To assess the impact of a program integrating cardiology and primary care in clinical practice, compared with usual care. The integrated care consists of a hospital cardiologist in each primary care clinic, shared clinical history, joint practice guidelines, consultation sessions, and other coordinating tools.
MethodsObservational, cross-sectional study of 2 series of chronic outpatients: conventional and integrated care. We analyzed patient distribution and the impact on good clinical practice indicators in patients with ischemic heart disease, heart failure and atrial fibrillation, along with primary care practitioner satisfaction and use of resources.
ResultsWe included 3194 patients (1572 usual care, 1622 integrated care). Integrated care changed the patient distribution, allowing the cardiologist to focus on serious pathologies while cardiovascular risk factors and stable patients were monitored in primary care. In ischemic heart disease, improvement was observed in cholesterol management and blood pressure control; optimal medical treatment was more frequently prescribed and ventricular function evaluated more often. In heart failure, β-blockers treatment increased and functional class was assessed more often. In atrial fibrillation, an increase in anticoagulation prescription and echocardiography evaluation was observed. Satisfaction parameters improved with integrated care. The use of resources was not increased.
ConclusionsUsing our integration model, follow-up and chronic treatment of patients with ischemic heart disease, heart failure, and atrial fibrillation were improved. Monitoring of chronic patients was redistributed between primary care and cardiology, and family physicians’ satisfaction levels improved. There was no increase in use of resources.
Keywords
Outpatient care of patients with heart disease has traditionally been based on a model of three separate levels of care. At opposite ends of the spectrum are the primary care team and the hospital cardiologist. In between is the outpatient or “district” cardiologist. For years, communication between these levels has been limited and not very fluid, being based solely on consultation reports with limited information, medical records only in certain cases and, usually, the comments of the patients themselves. The patient has 3 separate medical histories at the same time, with the resulting extra effort and repeated complementary tests and delays in diagnosis. Patients are required to visit multiple offices, and clinical practice may be uneven. Despite great progress in diagnostic and therapeutic techniques, the organization of outpatient care for patients with heart disease has not changed substantially in years.
In our current health care system, hospital physicians are to a certain extent unaware of what is done in primary health care and resources are concentrated in the acute phase of the disease. Specialists often have to deal with successive routine visits of patients initially referred for a one-time consultation. This unnecessary follow-up is often due to inertia or lack of awareness of the work of the family physician.1, 2, 3 Consensus protocols for referrals and joint, coordinated follow-up are still uncommon.
New models have been proposed in search of greater efficiency in the management of outpatients, such as one-stop consultations4, 5 or models that try to integrate primary and specialist health care.6 Integration between levels of care is an organizational response that aims to connect the different players in health care to avoid fragmentation and encourage continuity.6, 7, 8 An integrated care model should improve care,9, 10 but there is still no evidence that integrated care increases adherence to clinical guidelines or improves practice in our health system.
Our study was intended to assess the impact on clinical practice of a new model of integration between primary health care and cardiology in an urban area with a university reference hospital. The objectives were as follows: a) to assess the impact of integration on adherence to clinical guidelines in follow-up for ischemic heart disease, heart failure, and atrial fibrillation; b) to assess the change in diseases that require long-term follow-up by cardiology; and c) to assess the impact of organizational changes on physician satisfaction in primary health care, and d) to determine whether integration was accompanied by increased use of resources.
METHODS Study Population and PeriodThis observational study of outpatients requiring long-term follow-up analyzed 2 patient groups, recruited before (conventional care) and after the intervention (integrated care). In both periods, patients were included consecutively during their visit to the cardiologist.
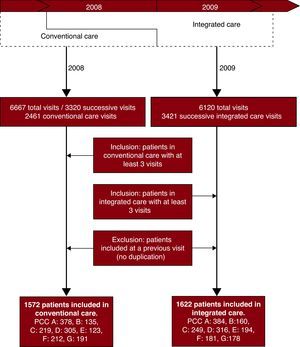
In January 2008, integrated care was implemented in the primary care centers (PCC), but the specialized centers continued the traditional model of long-term outpatient monitoring for 1 year, including these patients in the baseline sample of the study. From January through December 2009, 1 year after implementing integrated care, patients were included who were in long-term follow-up by the cardiologist under the integrated model. Long-term follow-up was defined as at least 3 patient visits under the corresponding model. We obtained an unduplicated sample; ie, patients included in the baseline sample were not included in the second. The distribution of patients is presented in Figure 1. Patient inclusion and data collection were performed by the cardiologist during the consultation. The data were subsequently reviewed by a researcher.
Figure 1. Flow diagram for patient selection. PCC, primary care center.
An inclusion period of 1 year was established for each sample, as patients in long-term follow-up would have had at least 1 consultation in this period. The 2 samples (ie, before and after the intervention) were recruited in consecutive years in order to be able to attribute any changes largely to the model of care and not to changes in clinical practice over time.
The patients were recruited from 7 PCC which, prior to integrating care, followed a conventional model of specialty care by the cardiologist assigned to the district. Districts were not included that, prior to integration, contracted with a hospital for cardiology follow-up with a hospital or were managed by the hospital itself.
