Many health systems have initiated electronic consultation (e-consultation) programs, although little is known about their impact on accessibility, safety, and satisfaction. The aim of this study was to assess the clinical impact of the implementation of an outpatient care model that includes an initial e-consultation and to compare it with a one-time face-to-face consultation model.
MethodsWe selected patients who visited the cardiology service at least once between 2010 and 2019. Using an interrupted time series regression model, we analyzed the impact of incorporating e-consultation into the health care model (started in 2013), and evaluated waiting times, emergency services, hospital admissions, and mortality.
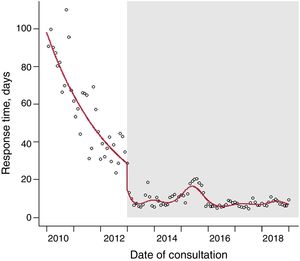
ResultsWe analyzed 47 377 patients: 61.9% were attended in e-consultation and 38.1% in one-time face-to-face consultations. The waiting time for care was shorter in the e-consultation model (median [IQR]: 7 [5-13] days) than in the face-to-face model (median [IQR]: 33 [14-81] days), P<.001. The interrupted time series regression model showed that the introduction of e-consultation substantially decreased waiting times, which held steady at around 9 days, although with slight oscillations. Patients evaluated via e-consultation had fewer hospital admissions (0.9% vs 1.2%, P=.0017) and lower mortality (2.5% vs 3.9%, P<.001).
ConclusionsAn outpatient care program that includes an e-consultation reduced waiting times significantly and was safe, with a lower rate of hospital admissions and mortality in the first year.
Keywords
The integration of electronic medical records among health care levels allows professionals at different care levels to share access to patients’ clinical information, improves communication, and enables the possible development of new clinical management modalities for outpatient care that optimize health care resources. This approach crystallizes the integration among levels by avoiding fragmentation of care and promotes coordination, continuity of care, and integrated patient management.1 All of these factors help to resolve health care problems at the appropriate care level, improve patient access to the health care system, and avoid medical acts of no value while guaranteeing safety.2 Based on these premises, the electronic medical records used by the Health Care Service of Galicia are integrated among health care levels (termed the IANUS system).
Telemedicine has been incorporated into new outpatient care management models via the inclusion of electronic consultations (e-consultations), which is a type of interconsultation between 2 medical specialists through applications or computer platforms that guarantee the security of the clinical information. Oseran et al.3 reported that patients and professionals readily accept e-consultations, which can more rapidly resolve care problems in outpatient consultations, adjust the care delay to the characteristics of the clinical problem, and reduce health care costs.
The Cardiology Service of the Integrated Health Care Area of Santiago de Compostela (ASISC) initiated one-time consultations in 2008. In this model, as an adjunct to face-to-face consultations, cardiologists perform on the same day any complementary tests required for the diagnosis of patients referred by primary care (PC) physicians to cardiology. This approach can reduce care to a single medical act and contrasts with the more classic models that include multiple patient visits for the initial consultation, for complementary tests, which are also often performed by different professionals from the treating clinic, and for a final visit to combine diagnosis and treament.4 This new one-time health care model reduces waiting times and the need for successive consultations5 and can even be more decisive when noncardiologists perform the echocardiogram outside of the hospital setting.6
In 2013, a universal e-consultation was developed and implemented, in agreement among health area managers, PC physicians, and cardiologists. This model includes a first non-face-to-face consultation (e-consultation) involving shared electronic medical records (IANUS). In all cases, the reason for the PC physician's request for the consultation was specified, as well as the cardiologist's clinical response.In patients whose needs could be met without a face-to-face consultation using the data available in the medical records, a diagnostic and therapeutic strategy was proposed to the PC physician. The other patients were referred to a one-time face-to-face consultation in which a clinical discharge or follow-up in subsequent consultations was determined by the cardiology service.
Despite the growing implementation of telemedicine consultation models, there are no data on the quality of the health care in terms of delays, prognostic impact, and patient and professional satisfaction.
