Atherosclerotic cardiovascular disease remains the major cause of premature death in developed and developing countries. Nevertheless, surveys show that most patients still do not achieve the lifestyles, risk factor levels, and therapeutic targets recommended in primary and secondary prevention. The present update reflects the most recent novelties in risk classification and estimation of risk and documents the latest changes in fields such as smoking, diet and nutrition, physical activity, lipids, hypertension, diabetes, and cardiovascular rehabilitation, based on experimental trials and population-based observational studies.
Keywords
.
INTRODUCTIONThere is a long period between the beginning of atherosclerotic disease and the onset of clinical manifestations, which often occur abruptly and with irreversible consequences. Fortunately, this disease can usually be predicted; its risk factors are well characterized and its prevention can be addressed using a wide variety of interventions. Primary prevention takes place over an extended period (decades), targets very large segments of the population, and consumes resources other than the healthcare resources required to manage the clinical disease per se. In addition, both secondary prevention and comprehensive rehabilitation play a vital role after a cardiovascular (CV) disease event.
Although the development of new drugs seems to have slowed—reflecting a world in crisis—there are continuous developments in all fields and old concepts and paradigms are giving way to new ones that never fail to surprise. Furthermore, in 2012, the European guidelines on CV disease prevention were updated1 in an extensive document that gathers all the knowledge from guidelines published since 2007 and which serves as the cornerstone of the present review.
We present an analysis of the recent literature, as well as the most relevant communications from 2012 medical meetings, all of which are compared with developments presented in consensus documents.
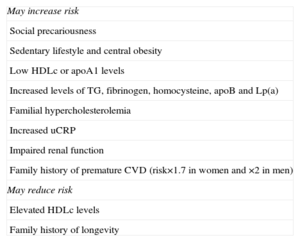
CARDIOVASCULAR RISK ESTIMATION AND STRATIFICATIONThe European Society of Cardiology1,2 continues to recommend the SCORE (Systematic COronary Risk Evaluation) risk chart (class IC recommendation), which is used to calculate the 10-year risk of CV disease mortality in asymptomatic persons. Some new features have been added: a) the inclusion of high-risk or very high-risk patients in whom calculation of the SCORE risk is unnecessary and those with chronic kidney disease (glomerular filtration rate<60 mL/min/1.73 m2); b) other circumstances that can modulate risk which had not been previously considered cardiovascular risk factors (CVRF) (Table 1); c) a supplementary chart with risk adjustment taking into account the level of high-density lipoprotein cholesterol (HDLc), which is highly relevant to Spain,3 and d) estimation of the risk of morbidity and mortality by tripling the risk-of-death score.
Circumstances That Can Increase or Decrease Cardiovascular Risk.
| May increase risk |
| Social precariousness |
| Sedentary lifestyle and central obesity |
| Low HDLc or apoA1 levels |
| Increased levels of TG, fibrinogen, homocysteine, apoB and Lp(a) |
| Familial hypercholesterolemia |
| Increased uCRP |
| Impaired renal function |
| Family history of premature CVD (risk×1.7 in women and ×2 in men) |
| May reduce risk |
| Elevated HDLc levels |
| Family history of longevity |
apoA1, apolipoprotein A1; apoB, apolipoprotein B; CVD, cardiovascular disease; HDLc, high-density lipoprotein cholesterol; Lp(a), lipoprotein(a); TG, triglycerides; uCRP, ultra-sensitive C-reactive protein.
Adapted from Perk et al.1
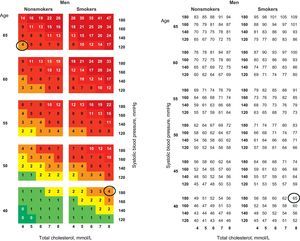
One aspect that deserves comment is the inclusion of the concept of CV risk age, which refers to estimated age depending on the patient's CV disease risk. Previous guidelines have recommended calculating the “relative risk” of a young person with CVRF compared with that in people of the same age without these risk factors. Currently, however, young individuals with multiple CVRFs are matched to older individuals without CVRF but who have the same level of risk, which is solely based on their advanced age.4 Tables have been specifically developed to calculate this value (Fig. 1).
