To the Editor,
Late stent malapposition (LSM) is diagnosed using intravascular ultrasound (IVUS) and defined as a separation of the stent struts from the intima of the coronary artery wall which was not present just after implanting the stent. This phenomenon is more common after implanting a drugeluting stent [DES] (incidence rate = 12%-14%1) than after implanting a metal stent (incidence rate = 4%-5%2).
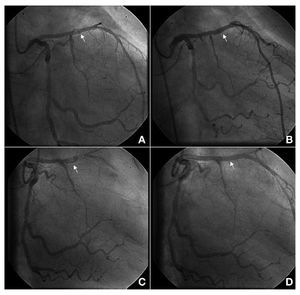
We present the case of a female patient aged 80 years with hypertension, dyslipidaemia, and diabetes who was seen in 2004 due to acute coronary syndrome with heart failure. The echocardiogram showed severe ventricular hypertrophy and anterior hypokinesia with an ejection fraction of 48%. The coronary angiography showed one vessel disease with a critical lesion in the segment proximal to the anterior descending artery. Next, a sirolimus-eluting stent was implanted, which produced good results with no complications (Figure 1A). The patient was discharged with aspirin and clopidogrel as a double platelet antiaggregant treatment.
Figure 1.A: coronary angiography after stent implantation. B: coronary angiography 24 months later. The arrow shows the area with suspected incomplete apposition. C: coronary angiography 49 months later, showing stent thrombosis. D: coronary angiography after implementation of 2 metal stents.
In December 2006, 24 months after the procedure, the patient was still taking the double platelet antiaggregant treatment and presented severe nosebleeds; for this reason, both antiaggregants were discontinued. The patient developed symptoms of infection secondary to the blockage produced by the nosebleeds. With this profile and having discontinued antiaggregant treatments, she presented general non-ST elevation acute coronary syndrome. We performed an additional coronary angiography, which showed insignificant coronary lesions as well as the image of a possible contrast leak around the stent (Figure 1B) which was not considered significant and not studied with IVUS. The patient made good clinical progress and was discharged with an antiaggregant treatment of aspirin alone.
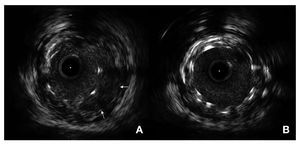
The patient remained asymptomatic until January 2009, 49 months after the procedure, when she was admitted due to an acute myocardial infarction with anterior ST segment elevation considered Killip class II, with more than 12 hours of evolution. She was continuing treatment with 150 mg aspirin at the time. A new coronary angiography was performed, showing thrombosis at the stent implanted in the anterior descending artery (Figure 1C). During the procedure, after having performed a thrombectomy that provided abundant material, an IVUS examination was carried out which detected a LSM on most of the stent, with no evidence of poor expansion, images showing dissection, or other complications (Figure 2A).
Figure 2. A: IVUS 49 months later, showing the area with incomplete apposition (arrows). B: end result with no incomplete apposition.
Two metal stents that were larger in diameter than the previous one were implanted and subjected to high pressure post-dilation. Angiographic (Figure 1D) and ultrasound (Figure 2B) results were good. The patient showed good clinical progress and was discharged with double platelet antiaggregant treatment.
At present, clinical progress is unknown for patients with a stent who develop LSM. On the one hand, some long-term follow-up studies describe patients with a LSM who have received conservative treatment and whose coronary event incidence rate is no higher than that of patients without LSM.3,4
However, other studies describe that LSM is much more frequent among patients with very late onset of stent thrombosis compared to other asymptomatic patients. They suggest a likely physiopathological relationship between LSM and stent thrombosis.5,6
We present a case of LSM which received conservative treatment and led to very late-onset stent thrombosis (49 months after stent implantation). Given our current knowledge, defining the proper treatment strategy in these cases is very difficult. One option could be pharmacological with the recommendation of long-term double antiaggregant treatment; however, since thrombosis may occur very late, the treatment should be indefinite, and the problems it creates will be continuous. Another option could be treating the LSM percutaneously by dilating or implanting a stent within a larger stent, as was finally done in this case.
The case we present supports the possibility of a causal relationship between LSM and late-onset thrombosis.