The study was approved by the ethics committee of each participating hospital.
Study InterventionThe effects of the change of organizational model from conventional specialty care to one of integrated care were studied.
Conventional care (baseline sample): Specialty care in cardiology was performed in a specialized outpatient clinic other than the PCC or hospital. The cardiologists did not have any links with the hospital, were permanent or interim employees in the Spanish national health system, and usually worked 2h per day, 3 days per week. The medical histories were in hardcopy format and separate from the medical records of the PCC and the hospital. The total number of cardiology care hours in the areas studied was 42 per week. Communication between the family physicians and the hospital was by means of referral reports.
Integrated care (intervention): A hospital cardiologist was integrated into each primary care team while also performing hospital tasks. A working group analyzed the most prevalent diseases responsible for referral for integrated follow-up and agreed on the criteria for referral and the coordinated management between cardiologist and primary health care. Follow-up of patients with the most prevalent heart diseases was coordinated between the family physician and the hospital cardiologist, who visited the PCC once a week, using new tools for coordination and communication. The characteristics of the integrated model are presented in Table 1. The total time spent by the cardiologist for the districts studied was the same as for the conventional model (42h/week: 5 office h plus 1 h of consultation for each PCC). Therefore, the differences in hours spent and workload depended on the organizational model and not the staff availability.
Table 1. Characteristics of the Integrated Care Model in Cardiology.
| 1. | Cardiologists integrated into the primary care team (they travel to the consultation in the primary care center) |
| 2. | Shared electronic medical records |
| 3. | Weekly consultation session |
| 4. | Cell phone and e-mail for consultations |
| 5. | Agreed pathways for redistributing patient care between primary and specialist care |
| 6. | Consensus clinical guidelines for ischemic heart disease, heart failure, atrial fibrillation, and valve disease |
| 7. | Web page for improved communication and consultations: www.ais-bcn.es |
| 8. | Cardiologist has the same complementary tests available as in the hospital clinic |
| 9. | Theoretical and practical training sessions for continued medical education for primary care and shared care course |
| 10. | Nursing link for coordination of follow-up after discharge from hospital |
| 11. | Electronic platform for transmission of documents from the hospital to the integrated medical records |
In each case, the main reason why the patient remained in long-term cardiology follow-up was recorded according to the defined criteria to assess the impact of integration on the profile of patients in follow-up in each care model. In the event of multiple diagnoses in the same patient, the most clinically relevant one was selected, following the pre-established definitions. For the 3 conditions indicating long-term follow-up in the integrated model (ischemic heart disease, heart failure, and atrial fibrillation), the following variables were established to analyze the differences between conventional care and integrated care:
– Ischemic heart disease:11, 12, 13, 14, 15, 16, 17 Indication of antiplatelet therapy, β-blockers, renin-angiotensin system inhibitors (RASI), and statins. Performance of cardiac catheterization and/or revascularization. Documentation of ventricular function, low-density lipoprotein cholesterol <100mg/dL, and optimum control of blood pressure.
– Chronic heart failure:10, 11, 18 Performance of echocardiography. Evaluation of functional class. Indication of treatment with RASIs and β-blockers. Anticoagulants in patients with associated atrial fibrillation.
– Atrial Fibrillation:19, 20, 21 performance of echocardiography. Indication for anticoagulants.
The study variables were selected to assess the degree of adherence to clinical guidelines, especially with regard to parameters associated with improved prognosis for the patients.
Data Collection and Statistical AnalysisData were collected by reviewing the medical record of conventional specialist care in consecutive visits of the patients recruited in the first inclusion period and analyzing the integrated care history in consecutive visits to the cardiologist in the second period. The data were analyzed with the SPSS 16.0 program to determine the statistical differences between the study variables before and after integration. Categorical variables were expressed as absolute numbers and percentages; quantitative variables were expressed as means (standard deviation). Statistical analysis was performed using the χ2 test or the Fisher test for categorical variables and the Student t test for quantitative variables. To control for possible type I errors, a logistic regression analysis was applied for each dimension studied and the results were obtained in the form of odds ratios (OR).
Satisfaction of the Physicians in Primary CareAn anonymous survey of family physicians was used to assess satisfaction with the conventional model (prior to integration) and with the integrated model (1 year after implementation). The survey, using an analog scale of 0 to 10, consisted of questions on overall satisfaction and specific satisfaction with respect to resolution of problems, communication, access of the primary care physician to the cardiologist, information received by the patients, and patient access to the specialist. Data were presented as means (standard deviation) and the k concordance index was determined for the analysis.
Resource UsageTo assess whether the organizational change was accompanied by a change in resource usage, information was obtained on the number of complementary tests (echocardiograms, stress tests, and Holter tests) requested by the cardiologists in the year prior to and after integration, referrals to hospital outpatient clinics, and hospital admissions of patients from the PCC studied. These data were obtained from the administrative records of the hospital and the PCC.
