Despite the established diagnostic value of the electrocardiogram in preparticipation screening of athletes, some cardiac structural changes can be missed, particularly in early disease stages. The aim of this study was to evaluate the prevalence of cardiac structural changes via the systematic use of echocardiography in preparticipation screening of competitive athletes.
MethodsProfessional athletes or participants in a competitive athletic program underwent a screening that included family and personal medical history, physical examination, electrocardiography, exercise testing, and Doppler echocardiography.
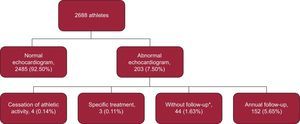
ResultsA total of 2688 athletes (67% men; mean age [standard deviation], 21 [10] years) were included. Most of the echocardiographic evaluations (92.5%) were normal and only 203 (7.5%) showed changes; the most frequent change was left ventricular hypertrophy, seen in 50 athletes (1.8%). Cessation of athletic activity was indicated in 4 athletes (0.14%): 2 for hypertrophic cardiomyopathy (electrocardiography had shown changes that did not meet diagnostic criteria), 1 pectus excavatum with compression of the right ventricle, and 1 significant pulmonary valve stenosis; the rest of the changes did not entail cessation of athletic activity and only indicated periodic monitoring.
ConclusionsAlthough rare, some cardiac structural changes can be missed on physical examination and electrocardiography; in contrast, they are easily recognized with echocardiography. These findings suggest the use of echocardiography in at least the first preparticipation screening of competitive athletes to improve the effectiveness of programs aimed at preventing sudden death in athletes.
Keywords
Despite the low incidence of sudden death in athletes,1 it presents a challenge to ideas about the undoubted beneficial health effects of exercise. The association between sudden death and exercise has been and continues to be controversial.2 However, it is recognized that athletic activity entails a hemodynamic demand that can be unacceptable for hearts with underlying heart disease, resulting in malignant arrhythmias and, potentially, sudden death.
One of the proposed approaches to ameliorate this risk of death involves the systematic medical evaluation of athletes—so-called preparticipation screening (PPS)—which aims to detect diseases that could be life-threatening during physical exercise, particularly when the activity is intense or extreme. Although controversy persists over the funding and economic resources available for performing these systematic screening programs, there is currently agreement that cardiological evaluation should at least be performed. However, the optimal examination in this type of screening is still under debate. In the United States, only a medical history and directed physical examination is recommended, whereas in Europe 12-lead electrocardiogram (ECG) is recommended or included in the PPS.3 Nonetheless, different countries within Europe apply different regulations regarding the minimum complementary tests that should be used in competitive athletes, ranging from ECG to exercise testing or compulsory echocardiography.4
Echocardiography is a relatively inexpensive technique that allows identification of the main causes of preventable sudden death, such as heart muscle diseases, coronary artery origin anomalies, and aortic disease. Echocardiography use would improve the sensitivity and specificity of PPS in detecting potentially serious changes in athletes, as well as in identifying those individuals requiring cardiac surveillance or special care.
Accordingly, the aim of this study was to evaluate the usefulness of the echocardiogram in PPS programs for competitive athletes by determining the prevalence and characterizing the types of cardiac structural changes found.
METHODSFrom January 2009 to December 2013, 2688 athletes from different sporting disciplines were consecutively studied. All participants were included in a competitive athletic program of the Catalan Sports Council (Consell Català de l’Esport) or Barcelona Football Club. All athletes underwent a cardiovascular evaluation consisting of the following 5 items: a) family and personal history; b) physical examination according to Bethesda conference recommendations5c) ECG; d) echocardiogram, and e) maximum exercise testing.
EchocardiographyAll athletes underwent 2-dimensional echocardiography using a commercially available system (Vingmed Vivid-7, General Electric Vingmed; Milwaukee, Wisconsin, United States; or Aplio XV and 400; Toshiba, Japan). The following parameters were measured: the diameter of the left ventricle (LV) in end-diastole and endsystole, the thickness of the interventricular septum and posterior wall of the LV, and the anteroposterior diameter of the left atrium. Valvular morphology was assessed, as well as the origins of both coronary arteries and the presence of intracardiac shunts or other congenital malformations. Transvalvular blood flow was estimated with quantitative Doppler echocardiography according to the recommendations of the European Association of Echocardiography.6 Valvular regurgitation was semiquantitatively evaluated through color Doppler echocardiography using a 4-grade scale (I, mild; II, moderate; III, severe; and IV, massive) according to the recommendations of the European Society of Cardiology.7
Experienced cardiologists performed all studies, which were digitally stored for off-line analysis. In the case of disagreement, the entire team reviewed the data.