The objective of our study was to compare the clinical impact of the implementation of an outpatient care model including an initial e-consultation with that of a one-time face-to-face model. As a secondary objective, we also evaluated the satisfaction of both patients and professionals with this new model.
METHODSPatientsThe ASISC provides health care coverage to 446 603 people; 352 331 are older than 14 years. This population is characterized by its considerable geographical dispersion, which involves 46 local governments. In total, 107 812 people are older than 65 years; they represent 24.2% of the regional population. To provide health care to the population older than 14 years, the health care area is equipped with 301 PC physicians, who perform their duties in 56 health care centers and 21 peripheral clinics, all functionally grouped together in 25 PC services.
The Cardiology Service of the ASISC is divided among 3 hospital centers. It responds daily to an average of 32 e-consultations with 6 cardiologists and attends about 25 face-to-face consultations with patients from e-consultations with 3 cardiologists. A team of 6 cardiologists responds to the e-consultations: 3 exclusively perform one-time face-to-face consultations and 3 rotate every 2 months with the other service specialists. These 3 cardiologists with other health care activity dedicate about 2hours of their working day to evaluating the e-consultations. For all professionals, 10minutes are allotted to each e-consultation in their schedule.
The one-time consultation model was implemented in 2008 and continued until 2012. For the present work, we selected patients from 2010 onward because the quality of the data recorded from this time is in line with that of the data recorded during the e-consultation period. Under this model, the cardiologist visit includes all complementary tests considered necessary for diagnosis (eg, electrocardiogram, echocardiogram, Holter monitoring, and cardiac stress tests). In this group, patients are referred from both PC and the different hospital services, including the emergency department.
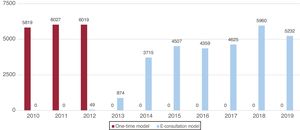
An outpatient care model was established in January 2013. This model includes an electronic consultation or e-consultation, defined by 3 characteristics: a) communication between 2 health care professionals; b) performance of both the consultation and the response in a secure electronic system and their documentation in the patients’ official medical records (IANUS); and c) the management of a specific clinical problem in the entire medical act. This e-consultation can be resolved in 1 of 3 ways: a) no face-to-face visit with the cardiologist is deemed necessary; b) the cardiologist decides that the patient requires a face-to-face examination, which is performed in a one-time consultation; and c) after the e-consultation and face-to-face consultation, subsequent follow-up by the service is chosen. This model was applicable solely to referrals from PC. Figure 1 shows the number of patients annually attended in the Cardiology Service of the ASISC.
For the present work, we selected patients referred at least once to the cardiology department from January 1, 2010, to December 31, 2019, giving a final sample of 47 377 patients.
VariablesDemographic and clinic characteristics were acquired, as well as the consultation modality used to manage each patient. To assess the impact of the e-consultation, the following variables were analyzed: health care delay, emergency department attendance, hospital admission, and mortality in the first postconsultation year. The cause of death was available for patients who died in hospital (6965 patients).
In addition, for AENOR reaccreditation purposes, patient and professional satisfaction was evaluated in 2019 using a specific questionnaire.
Statistical analysisContinuous variables are expressed as mean ± standard deviation or, if nonnormally distributed, as median [interquartile range]. Chi-square and Mann-Whitney U tests were used to determine the presence of differences between the consultation models (one-time or e-consultation). SPSS statistical software version 22.0 (SPSS Inc, United States) was used to analyze these data. Interrupted time series analysis7 was applied to assess the impact of the e-consultation on health care delays, emergency department attendance, and mortality in the first year after the first consultation.
To analyze mortality, emergency department attendance, and hospital admissions, the denominators were the consultations performed in each month. Poisson regression models were used to test the hypothesis that the e-consultation model would have lower rates. The rates were directly modeled with a log-linear model including all events (emergencies, hospitalizations, deaths) as the dependent variable and monthly consultations as the offset.