Cardiovascular risk in a 40-year-old male smoker, systolic blood pressure of 180 mmHg; total cholesterol, 8 mmol/L: 4%, equivalent to that of a 65-year-old man without risk factors (nonsmoker; systolic blood pressure, 120 mmHg; total cholesterol, 4 mmol/L). In the right-hand chart, age is calculated according to cardiovascular risk, which is equivalent to 65 years. Adapted from Cooney et al.4
A meta-analysis has shown that the analysis of gene variants is no better than calculation based on classic CVRFs in predicting subclinical atherosclerosis, as assessed by carotid ultrasound.5 There is debate concerning the inclusion of carotid ultrasound or computed tomography to detect coronary calcium;6 risk estimation can be improved by assessing the lesion in the target organ or metabolic syndrome, without the need to resort to sophisticated techniques.7
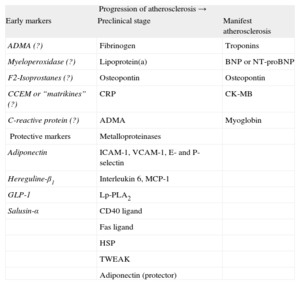
BIOMARKERSBiomarkers are biological indicators associated with the occurrence of a disease.8 This concept differs from risk factor, which implies a causal relationship. The model that uses the classic CVRFs, included in the SCORE charts, has some limitations, which has led to interest in new markers that could improve predictive ability, although few of these markers have been recommended in clinical practice (Table 2).9–11
Biomarkers in the Cardiovascular Continuum.9–11
| Progression of atherosclerosis → | ||
| Early markers | Preclinical stage | Manifest atherosclerosis |
| ADMA (?) | Fibrinogen | Troponins |
| Myeloperoxidase (?) | Lipoprotein(a) | BNP or NT-proBNP |
| F2-Isoprostanes (?) | Osteopontin | Osteopontin |
| CCEM or “matrikines” (?) | CRP | CK-MB |
| C-reactive protein (?) | ADMA | Myoglobin |
| Protective markers | Metalloproteinases | |
| Adiponectin | ICAM-1, VCAM-1, E- and P-selectin | |
| Hereguline-β1 | Interleukin 6, MCP-1 | |
| GLP-1 | Lp-PLA2 | |
| Salusin-α | CD40 ligand | |
| Fas ligand | ||
| HSP | ||
| TWEAK | ||
| Adiponectin (protector) | ||
ADMA, asymmetric dimethylarginine; BNP, brain natriuretic peptide; CCEM, components of cardiac extracellular matrix (type I and type III procollagen); CK-MB, MB fraction creatine kinase; CRP, C-reactive protein; GLP-1, glucagon-like peptide-1; HSP, heat shock proteins; ICAM-1, intercellular adhesion molecule-1; Lp-PLA2, lipoprotein-associated phospholipaseA2; MCP-1, monocyte chemoattractant protein-1; NT-proBNP, N-terminal pro-brain natriuretic peptide; TWEAK, tumor necrosis factor-like weak inducer of apoptosis; VCAM-1, vascular cell adhesion molecule-1.
Question marks follow certain biomarkers because it is still not sufficiently clear whether these are truly useful for the purpose indicated in the corresponding column.
The best-characterized biomarker of inflammation closest to clinical use is ultrasensitive C-reactive protein (uCRP). The ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial)12 showed that baseline uCRP and low-density lipoprotein cholesterol (LDLc) correlated with the occurrence of CV events, but that the Framingham risk prediction model was not improved by the inclusion of uCRP, a finding that has provoked controversy.13
Similarly, a recent meta-analysis14 showed that the addition of lipoprotein(a) or lipoprotein-associated phospholipase A2 added little information to that provided by traditional risk factors.14 A recent publication15 has given new impetus to the role of inflammation in atherogenesis, showing a relationship between a genetic variant known to affect the function of the interleukin 6 receptor (Asp358Ala; rs2228145) and decreased CV risk.
IMAGING TECHNIQUES IN PREDICTING CARDIOVASCULAR RISKImaging techniques can identify atherosclerotic burden and refine risk stratification.16 There have been no major new advances in this field in the last 12 months. The ACCF/AHA (American College of Cardiology Foundation/American Heart Association) guidelines 2010 recommended determination of the coronary calcium score as being useful for risk assessment in adults with intermediate-risk (class IIa); the European guidelines17 also assign this recommendation to class IIa, but with a weak level of evidence.
