To the Editor,
Tako-Tsubo cardiomyopathy (TC) is a syndrome of clinical presentation, electrical impulses, and segmental impairments similar to the anterior myocardial infarction and it is characterized by the absence of significant coronary diseases causing ventricular dysfunction and by the normalization of the left ventricular function in the short term.
We present the case of a 61-year-old woman, with high blood pressure, hypercholesterolemia and a suspected severe anaphylactic reaction during the anesthetic induction of a urinary tract neoplasia; no significant arterial pressure figures could be observed with noninvasive monitoring. As a result, a high dose-adrenalin-and-noradrenalin perfusion was initiated and the patient taken to the intensive care unit.
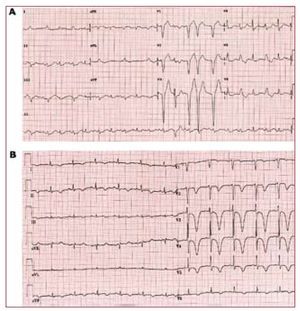
The patient had initially normal baseline ECG but exhibited a left bundle branch block and one hour after exhibiting these symptoms the ECG confirmed hypertrophy of the basal septum (14 mm) with septal, apical, and lateral akinesia and hyperdynamic movement of the basal portions (with no dynamic gradient in the left ventricular outflow tract) and a severe global systolic dysfunction.
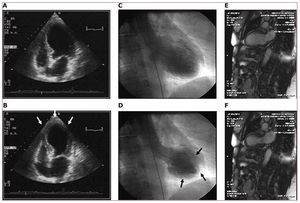
Suspecting TC yet still unable to rule out acute coronary syndrome, cardiac catherization was performed 2 hours after catecholamine perfusion. It showed coronary arteries without major injuries and confirmed the segmental impairments noted (Figures 1 and 2).
Figure 1. A: ECG in the acute stage where left bundle branch block was observed. B: later evolution with neutralization of T-waves, frequent in stress cardiomyopathy.
Figure. 2. Images from transthoracic ECG and ventriculography within first hours of exhibiting the symptoms showing extensive akinesia with preserved contraction in more basal portions (B and D). The 48-hour cardiac magnetic resonance imaging still shows segmental impairments with a slight improvement compared to the acute stage (E and F).
Patient exhibited some hemodynamic improvement after interrupting inotrope drugs in the absence of further pharmacological drugs like beta-blockers or balloon pumps. The ECG proved the left bundle branch block was gone and negative T-waves appeared in the antero-lateral face with late normalization.
The 48-hour cardiac magnetic resonance imaging proved global contractility and segmental impairments with no late enhancement had improved significantly. Monthly ECG monitoring proved the global and segmental ventricular function was normal.
A chest CT scan performed at a later stage showed that the apparent hypotension during the noninvasive monitoring was secondary to a proximal occlusion of the left subclavian artery and to an occlusive stenosis of the right subclavian artery, with a 70 mm Hg difference wih respect to measurements taken through the femoral artery.
TC is a reversible form of the LV regional systolic dysfunction. These are some of the theories that might actually explain its causes: the multivessel transient vasospasm,1 the rupture of the atheromatous plaque in the LAD (only seen using intravascular ultrasound),2 the formation of a dynamic intraventricular gradient (when there is medioseptal hypertrophy with an exaggerated adrenergic tone), the spasm-induced microvascular ischemia with normal coronary epicardial arteries,3-6 or the catecholamine-induced myocardial dysfunction.7
Findings of this case prove stress cardiomyopathy followed the high-dose catecholamine administration when interpreting fictitious hypotension as an anaphylactic response, so we believe catecholamine-induced myocardial stunning is the main physiopathological base for the apical transient dyskinesia.