To analyze the consultation delay, a log-normal distribution regression model was used for the dependent variable, with the effect of the time-consultation model interaction (with time calculated from study initiation) adjusted with a generalized additive model with splines.
The adjusted models considered seasonality, autocorrelation, overdispersion, and linearity. For data analysis, we used R program version 4.0.3, freely distributed in CRAN-R.8
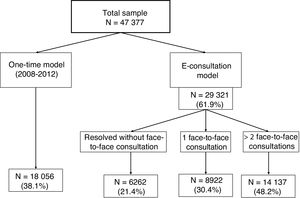
RESULTSA total of 47 377 patients were attended in the study period (38.1% under the one-time consultation model and 61.9% under the e-consultation model). Of those attended via e-consultation, 21.4% did not require a face-to-face consultation, 30.4% required 1 face-to-face consultation, and 48.2% required 2 or more face-to-face consultations (figure 2).
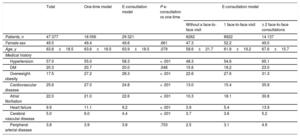
The characteristics of the patients attended by care model are shown in table 1. There were no differences in age or sex between the 2 models. However, the patients attended via the one-time model exhibited a higher frequency of comorbidities than those attended via the e-consultation model. Older patients and those with more comorbidities required a higher number of face-to-face consultations.
Clinical and epidemiological characteristics of the 4 groups analyzed
| Total | One-time model | E-consultation model | P e-consultation vs one-time | E-consultation model | |||
|---|---|---|---|---|---|---|---|
| Without a face-to-face visit | 1 face-to-face visit | ≥ 2 face-to-face consultations | |||||
| Patients, n | 47 377 | 18 056 | 29 321 | 6262 | 8922 | 14 137 | |
| Female sex | 49.5 | 49.4 | 49.6 | .661 | 47.3 | 52.2 | 49.0 |
| Age, y | 63.8±18.5 | 63.6±18.5 | 63.9±18.5 | .079 | 58.6±21.7 | 61.8±19.2 | 67.6±15.7 |
| Medical history | |||||||
| Hypertension | 57.0 | 55.0 | 58.3 | < .001 | 48.3 | 54.6 | 65.1 |
| DM | 20.3 | 20.7 | 20.0 | .048 | 15.6 | 18.2 | 23.0 |
| Overweight-obesity | 17.5 | 27.2 | 28.3 | < .001 | 22.6 | 27.6 | 31.3 |
| Cardiovascular disease | 25.6 | 27.0 | 24.8 | < .001 | 13.0 | 15.4 | 35.9 |
| Atrial fibrillation | 22.0 | 21.0 | 22.6 | < .001 | 10.3 | 18.1 | 30.8 |
| Heart failure | 9.9 | 11.1 | 9.2 | < .001 | 3.9 | 5.4 | 13.9 |
| Cerebral vascular disease | 5.0 | 6.0 | 4.4 | < .001 | 3.7 | 3.6 | 5.2 |
| Peripheral arterial disease | 3.8 | 3.9 | 3.8 | .703 | 2.5 | 3.1 | 4.9 |
DM, diabetes mellitus.
Data are expressed as percentage or mean ± standard deviation.
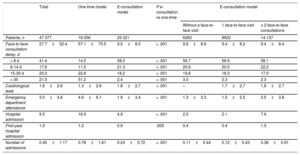
Table 2 shows data related to the consultation delay, tests performed, emergency department attendance, and hospital admission. Delays were significantly decreased with the e-consultation model vs the one-time model, with medians of 7 [5-13] and 33 [14-81] days, respectively (P < .001). The e-consultation model also showed significantly lower rates of emergency department attendance and hospital admission.