A prospective population-based study conducted in Rotterdam analyzed the impact of new risk markers and included the N-terminal pro-brain natriuretic peptide, fibrinogen, uCRP, homocysteine, coronary artery calcium score, carotid intima-media thickness (CIMT), pulse wave velocity, and the presence of peripheral vascular disease. The coronary artery calcium score was the only risk factor that substantially improved CV disease risk prediction compared with conventional CVRFs.18
CIMT appears to play a weak role in population studies using conventional CVRFs. The Strong Heart Study19 showed that the presence of carotid plaque, but not CIMT, was predictive of events. However, the C statistic changed relatively little (from 0.700 to 0.714; P=.011), which calls into question the practical utility of using carotid ultrasound when examining this type of population.
NUTRITIONThe most recent European guidelines on CV disease prevention1 recommend a balanced diet that maintains body mass index<25 kg/m2. These guidelines also describe a J-shaped relationship between alcohol use and CV disease (maximum intake 20 g/day for men and 10 g/day for women), support the benefit of DASH (Dietary Approaches to Stop Hypertension) for hypertension and highlight the complete absence of evidence in support of treating elevated homocysteine levels.
No position is taken regarding omega 3 fatty acids, although they are recommended in the European guidelines on dyslipidemia (class IIaB).2 A recent meta-analysis found no reduction in mortality or CV disease events.20
Currently, there is no evidence that phytosterols prevent CV disease, although doses of 2 g/day can lower LDLc by 7% to 10%.21
The Spanish Association for the Study of Obesity does not recommend high-protein Dukan-type diets; in the short term these diets may induce greater weight loss than a heart-healthy diet but weight reduction is not maintained after 12 months and long-term efficacy remains undemonstrated.22
PHYSICAL EXERCISEPhysical exercise is recognized as a key intervention in preventing CV disease. There is clear scientific evidence demonstrating the beneficial effect of physical activity in reducing morbidity and improving functional capacity23 although debate continues regarding the type and intensity of activity.24 High-intensity training achieves better results regarding aerobic capacity, even when low-intensity training is augmented by longer duration or frequency,25 but the issue of safety remains open to question. Recent studies have found that high-intensity interval training is more effective than the traditional method of moderate continuous training, achieving better results in functional capacity and other predictors.26
SMOKINGThe EUROASPIRE (European Action on Secondary and Primary Prevention through Intervention to Reduce Events) registries appear to suggest that smoking is still a pending issue.27 Two contradictory circumstances come together: the risk to health posed by smoking (not only CV disease) and the disturbing neglect of this habit by the medical community, especially cardiologists. The recent European guidelines update1 has highlighted the role of laws restricting tobacco consumption in public places as a tool to prevent and control smoking. In January 2011, Spain extended the law to prohibit smoking in any enclosed space for collective use, in addition to prohibiting smoking in some open areas. Although this law has had some success in reducing the prevalence of smoking, its effect on reducing admissions for infarction or angina and its resulting economic impact, as demonstrated in a recent study in Germany,28 awaits confirmation. Importantly, the impact of smoking on the risk of infarction is greater among young people29 and the prevalence of smoking has continued to rise in women, an issue of some concern.
The current European guidelines mention 3 first-line pharmacological aids for smoking cessation (nicotine replacement therapy, buproprion, and varenicline), of which varenicline is the most effective. Side effects are rare, but there is some uncertainty concerning its neuropsychiatric safety profile and CV disease. An initial meta-analysis reported an increase in CV events.30 The methodology used in this study was questioned, but its publication impacted on the use of varenicline. The Food and Drug Administration cautiously confirmed that the slight increase in CV disease risk does not outweigh the wide benefits of quitting smoking. Subsequently, a more conventional meta-analysis was published, which analyzed the rate of CV events in 22 double-blind randomized trials of varenicline compared with placebo. The rate of CV events was low and no difference was found between varenicline and placebo. It was concluded that the use of varenicline did not significantly increase CV disease events, thus reestablishing its role.31
HYPERTENSIONA study of the diagnosis of hypertension (HT) compared the use of ambulatory blood pressure monitoring (ABPM), home blood pressure monitoring (HBPM) and casual blood pressure monitoring to predict subclinical cerebrovascular disease in the general population.32 ABPM and HBPM values were associated with the risk of subclinical cerebrovascular disease and carotid atherosclerosis. The most powerful predictor of subclinical cerebrovascular disease was the nocturnal ABPM value. The HBPM value was more closely associated with the risk of carotid atherosclerosis than any of the ABPM values. Casual blood pressure readings were not associated with the risk of cerebrovascular disease.
