anticoagulants favor.
In conclusion, this study indicates important mid-term beneficial effects derive from CRT both clinically and in terms of ventricular remodeling in patients with advanced heart failure secondary to valvular cardiomyopathy. In the absence of randomized clinical studies, these beneficial effects can be similar to those obtained by CRT in patients with left ventricular dysfunction of other origin.
Correspondence: Dr. I. García-Bolao.
Departamento de Cardiología.
Avda Pío XII, 36. 31008 Pamplona. Navarra. España.
E-mail: igarciab@unav.es
Received November 7, 2007.
Accepted for publication January 9, 2008.