Safety criteria in each consultation model
| Total | One-time model | E-consultation model | P e-consultation vs one-time | E-consultation model | |||
|---|---|---|---|---|---|---|---|
| Without a face-to-face visit | 1 face-to-face visit | ≥ 2 face-to-face consultations | |||||
| Patients, n | 47 377 | 18 056 | 29 321 | 6262 | 8922 | 14 137 | |
| Face-to-face consultation delay, d | 27.7±52.4 | 57.1±75.5 | 9.5±8.5 | < .001 | 9.9±8.8 | 9.4±8.2 | 9.4±8.4 |
| < 8 d | 41.4 | 14.5 | 58.0 | < .001 | 56.7 | 58.9 | 58.1 |
| 8-14 d | 17.6 | 11.5 | 21.3 | < .001 | 20.6 | 20.5 | 22.2 |
| 15-30 d | 20.0 | 22.8 | 18.2 | < .001 | 19.8 | 18.3 | 17.5 |
| > 30 | 21.0 | 51.2 | 2.4 | < .001 | 3.0 | 2.3 | 2.3 |
| Cardiological tests | 1.6±2.6 | 1.3±2.6 | 1.8±2.7 | < .001 | – | 1.7±2.7 | 1.8±2.7 |
| Emergency department attendance | 3.0±4.8 | 4.8±6.1 | 1.9±3.4 | < .001 | 1.3±3.3 | 1.5±2.5 | 2.5±3.8 |
| Hospital admission | 9.5 | 16.9 | 4.9 | < .001 | 2.0 | 2.1 | 7.9 |
| First-year hospital admission | 1.0 | 1.2 | 0.9 | .005 | 0.4 | 0.4 | 1.5 |
| Number of admissions | 0.45±1.17 | 0.78±1.61 | 0.24±0.72 | < .001 | 0.11±0.44 | 0.12±0.43 | 0.38±0.91 |
Data are expressed as percentage or mean ± standard deviation.
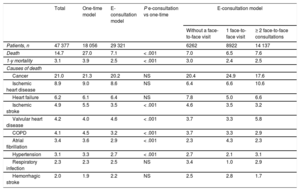
Table 3 shows the mortality and cause of death data of the patients who died in the hospital. Mortality was significantly lower in those attended via e-consultation.
Deaths in each consultation model
| Total | One-time model | E-consultation model | P e-consultation vs one-time | E-consultation model | |||
|---|---|---|---|---|---|---|---|
| Without a face-to-face visit | 1 face-to-face visit | ≥ 2 face-to-face consultations | |||||
| Patients, n | 47 377 | 18 056 | 29 321 | 6262 | 8922 | 14 137 | |
| Death | 14.7 | 27.0 | 7.1 | < .001 | 7.0 | 6.5 | 7.6 |
| 1-y mortality | 3.1 | 3.9 | 2.5 | < .001 | 3.0 | 2.4 | 2.5 |
| Causes of death | |||||||
| Cancer | 21.0 | 21.3 | 20.2 | NS | 20.4 | 24.9 | 17.6 |
| Ischemic heart disease | 8.9 | 9.0 | 8.6 | NS | 6.4 | 6.6 | 10.6 |
| Heart failure | 6.2 | 6.1 | 6.4 | NS | 7.8 | 5.0 | 6.6 |
| Ischemic stroke | 4.9 | 5.5 | 3.5 | < .001 | 4.6 | 3.5 | 3.2 |
| Valvular heart disease | 4.2 | 4.0 | 4.6 | < .001 | 3.7 | 3.3 | 5.8 |
| COPD | 4.1 | 4.5 | 3.2 | < .001 | 3.7 | 3.3 | 2.9 |
| Atrial fibrillation | 3.4 | 3.6 | 2.9 | < .001 | 2.3 | 4.3 | 2.3 |
| Hypertension | 3.1 | 3.3 | 2.7 | < .001 | 2.7 | 2.1 | 3.1 |
| Respiratory infection | 2.3 | 2.3 | 2.5 | NS | 3.4 | 1.0 | 2.9 |
| Hemorrhagic stroke | 2.0 | 1.9 | 2.2 | NS | 2.5 | 2.8 | 1.7 |
COPD, chronic obstructive pulmonary disease; NS, not significant.
Unless otherwise indicated, the data are expressed as percentages.