Statistical AnalysisA general descriptive analysis was performed. Quantitative variables are expressed as the mean (standard deviation). Discrete variables are presented as the number of individuals and percentages. All data were analyzed using the IBM SPSS statistical software package (version 19).
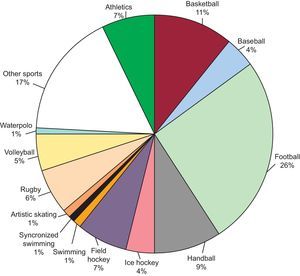
RESULTSOf the 2688 athletes evaluated, 67% were men, with a mean age of 21 (10) years (range, 14–45 years.) The sporting activities practiced by the study population are shown in Figure 1. At the time of the study, 164 of the 2688 athletes studied (6.1%) were professionals. The majority of the study population (2139 [79.6%]) competed in regional competitions, whereas 357 (13.2%) and 192 (7.2%) competed in national and international events, respectively.
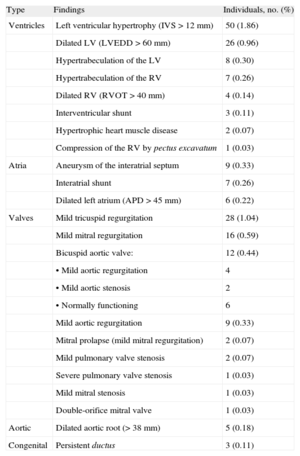
Most of the echocardiography examinations (92.5%) were normal and showed no cardiac disease; in 203 participants (7.5%), changes were seen in the echocardiogram (Table 1). The change most frequently found in the echocardiogram was left ventricular hypertrophy: 50 athletes (1.86%) were found to have left ventricular hypertrophy, using an interventricular septum cut-off of 12mm. The incidence was reduced to 30 (1.11%) if the cut-off was increased to 13mm. Thus, 20 participants showed left ventricular hypertrophy that could be considered “physiological”; none of the ECGs of these athletes met the diagnostic criteria of hypertrophic heart muscle disease.
Echocardiographic Findings in the Athletes
| Type | Findings | Individuals, no. (%) |
| Ventricles | Left ventricular hypertrophy (IVS > 12 mm) | 50 (1.86) |
| Dilated LV (LVEDD > 60 mm) | 26 (0.96) | |
| Hypertrabeculation of the LV | 8 (0.30) | |
| Hypertrabeculation of the RV | 7 (0.26) | |
| Dilated RV (RVOT > 40 mm) | 4 (0.14) | |
| Interventricular shunt | 3 (0.11) | |
| Hypertrophic heart muscle disease | 2 (0.07) | |
| Compression of the RV by pectus excavatum | 1 (0.03) | |
| Atria | Aneurysm of the interatrial septum | 9 (0.33) |
| Interatrial shunt | 7 (0.26) | |
| Dilated left atrium (APD > 45 mm) | 6 (0.22) | |
| Valves | Mild tricuspid regurgitation | 28 (1.04) |
| Mild mitral regurgitation | 16 (0.59) | |
| Bicuspid aortic valve: | 12 (0.44) | |
| • Mild aortic regurgitation | 4 | |
| • Mild aortic stenosis | 2 | |
| • Normally functioning | 6 | |
| Mild aortic regurgitation | 9 (0.33) | |
| Mitral prolapse (mild mitral regurgitation) | 2 (0.07) | |
| Mild pulmonary valve stenosis | 2 (0.07) | |
| Severe pulmonary valve stenosis | 1 (0.03) | |
| Mild mitral stenosis | 1 (0.03) | |
| Double-orifice mitral valve | 1 (0.03) | |
| Aortic | Dilated aortic root (> 38 mm) | 5 (0.18) |
| Congenital | Persistent ductus | 3 (0.11) |
APD, anteroposterior diameter; IVS, interventricular septum; LV, left ventricle; LVEDD, left ventricular end-diastolic diameter; RV, right ventricle; RVOT, right ventricular outflow tract.