Two large meta-analyses on the pharmacological treatment of HT were published this year. The first33 examined the efficacy of hydrochlorothiazide vs chlorthalidone and concluded that chlorthalidone leads to greater reduction in CV disease than hydrochlorothiazide. In total, the number-needed-to-treat to prevent 1 CV disease event over 5 years was 27. The second study34 demonstrated that the combination of aliskiren with angiotensin-converting enzyme inhibitors and angiotensin receptor blockers increased the risk of hyperkalemia compared with monotherapy with either angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. The recent termination of the ALTITUDE (Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints)—which was not included in the second study34—due to an unexpected incidence of adverse events in diabetic patients receiving a combination of aliskiren with other renin-angiotensin system inhibitors, is another wake-up call.
The novel technique of renal denervation via radiofrequency ablation of the renal arteries has achieved notable decreases in blood pressure in patients with resistant HT. An expert group has published an article describing the requirements, evidence and future development of the technique.35 In addition, long-term follow-up of the SIMPLICITY clinical trials have been published endorsing its efficacy and safety.
Regarding the control of HT in Spain, a meta-analysis36 determined the prevalence of uncontrolled HT in 341 632 patients with different risk characteristics and the outlook is bleak. Among hypertensive patients, the prevalence of uncontrolled HT was 67%, and in patients at high CV disease risk the prevalence reached 87.6% (target<130/80 mmHg). In a study which included 6675 participants, a different Spanish group also demonstrated that knowledge of HT increased according to the frequency of health service attendance; the factors associated with frequency of attendance were female sex, age, and having health problems.37
In the field of prognosis, a new study of 5788 patients found a J-curve relationship, with increased CV disease events and mortality rates above and below the nadir blood pressure of 143/82 mmHg.38
LIPIDSThe main changes regarding lipids are represented by new findings related to target LDLc and non-HDLc levels. A meta-analysis of 60 000 patients treated with statins demonstrated that achieving LDLc values below 100 mg/dL did not reduce the incidence of CV disease unless non-HDLc levels below 130 mg/dL were also achieved.39 Another important finding of this meta-analysis was that only about 60% of patients receiving statins reached target LDLc and non-HDLc values, reflecting the shortcomings of current treatments in achieving complete control of lipid profile. This concept has been termed lipid-related residual risk. A registry of patients with ischemic heart disease established in Spain found that 30% of patients had lipid-related residual risk.40
In the field of therapy, one of the most promising strategies to reduce LDLc is pharmacologic inhibition of PCSK9 (proprotein convertase subtilisin/kexin type 9), which is involved in the breakdown of hepatic LDL receptors by monoclonal antibodies. A phase I study demonstrated that the use of these antibodies, administered subcutaneously every 15 days or 30 days, reduced the LDLc concentrations by 40% to 60%, with excellent tolerability.41 The efficacy of these agents in reducing clinical events will not be known until 2 large clinical trials scheduled to begin in 2013 have finished.
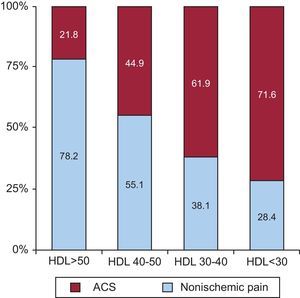
Selective cholesteryl ester transfer protein inhibitors prevent the degradation of HDL and increase its serum concentrations between 60% and 90%. However, in May 2012, the DAL-OUTCOMES clinical trial using dalcetrapib in coronary patients was stopped prematurely due to lack of efficacy. Furthermore, certain genetic mutations have been identified that lead to higher HDLc values but which are not associated with decreased CV disease risk.42 However, in a study comparing patients with chest pain admitted to a single center, HDLc levels were 22% higher in patients discharged with a diagnosis of noncoronary chest pain than in those diagnosed with acute coronary syndrome, although there were no differences in LDLc levels.43 It was also noted that the lower the mean HDLc level, the greater the prevalence of acute coronary syndrome (Fig. 2).
Relationship between high-density lipoprotein levels and acute coronary syndrome.43 ACS, acute coronary syndrome; HDL, high-density lipoprotein.
The choice of a 6.5% cutoff value of glycated hemoglobin (HbA1c) for the diagnosis of diabetes mellitus (DM) is still controversial. For many, this figure should be lower, since some patients in the 6% to 6.4% range may remain undiagnosed.44
Regarding the role of postprandial blood glucose for prognosis, a study which followed up diabetic patients over 14 years45 showed that postprandial blood glucose rather than fasting blood glucose was a predictor of both CV disease events and mortality.