During the one-time model period, there was a gradual reduction in delays, which fell abruptly upon implementation of e-consultation and were thereafter maintained at about 9 days, although with slight oscillations (figure 3).
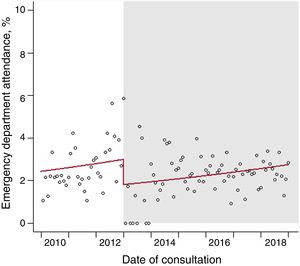
Emergency department attendance at 1 postconsultation yearDuring the one-time model period, there was a slight increase in the rate of emergency department attendance of 0.6% (95% confidence interval [95%CI], 0.2%-1.0%) (figure 4). This rate fell by 51% (95%CI, 23%-79%) upon e-consultation implementation, although the previous monthly growth rate resumed.
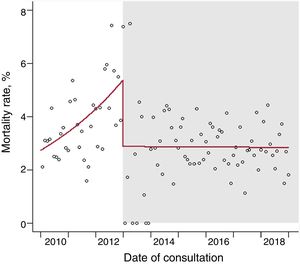
Mortality at 1 postconsultation yearDuring the one-time model period, there was a slight increase in mortality rates, with a monthly increase of 1.9% (95%CI, 1.2%-2.7%) (figure 5). This rate fell upon e-consultation implementation and held steady thereafter.
Patient and PC physician satisfaction was regularly surveyed. The health care professional survey was distributed online to all PC physicians; 129 responded (response rate, 42.86%). They believed the response time to be appropriate or highly appropriate (69.0%) and that the program improved communication (70.6%), helped to resolve diagnostic doubts (70.5%), and was effective for the diagnostic and therapeutic management of cardiology patients (73.6%). The patient survey was distributed in person to 325 consecutive patients who attended the first visit in the cardiology service (response rate, 87.0%). The results showed that they were satisfied or very satisfied with the waiting times (92%), with the clarity of information concerning appointments (98%), and with the communication between their PC physician and cardiologist (88%) and that they considered the care received to be satisfactory (99%). In total, 81% of patients surveyed said that they were very satisfied with the care provided in the cardiology consultation; 7% were satisfied and 12% were unsatisfied. Moreover, they reported a general satisfaction with the care received of 94%. In addition, during the 4-year period of the one-time face-to-face model, some complaints were recorded concerning the waiting times, whereas no such complaints were received after the initiation of the model involving e-consultation.
DISCUSSIONHere, we describe the results of a universal e-consultation program in a cardiology service for referrals made by PC physicians. The clinical characteristics of the patients were similar in the 2 outpatient care models (table 1). Our data show that the implementation of an e-consultation program in the outpatient care model effectively reduces waiting times and is safe, with a significant reduction in emergency department attendance, hospital admissions, and mortality. In addition, the model incorporating e-consultation allows identification of a group of less complex patients who do not require face-to-face care.
As far as know, this is the first description of the outcomes of a program for managing outpatient care demand in a cardiology service that incorporates e-consultation. We believe that our design could serve as an outpatient care model, at least for health care areas with integrated medical records among care levels because, in addition to promoting communication between PC physicians and cardiologists, the program improves health care access and patient prognosis. In addition, it permits optimization of available health care resources, avoiding medical acts with no value and promoting the resolution of clinical problems at the appropriate care level.
A recent meta-analysis analyzed the characteristics and outcomes of different cardiology e-consultation programs in the United States and Canada. The results indicated that initiatives incorporating telemedicine generally improve access to specialized care and reduce costs by limiting medical acts, complementary tests, and patient travel.3 In that analysis, 4 basic prerequisites needed to be met for the system to be considered an e-consultation program: a) communication between at least 2 health care professionals; b) asynchronous communication; c) performance of both the consultation and response in a secure electronic system, as well as their documentation in patients’ official medical records; and d) management of a specific clinical issue in the entire medical act.3 All of these elements are present in our care model incorporating e-consultation. In addition, most publications in the meta-analysis were from the same group (Liddy et al.) and no European experience was included.
