To the Editor,
.
For a doctor, being on call typically involves stress and fatigue associated with moments of anxiety and sleeplessness. Resident physicians (MIR) are on call more than 4 times per month and during those periods may have to work for 24h at a stretch. Several studies have associated being on call with increased cardiovascular risk,1 and alteration in blood pressure (BP) is one of the causal mechanisms.2, 3 Physiological oscillations of a function over 24h are known as the circadian rhythm (CR). Blood pressure decreases during night-time resting.1
Melatonin is the main hormone involved in CR. Its secretion is regulated by the effect of light on the suprachiasmatic nucleus, with darkness stimulating production and light inhibiting it. Studies have shown a relationship between an abnormal pattern of melatonin secretion and alterations in BP.4 The aim of this study was to determine BP values in a population of on call-resident doctors and to investigate their relationship with the pattern of melatonin in urinary secretion.
This was a cohort study carried out in a tertiary hospital with a total of 18 resident doctors. Two BP Holter (Microlife®, WatchBP model) studies were carried out on participants. One was performed on a normal working day to provide baseline measurements and another was performed while residents were on call. Four isolated urine samples were collected: a) morning (8:00) and night (0:00) of the normal working day, and b) morning (8:00) and night (0:00) of the on-call day. Urine samples were analyzed to determine urinary concentrations of 6-hydroxymelatonin sulphate (6-SO4MEL), the urinary metabolite of melatonin. Urinary concentrations of 6-SO4MEL follow the circadian pattern of accumulated melatonin, which correlates with serum melatonin.5 A urine specimen first thing in the morning provides a proportional fraction of nocturnal melatonin production. The CR was defined as normal when 6-SO4MEL concentration was greater in the morning than at night, as production of the hormone increases during the hours of darkness.5 The SPSS 17.0 statistical package (Chicago, Illinois) was used for all statistical analysis. Data with a normal distribution are presented as means ± standard deviations and nonnormally distributed data as medians. Continuous variables were compared using Student's t test or Mann-Whitney U. In all tests, P was considered significant at <.05.
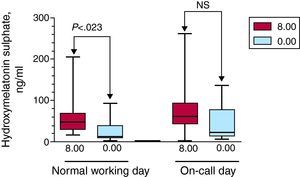
Residents’ mean age was 28±2.1 years. On a normal working day, systolic and diastolic BP decreased significantly between day and night-time readings (119±10.9 and 77±5.4 vs 108±7.6mmHg and 67±6.1, P=.003). Furthermore, 6-SO4MEL values showed that CR was maintained during normal working hours, with concentrations being higher in the morning (8.00) than at night (0.00) (48.6 [28.1 to 74.1] vs 12.4 [7.7 to 38.9] ng/ml, P<.023) (Figure). When samples taken when residents were on call for 24h were analyzed, there were no statistically significant differences between day and night-time values for systolic and diastolic BP (121±9.9 and 81±6.3 vs 116±11.3 and 73±7.3mmHg, P=.08). Analysis of 6-SO4MEL values showed that CR was lost during the on-call work day, with values of 61.2 [43.7 to 89] at 8:00 am compared to 21.2 [14.4 to 75.2] ng/ml at 0:00 pm (P=.08) (Figure).
Figure. Box plot of urine concentrations of 6-hydroxymelatonin sulphate in a population of resident physicians during a normal working day and when on call. Urine samples were collected separately at 2 different times (during daylight hours, at 8:00, and during the hours of darkness, at 0:00). NS, not significant.
This study's novelty lies in its design and the population studied. These were young participants in whom lack of sleep led to a burden of stress and fatigue. The results observed are relevant for 2 reasons. First, we noted that BP, by decreasing at night, followed a circadian pattern on the normal working day, but that this pattern disappeared when participants were on call. Second, the pattern of melatonin secretion indicated a loss of CR during the day on call. Diet would not be relevant to the results as the main factor regulating secretion of melatonin is light.5
Melatonin is involved in regulating biological CRs, including sleep. In our study, the melatonin CR is lost because hyperpolarization of retinal photoreceptor cells occurs in doctors who are awakened for an emergency while on call. This in turn would inhibit the release of noradrenaline and therefore the synthesis and secretion of melatonin.5 The loss of this CR is likely to be at least partly responsible for the abnormal patterns of BP observed. These in turn could lead to increased cardiovascular risk during periods when doctors are on call.
Corresponding author: adrvdg@hotmail.com