Cessation of sporting activity was indicated in 4 athletes (0.14% of the study population). Two of the 4 athletes had hypertrophic heart muscle disease; in 1 of these athletes, the ECG showed nonspecific changes (negative T waves in the left wall) that failed to meet diagnostic criteria. The third individual had a pectus excavatum that compressed the right ventricle. The fourth individual showed significant pulmonary valve stenosis. The other changes found did not indicate cessation of athletic activity. Of the remaining 199 athletes whose echocardiograms showed some change not contraindicating sporting activity, a specific treatment was indicated in 3 individuals (0.11%): percutaneous closure of an interatrial shunt and persistent ductus in 2 and 1 athletes, respectively. In 44 individuals (1.63% of the studied population), no specific treatment or follow-up was ordered and cardiological fitness for athletic activity was maintained because the echocardiographic findings (mild tricuspid or mitral regurgitation) were considered to be trivial. In 152 individuals (5.65%), the findings indicated an annual follow-up. A summary of the echocardiogram results in the PPS of the athletes is shown in Figure 2. The other major changes described—5 interatrial shunts, 2 cases of ductus, and the interventricular shunts—were all small in size and without hemodynamically significant shunting, which did not indicate their preventative closure.
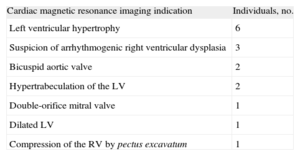
In 16 athletes (0.59%), cardiac magnetic resonance imaging was ordered as a complementary imaging technique when the echocardiogram failed to provide a definitive diagnosis due to an insufficient acoustic window (to evaluate certain bicuspid aortic valves or the ascending aorta) or to further study the anomaly (more appropriate assessment of ventricular hypertrophy, analysis of the right ventricle, inspection of the coronary artery origin in bicuspid arteries, or examination of the ascending artery); the reasons for requesting magnetic resonance imaging are detailed in Table 2. Magnetic resonance imaging failed to provide a different diagnosis or alter the therapeutic approach or follow-up from that indicated by the echocardiogram findings.
Indications for Cardiac Magnetic Resonance Imaging
| Cardiac magnetic resonance imaging indication | Individuals, no. |
| Left ventricular hypertrophy | 6 |
| Suspicion of arrhythmogenic right ventricular dysplasia | 3 |
| Bicuspid aortic valve | 2 |
| Hypertrabeculation of the LV | 2 |
| Double-orifice mitral valve | 1 |
| Dilated LV | 1 |
| Compression of the RV by pectus excavatum | 1 |
LV, left ventricle; RV, right ventricle.
Our results showed that addition of echocardiography to PPS was useful because it completed the evaluation and enabled the diagnosis of 4 athletes with risk of sudden death and 3 athletes with a disease that required a specific treatment or follow-up. None of these problems had been detected via medical history, physical examination, or 12-lead ECG. Although the described findings are of low prevalence, the implications of having been able to prevent 4 cases of sudden death or the subclinical progression of cardiac disease in the athletic context show the importance and value of adding echocardiography to PPS.
The usefulness of echocardiography in experienced hands for excluding cardiac structural alterations is undeniable. One such use is in the diagnosis of structural cardiac disease in the presence of significant changes in the ECG, namely, group 2 of the ECG anomalies described in athletes in the current guidelines.8
The incidence of changes in the echocardiogram was lower in our population than that of another study performed in football players,9 but higher than that of a large study that observed elite athletes.10 The higher incidence of abnormal findings in our study than that reported by Pelliccia et al10 could be explained by 2 reasons. On one hand, more minor cardiac changes have been assessed in our study, changes that do not exclude athletic competition but that are important when establishing a strict follow-up of these athletes. On the other hand, the athletes included in the study performed in Italy were elite and had already undergone a legally mandated PPS, meaning that those already detected with changes had been excluded. In our opinion, this additional value of echocardiography makes the echocardiogram a useful tool for the monitoring of competitive athletes.
