Among other aims, multidisciplinary heart failure (HF) management programs are designed to reduce admissions1 and improve survival rates. The nursing team plays a crucial role in the achievement of these aims.2 Activities conducted by nursing staff when patients visit a HF unit include encouraging self-help, providing health care advice, and assessing the patient's biopsychosocial situation. In addition, an increasingly important aspect of these programs is telephone assistance,3 which the nursing staff provide alongside patient visits. However, few publications discuss the reasons why patients use this telephone service and how dealing with them affects the professionals working at a specialist unit.
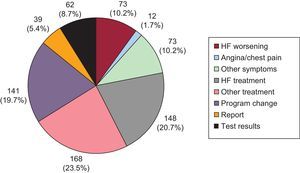
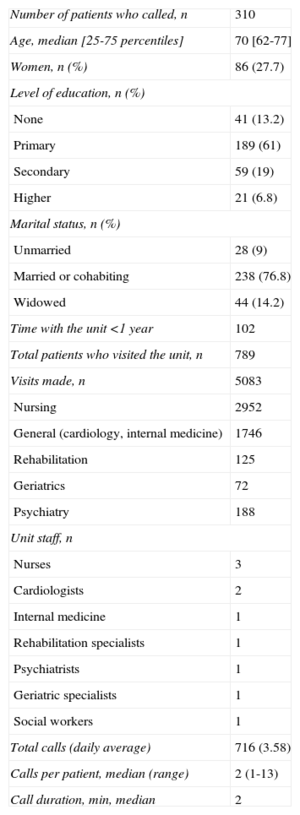
We therefore decided to analyze telephone calls received between February and November 2012 by a multidisciplinary HF unit at a tertiary care hospital offering outpatient services.1 Our aim was to assess the most common reasons for the calls and the response given or action taken following the call. During the study period, 716 telephone calls were received from 310 patients; therefore, 39.2% of the 789 patients treated during this period used the service (Table). A total of 56% of the calls were made by the patient and the remaining 44% by primary care, usually a family member. There was no difference between the patients who called the unit and those who did not in age, sex, marital status, level of education or time registered with the unit. Of the patients who called, those who had been under the care of the unit for less than 1 year when the study began (median=2 years) made more calls (P=.006) than those who had been under its care for more than 1 year (median=1 year). The reasons for the calls are shown in the Figure. There was no difference in reason based on who made the call (P=.18), level of education (P=.15), or marital status (P=.49), but differences were found based on the time registered with the unit (P<.001), since patients who had been with the unit for more than 1 year called more to ask questions about nonheart-related treatment (23.3%), and the more recently registered tended to ask questions about treatment for their HF (27.7%). Only 73 calls (10.2%) were due to worsening symptoms; the most common reasons were fatigue or tiredness (32 calls [43.8%]) and edema (28 calls [38.3%]), ahead of dyspnea (18 calls [24.6%]) and sudden weight gain (12 calls [16.4%]); some patients described more than 1 symptom. Of the calls made in relation to HF treatment, 48% were due to symptomatic hypotension, possibly triggered by the HF treatment itself and with time of year as an added causative trigger, such that these calls significantly increased (P=.004) from June to September compared with the rest of the study period. The most common action taken by the nursing staff (52%) was to give telephone advice (sometimes including advice to visit the patient's family physician), while the patient's HF treatment was changed in only 3.5% of cases. There were no differences in the actions taken by the nursing staff based on who made the call (P=.14), but, as expected, there were differences based on the reason for the call (P<.001). Of all the calls prompted by clinical worsening, 42 (58%) led to an unscheduled visit to the unit, 5 (7%) resulted in a visit to the emergency department and 5 (7%) required a change in medication. Of calls made in relation to HF treatment, 22 (14%) resulted in the caller being referred to a physician, 66 (45%) in telephone advice, and 20 (13.5%) in a change of treatment.
Analysis of Patients Who Called a Multidisciplinary Heart Failure Unit and of the Calls Received
| Number of patients who called, n | 310 |
| Age, median [25-75 percentiles] | 70 [62-77] |
| Women, n (%) | 86 (27.7) |
| Level of education, n (%) | |
| None | 41 (13.2) |
| Primary | 189 (61) |
| Secondary | 59 (19) |
| Higher | 21 (6.8) |
| Marital status, n (%) | |
| Unmarried | 28 (9) |
| Married or cohabiting | 238 (76.8) |
| Widowed | 44 (14.2) |
| Time with the unit <1 year | 102 |
| Total patients who visited the unit, n | 789 |
| Visits made, n | 5083 |
| Nursing | 2952 |
| General (cardiology, internal medicine) | 1746 |
| Rehabilitation | 125 |
| Geriatrics | 72 |
| Psychiatry | 188 |
| Unit staff, n | |
| Nurses | 3 |
| Cardiologists | 2 |
| Internal medicine | 1 |
| Rehabilitation specialists | 1 |
| Psychiatrists | 1 |
| Geriatric specialists | 1 |
| Social workers | 1 |
| Total calls (daily average) | 716 (3.58) |
| Calls per patient, median (range) | 2 (1-13) |
| Call duration, min, median | 2 |
These results differ from those published by Staples et al.4 based on a study of telephone nursing advice, in which the most common reason for calls by the patient or carer was a worsening of the HF symptoms (50% of patients), although we are unable to draw comparisons due to the differences between the 2 studies and the type of unit.
Contrary to our expectations, we found that the main reason for telephone calls to the HF unit was to request advice on treatment not directly related to HF rather than to request advice on worsening of HF symptoms; we believe this finding reflects the large extent to which patients depend on the staff of the unit rather than any mistrust of their physicians. A not inconsiderable proportion of calls were related to bureaucratic issues that could have been dealt with by administrative staff, although it is not unusual for nurses to handle these tasks in units such as ours, a consideration that could affect the planning of future HF units. Just over 10% of calls resulted in an extra visit to the unit more or less immediately, due to the ease with which patients are able to access our care, a feature that sets this type of unit apart. Finally, the nurses only redirected one-tenth of calls to the unit's medical staff, confirming their ability to deal with HF patients and their critical role in the various ways of dealing with this condition.