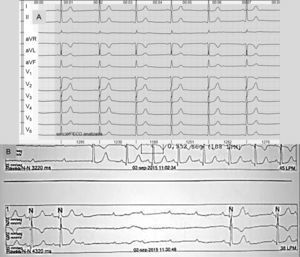
We present the case of a 46-year-old woman whose only cardiovascular risk factor was that she smoked 4 to 6 cannabis cigarettes a day. The patient had no family history of congenital heart disease or ischemic heart disease. She was not taking medications. She attended our center with cardiogenic syncope and associated head trauma, resulting in minor frontal subarachnoid hemorrhage and no progression in the follow-up computed tomography. She was admitted to the cardiology department for study of the syncope. On questioning, the patient reported syncopal episodes from the age of 12 years, all with very similar characteristics, as well as other presyncopal episodes lasting 8 to 10seconds that resolved spontaneously. The examination revealed no remarkable findings. No murmurs or indications of heart failure were detected. The neurological and muscle work-up was entirely normal. The results of chest X-ray and laboratory tests, including screening for systemic diseases and deposits, were also normal. The baseline electrocardiogram on admission (Figure 1A) showed no significant abnormalities, although during heart monitoring (Figure 1B), bursts of third-degree atrioventricular block (AVB) were observed, present both during the day and during the hours of rest, with a maximum duration of up to 10seconds. These correlated clinically with occasional presyncope reported by the patient. Exercise testing (Bruce protocol) was clinically and electrically negative for ischemia; in the second stress stage, third-degree AVB was observed with a 3-second duration. In the transthoracic echocardiogram, slight narrowing of the ventricular septum next to the aortic outflow was observed, measuring 11mm and protruding into the right cavities with no apparent through-flow. The other cardiac structures were normal. The work-up was extended with a transesophageal echocardiogram (Figure 2), which confirmed these findings. The patient was diagnosed with structural heart disease in the form of aneurysmal membranous septum (AMS). This explained the high-degree paroxysmal AVB in the absence of other processes, and a definitive dual-chamber pacing device was implanted. The patient experienced no further syncopal or presyncopal episodes in subsequent follow-up.
A: Baseline electrocardiogram, sinus bradycardia at 48 beats per minute, normal axis, PR normal, narrow QRS with no repolarization abnormality. B: External monitoring, third-degree atrioventricular block with delay of 4320ms and QRS escape of similar morphology to the baseline electrocardiogram.
Transesophageal echocardiogram, 5-chamber view: image showing thinning of ventricular septum (arrow) next to the aorta outflow, measuring 11mm, protruding towards the right ventricle, consistent with membranous septal aneurysm. Ao, aorta; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Membranous ventricular shunts account for three-quarters of all ventricular shunts.1 The membranous septum is located adjacent to the aortic valve and next to the tricuspid valve, just below its septal leaflet. This structure, known as AMS, may sometimes have an accessory tissue that partially or completely occludes the ventricular shunt. It is usually an incidental finding in cardiac magnetic resonance imaging or computed tomography, as shown in the series reported by Choi et al,2 in which 8 cases were reported among 3402 patients studied. Half of those patients with AMS had electrocardiographic abnormalities consistent with minor atrioventricular conduction disorders (first degree) or incomplete right bundle branch block, with no clinical repercussions. The bundle of His follows a subendocardial path along the inferior border of the membranous septum, such that electrical conduction in this region is susceptible to block as a result of the fibrosis component and the turbulence of the blood flow. Thery et al3 reported histological findings in conduction tissue from autopsies in patients with AMS. The authors found a greater degree of atrophy at the bundle of His, which coincided with the region of greatest narrowing of the aneurysm. The atrioventricular node was spared in most cases. In our case, as can be observed in Figures 1A and B, the findings might point to the origin of the AVB lying above the bundle of His; however, an accurate and definitive diagnosis can only be obtained by electrophysiological study. The blood turbulences generated in AMS are more intense during tachycardia, which may explain the burst of AVB observed in our patient during exercise testing.
The association of AMS with sudden death is open to debate. Although cases have been described in the literature,4 they are almost always associated with other congenital heart diseases.
To date, only 5 cases of AMS as a cause of complete AVB requiring pacemaker implantation have been reported5; however, these were detected as already established high-degree irreversible AVB. The complexity and exceptional nature of the present case lay the form of presentation of the syncope and presyncope, with a prolonged clinical manifestation spanning more than 30 years. This clinical presentation might be explained by the small size the septal defect as, according to some authors,3 the degree of atrophy of the conduction tissue is directly related to defect size. Previously published cases correspond to larger septal defects.
In conclusion, the finding of AMS in cardiac imaging is uncommon, and clinical manifestation in the form of complete AVB is even more exceptional. Differential diagnosis in young patients should be extended to include potentially treatable causes for the clinical manifestations.