To the Editor,
Cardiac auscultation is a reliable and cost-efficient clinical skill,1, 2 but is being replaced by sophisticated, costly techniques. Moreover, recent experiences have shown that proficiency in this skill has declined among physicians in training.3 The objective of this report was to evaluate auscultation skills in undergraduate and postgraduate students and determine whether a training program involving a heart sound simulator can improve these skills.
This study included 32 fifth-year medical students (in Chile, undergraduate medical degrees take 7 years to complete) and 18 first- and second-year internal medicine residents. The SAM (Student Auscultation Manikin, Cardionics Inc.; Texas, United States) was used, which is capable of reproducing heart sounds at the 4 standard locations (mitral, aortic, pulmonary, and tricuspid). All of the participants underwent a baseline evaluation that included auscultation of the following sounds: normal heart sounds; mitral stenosis (loud first sound, opening snap, and a rumbling murmur); mitral regurgitation (apical holosystolic murmur); aortic stenosis (ejection click, harsh early-to-midsystolic murmur at the base of the heart); aortic regurgitation (diastolic murmur); third and fourth sounds; and pericardial friction rub. Half of the students and half of the residents were randomly assigned to 1 of 2 groups; each group (the SAM group, participants who underwent a training program in cardiac auscultation using the SAM, and the control group, participants who continued their usual training program) was made up of 25 individuals.
In the SAM group, training consisted of three 45-min sessions of heart sound auscultation with the simulator; in total, each student and resident listened to every sound at least 300 times. Participants were told which sound was being reproduced and could ask the instructor any questions they might have. The order in which the murmurs were auscultated in each session was randomized. Once the training period was over, 4 weeks after the baseline evaluation, all of the participants underwent the final evaluation in which the same manikin was employed; in addition to the 8 sounds described above, the participants were required to listen to 2 additional heart sounds (atrial septal defect and patent ductus arteriosus), in order to reduce the possibility of their identifying the sounds correctly by chance. These new sounds were not evaluated.
This study received the approval of the ethics committee of our institution; the participants had been free to decide whether or not they wished to enroll in it. Participation had no effect on the students’ grades.
In the baseline auscultation, the participants (students and residents) correctly identified an average of 31% of the heart sounds presented to them; there were no significant differences between residents and students (36% vs 26%; P=.22).
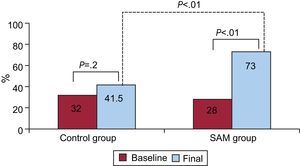
In the final, post-training auscultation, the percentage of correct responses by the participants in the SAM group improved from 28% to 73% (P<.01); in the control group, this percentage increased from 32% to 41.5% (P=.2). The percentage of correct responses in the SAM group was significantly higher than that of the control group (73% vs 41.5%; P<.01) (Figure).
Figure. Percentage of correct diagnoses based on auscultation of heart sounds according to type of training. SAM, Student Auscultation Manikin.
After training, both the students and residents in the SAM group showed a significant improvement in the percentage of correct responses, unlike the participants assigned to the control group. The rate of correct identification by the students in this group increased from 27% to 38% (P=.2), whereas the students in the SAM group improved from 25% to 70% (P<.005). The residents in the control group improved from 40% to 47% (P=.4); in contrast, the residents in the SAM group improved from 33% to 78% (P<.005).
The Table shows the changes in the percentages of correct diagnoses based on specific sounds after training in the SAM group. Recognition of the 8 sounds analyzed significantly improved.
Percentage of Correct Responses Among the Students in the SAM Group According to Heart Sound *
| Heart sound | Baseline, n (%) | Final, n (%) | Improvement, % | P |
| Mitral stenosis | 6 (24) | 18 (72) | 48 | <.001 |
| Mitral regurgitation | 11 (44) | 22 (88) | 44 | <.001 |
| Aortic stenosis | 15 (60) | 24 (96) | 36 | .001 |
| Aortic regurgitation | 8 (32) | 22 (88) | 56 | <.001 |
| Third sound | 7 (28) | 17 (68) | 40 | <.001 |
| Fourth sound | 2 (8) | 9 (36) | 28 | .008 |
| Pericardial friction rub | 4 (16) | 24 (96) | 80 | <.001 |
| Normal | 6 (24) | 15 (60) | 36 | .001 |
SAM, Student Auscultation Manikin.
* The characteristics of the murmurs are specified in the description of the methods.
Correct interpretation of heart sounds is a skill that requires training, and it is understood to be the task of medical schools to provide proper instruction in this area. However, this is not happening, and these skills—like other basic skills—are not being correctly taught or evaluated.4, 5 The utilization of simulators appears to be an attractive training option. Their use for teaching cardiac auscultation has been validated in previous experiences. For example, Barrett et al.6 had participants listen to 4 cardiac murmurs 500 times using a simulator or recordings of murmurs on a compact disk, with a total of 6h of training. Our protocol required fewer repetitions (300 per murmur) and less instruction time (2.2h) with satisfactory results, and will help students to recognize murmurs in real patients.
In short, undergraduate and postgraduate students in our medical school correctly identify only about one third of the heart sounds they hear. A training program involving a heart sound simulator can significantly improve this skill. It would be interesting to reevaluate these students at distinct time periods to determine the need to repeat these modules throughout their training.
FundingA resident fellowship from the Pontificia Universidad Católica de Chile.
Corresponding author: eguarda@med.puc.cl