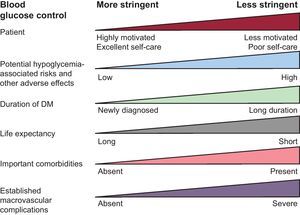
There have been changes in blood glucose targets in favor of multifactorial control. The European CV disease prevention guidelines1 recommend an HbA1c target of <7% for diabetic patients with coronary heart disease. A target below 6.5% could be useful in newly diagnosed patients and could reduce microvascular complications in patients with long-standing DM, according to results from the ADVANCE (Action in Diabetes and Vascular disease: PreterAx and DiamicroN MR Controlled Evaluation) clinical trial.46 The AHA/ACCF 2011 guidelines on secondary prevention47 recommend a general HbA1c target of <7%. These guidelines specify that a less ambitious target could be considered in patients with a history of hypoglycemia, macrovascular or microvascular disease or the presence of other comorbidities, becausemacrovascular disease—which causes more deaths in diabetic patients than does microvascular disease—appears to be less clearly affected by the intensity of blood glucose control than by adequate control of other risk factors. The American Association for Diabetes and the European Association for the Study of Diabetes emphasize the importance of individually tailoring HbA1c target values in each patient (Fig. 3).48 Moreover, serious doubts concerning the safety of setting over-ambitious targets in patients with advanced atherosclerosis have arisen from the performance of ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial,49 which was stopped prematurely due to increased mortality in the intensive treatment arm. In diabetics with heart failure, higher HbA1c levels were associated with improved survival.50 The following conclusions were established: a) greater blood glucose control does not always translate into increased benefit, and b) the best treatment for DM is strict control of CVRFs, especially blood pressure and lipids.
Blood glucose targets in diabetes mellitus should be based on individualizing treatment to each patient and assessing the role of several factors. DM, diabetes mellitus. Adapted from Zannad et al.6
Currently, there is debate on the factors that cause macrovascular disease in the context of metabolic syndrome and prediabetes. Insulin resistance before the onset of DM is defined by hyperinsulinemia and may have a causal relationship with vascular disease.51
In the pharmacologic treatment of diabetic patients with heart disease, the impact of insulin secretogogues on CV events and mortality remains a matter of debate. Recent studies have demonstrated a greater increase in mortality and CV disease events in patients taking glimepiride, glibenclamide, glipizide or tolbutamide vs those taking metformin.52 A meta-analysis of insulin has ruled out the risk of cancer with the use of insulin glargine.53
CARDIAC REHABILITATIONIt has been shown that cardiac rehabilitation programs (CRP) decrease CV mortality and total mortality, nonfatal infarction and the need for revascularization and improve quality of life compared with conventional intervention after a coronary event.54
The European guidelines on CV disease prevention1 recommend (class IIaB) that all patients who have undergone coronary revascularization (surgical or percutaneous) after an acute coronary syndrome should be referred to CRP to improve their lifestyle and adherence to drug treatment.
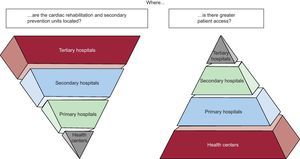
Despite the clear benefits of CRP, its use remains disappointingly low. This underuse is partly due to the low number of cardiac rehabilitation units and the lack of access to these programs; however, another important factor is that cardiologists only refer small percentages of patients to these programs, particularly women and the elderly. To address these obstacles, a consensus document by the AHA54 provides alternatives to traditional models of center-based CRP, such as conducting outpatient programs in health centers or at home. Home-based programs for low-risk patients have been recommended, because no differences were found in patient prognosis or outcome when these programs were compared with traditional center-based CRP.55
Outpatient programs for low-risk patients supervised by primary care physicians (Fig. 4) have also been included, due to better accessibility, as have distance education programs. The Spanish Society of Cardiology has published studies supporting this position56,57; these studies also demonstrate benefits in the reduction of CV disease complications and better quality of life for the patients.
The underutilization of cardiac rehabilitation programs is due to many factors; one of the most important is lack of patient access to tertiary hospitals. New models are proposed for prevention and cardiac rehabilitation centers, such as the creation of center-based programs to facilitate patient access.
Despite the worst social and economic crisis that the current generation can remember, knowledge continues to advance, as clearly reflected in this review. In addition, we are simultaneously witnessing a phase of reflection and consolidation regarding many of these advances, in which multiple strategies in the field of CV disease prevention have been analyzed and agreed upon. However, this does not disguise the fact that many gaps in the evidence remain to be filled and that there is still ample room for improvement.
CONFLICTS OF INTERESTNone declared.