Although these changes are usually considered trivial, their progression is completely unknown in those partaking in intensive training programs. Previous studies indicated that training should not cause an increased progression of these mild-to-moderate diseases,11 but the evidence remains scarce. In athletes without heart disease that participated in one or more Olympic Games, a 17-year follow-up revealed no significant changes in the volume, mass, and motility of the LV, and, crucially, found only a slight increase in left atrium size that fell within the normal range.12
Recently, a higher prevalence has been described of diagnostic criteria for apical noncompaction or hypertrabeculation of the LV in athletes.13 Although the prevalence of noncompaction cardiac heart muscle was lower in our series, the differential diagnosis of this abnormality was made in 8 athletes (0.3%). In this subgroup, the inclusion of ECG data is required to make diagnostic and follow-up decisions, especially when there are ventricular repolarization and echocardiography changes, and particularly when there is a decrease in the systolic function of the LV.
Although the incidence of bicuspid aortic valves in athletes is similar to that of the general population, a 5-year follow-up revealed that athletes with bicuspid aortic valve show a significant increase in the dimensions of the LV compared with athletes that have a tricuspid aortic valve, although the values were still within normal limits.14 Similarly, even if athletes with bicuspid aortic valves maintain a normal LV ejection fraction, the strain rate is lower in apical segments of the LV than in athletes that have a tricuspid aortic valve.15 Therefore, the impact of long-term training on small cardiac changes is poorly understood, but chronic volume overloading probably causes some difference in the development of those individuals that at the very least requires monitoring, and therefore its early detection is clinically important.
Dilation of the right ventricle is defined as an outflow tract diameter > 40mm,16 and right ventricular hypertrabeculation is diagnosed by the presence of more than 3 trabeculations > 3mm.17 Mild tricuspid and pulmonary regurgitations are frequent in the healthy population,18 and they were recorded only when they were significant and considered moderate; that is, trivial and mild regurgitations were not described.
Finally, with technological advances in echocardiography systems, the diagnostic sensitivity for detecting an abnormal origin in the coronary arteries has increased from 80% to more than 96%.19 In fact, echocardiography is the noninvasive diagnostic method of choice for confirming this diagnosis.20 In our series, a systematic search was performed for the ostium of both coronary arteries, and it was identified in 99% of individuals.
LimitationsOne of the problems raised by the systematic use of echocardiography is the inherent limitation of the ultrasound technique, such as the diagnostic difficulties posed by poor acoustic windows, although they are infrequent in athletic individuals and athletes. In our series, the frequency of the complementary use of cardiac magnetic resonance imaging as a diagnostic technique was < 1%. This finding is consistent with the only relevant series published in Italy,21 in which < 5% of participants required more complex examinations, such as cardiac magnetic resonance imagining, electrophysiology studies, and angiography.
The cost-effectiveness of PPS programs has been controversial. In fact, many sporting bodies in Western Europe dispense with PPS or ECGs for competitions. Thus, the systematic use of echocardiogram may be idealistic. However, we believe that echocardiogram use does not involve an excessive additional expense and that echocardiography should become part of the PPS program, at least in its initial assessment. Other authors have proposed including a short and directed echocardiogram,19 with a special focus on excluding diseases that cause problems for athletes, such as hypertrophic heart muscle disease, anomalous origins of the coronary arteries, mitral valve prolapse, and right ventricular dysplasia. Accordingly, we consider appropriate the current European recommendations, which recommend that all competitive athletes undergo a basic cardiovascular evaluation (family and personal history, physical examination, and ECG)22,23 and that more detailed cardiovascular evaluation (which includes maximum exercise testing and echocardiography) be reserved for those that practice highly competitive or demanding physical activities.24
CONCLUSIONSSome cardiac structural changes that can be missed on physical examination and ECG are easily recognized with echocardiography. These changes can force the cessation of athletic activity in some isolated cases (possibly preventing sudden death), whereas in other cases they can enable the early detection of less serious anomalies that require cardiological monitoring and whose progression in response to chronic exercise is currently poorly known. All of these observations indicate that echocardiography should be performed in at least the first PPS of competitive athletes.
FUNDINGThis study was partially funded by the Spanish Government through the National R+D+I Plan (DEP2010-20565).
CONFLICTS OF INTERESTSNone declared.
To the Mémora Group for supporting research into the prevention of sport-related sudden death.