The results have been reported of 2 randomized clinical trials comparing e-consultation with traditional outpatient care. By analyzing a group of 590 patients, Anderson et al.9 showed a reduction in associated costs for an e-consultation program with lower use of outpatient procedures than in a group of patients randomized to the conventional model; they estimated a reduction of 466 dollars per patient compared with the face-to-face consultation. Based on the same clinical trial, Olayiwola et al.10 and Wasfy et al.11 did not detect a higher incidence of complications in the group of patients randomized to the e-consultation program, although their analyses were limited to a subgroup of patients included in an electronic medical record system. In our experience, the incorporation of e-consultation into the outpatient care management program of our cardiology service was associated with improved patient prognosis.
In Spain, Hernández-Afonso et al.12 described the characteristics of a virtual cardiology care program that showed the resolution, without face-to-face consultation, of 30% of referrals to their cardiology service, results that are slightly better than those seen in our program. In addition, both approaches enabled a marked improvement in accessibility to health care services, with notable reductions in health care delays, outcomes similar to those described in an observational study13 and in the clinical trial by Olayiwola et al.10
Our results show that an initial telemedicine consultation-based assessment can identify patients with lower clinical complexity who do not require a face-to-face visit and can reduce waiting times for a one-time face-to-face consultation in more complex patients. This improved access to health care can reduce the need for emergency department visits, complications requiring admission, and mortality. In our model, the availability of clinical information in the electronic medical records, in addition to the results of complementary tests, undoubtedly facilitates the resolution of health care demand and probably reduces health care costs.
LimitationsAlthough we acknowledge certain limitations in the analysis of our results, the experience described in this large cohort of patients with demographic, clinical, and prognostic information integrated in an electronic medical record system strengthens the relevance of the clinical and health care management aspects of our findings. In addition, an interrupted time series analysis is the best option for quasiexperimental studies to estimate the effect of an intervention in nonrandomized studies. In contrast to cross-sectional studies, this type of analysis can control for trends in place before the event of interest while studying the dynamics of the change related to the intervention. Another strong point of this analytical approach is that it enables intuitive visualization of the dynamics of the response to an intervention, in this case the inclusion of e-consultation in outpatient cardiological management, and can thereby show if the effects are immediate or delayed and temporary or persistent. In addition, the analysis of patient and professional satisfaction supports the general acceptance of a health care model that includes telemedicine.
A possible information bias related to the retrospective analysis of data with limited access to the cause of death might explain some of our findings, although information was available on all deaths occurring during our follow-up period. In addition, we were unable to identify the contacts of patients with health care professionals outside of the public health care system of our health care area, which may have also affected our results. However, the impact of this factor in our area would be very small due to the low implementation of private health care systems, which is 8 points lower than the national average.14
CONCLUSIONSAn outpatient care program in a cardiology service that includes e-consultation improves access to health care and thereby reduces waiting times for specialized care. This model is safe and is associated with lower rates of emergency department attendance, hospital admission, and mortality in the first year vs a one-time face-to-face care program. We believe that our experience could help in the design of outpatient care management programs that improve health care access and patient prognosis.
- -
Few data are available on outpatient care management models in cardiology. The most often analyzed consultation model in cardiology is the one-time consultation, with all tests performed on the same day. Although there are reported experiences with e-consultation, the studies only report data on waiting list reductions and degree of satisfaction.
- -
We report the results of an outpatient care management model that includes e-consultation. Implemented in our health care area, it improved access to specialized care and was associated with lower rates of emergency department attendance, hospital admission, and mortality. Our results indicate that the implementation of a model with these characteristics would improve the efficiency of the outpatient care process in cardiology.
The authors report no conflicts of interest in relation to this article.
We thank Dr Francisco Gude Sampedro of the Clinical Epidemiology Unit of the Health Research Institute of Santiago de Compostela (IDIS) for advice and help with the statistical analysis and manuscript drafting.