RESULTSA total of 3194 patients were included, 1572 corresponding to the period of conventional care and 1622 to integrated care. The mean age was 72.8 (11.4) years and 55% were men.
Distribution of DiseasesThe diseases responsible for the long-term patient follow-up are presented in Table 2. Ischemic heart disease was the main reason for follow-up in both periods, but the proportion increased significantly after integration. Of note during the conventional care period was the considerable number of patients who were in follow-up for cardiovascular risk factors, with no associated heart disease, due to the electrocardiogram (ECG) findings in asymptomatic patients. After integration, the reasons for long-term follow-up essentially changed to those agreed upon as the clinical pathways: ischemic heart disease, heart failure, valve disease, and atrial fibrillation. Monitoring of risk factors became the responsibility of primary health care and the number of cardiology consultations decreased. Follow-up of insignificant ECG abnormalities almost disappeared as these cases were resolved during consultation sessions.
Table 2. Diagnoses Responsible for Long-term Follow-up by Cardiology According to the Conventional and Integrated Model.
| Variable | Univariate analysis | ||
| Conventional care (n=1572) | Integrated care (n=1622) | P | |
| Increase after integration | |||
| Ischemic heart disease | 439 (27.9) | 689 (42.5) | < .001 |
| Heart failure | 83 (5.3) | 219 (13.5) | < .001 |
| Valve disease | 138 (8.8) | 242 (14.9) | < .001 |
| Hypertrophic cardiomyopathy | 14 (0.9) | 35 (2.2) | .004 |
| Decrease after integration | |||
| Atrial fibrillation | 290 (18.4) | 223 (13.7) | < .001 |
| Management of risk factors without associated heart disease | 307 (19.5) | 73 (4.5) | < .001 |
| ECG findings in asymptomatic patients | 83 (5.3) | 1 (0.1) | < .001 |
| No change after integration | |||
| Syncope | 25 (1.6) | 37 (2.3) | NS |
| Bradyarrhythmias | 33 (2.1) | 42 (2.6) | NS |
| Other reasons for long-term follow-up | 160 (10.1) | 61 (3.7) | — |
ECG, electrocardiogram.
Data are presented as n (%).
The main reason for long-term follow-up in all patients was ischemic heart disease, although this percentage increased with integrated care. After integration, better control of cholesterol (OR=5.9), more statin treatment (OR=5.6), better control of blood pressure (OR = 2.3), documentation of ejection fraction (OR=3), and optimized medical treatment (OR=1.7) were reported (Table 3).
Table 3. Results in Patients With Ischemic Heart Disease.
| Variable | Univariate analysis | Logistic regression model | |||
| Conventional care (n=439) | Integrated care (n=689) | P | Adjusted OR (95% CI) | P | |
| Age, years | 72 (10.4) | 72 (11.1) | NS | — | — |
| Men | 327 (74.5) | 519 (75.4) | NS | — | — |
| Antiplatelets | 390 (88.8) | 666 (96.4) | < .001 | 1.7 (0.9-3.1) | .1 |
| β-blockers | 275 (55.8) | 562 (81.7) | < .001 | 1.45 (1-2.2) | .075 |
| RASI | 235 (53.5) | 533 (77.5) | < .001 | — | — |
| Statins | 297 (67.7) | 663 (94.4) | < .001 | 5.6 (3.3-9.6) | < .001 |
| Optimal treatment a | 169 (22.6) | 419 (60.9) | < .001 | 1.7 (1.2-2.6) | .007 |
| Catheterization+revascularization | 260 (52.9) | 513 (73.3) | < .001 | — | — |
| Documented ejection fraction | 190 (43.3) | 524 (76.2) | < .001 | 3.0 (2.2-4.1) | < .001 |
| LDL-C < 100 mg/dL | 99 (22.6) | 498 (72.4) | < .001 | 5.9 (4.3-8) | < .001 |
| Optimal blood pressure | 245 (55.8) | 574 (83.4) | < .001 | 2.3 (1.6-3.3) | < .001 |
CI, confidence interval; LDL-C, low-density lipoprotein cholesterol; NS, not significant; OR, odds ratio; RASI, renin-angiotensin system inhibitors. Data from the univariate analysis are expressed as n (%), except for age, which is expressed as mean (standard deviation).
a Antiplatelets+β-blocker+RASI+statin.
Integrated care increased the number of patients in follow-up for heart failure. Logistic regression analysis revealed that integrated care improved documentation of functional class (OR=196) and treatment with β-blockers (OR=3.7) (Table 4).
Table 4. Results in Patients With Heart Failure.
| Variable | Univariate analysis | Logistic regression model | |||
| Conventional care (n=83) | Integrated care (n=220) | P | Adjusted OR (95% CI) | P | |
| Age, years | 76.1 (10.5) | 75.5 (9.9) | NS | — | — |
| Women | 47 (56.6) | 121 (55.9) | NS | — | — |
| Echocardiogram | 75 (90.4) | 216 (98.2) | .02 | — | — |
| Decreased ejection fraction | 42 (50.6%) | 137 (62.3) | .004 | — | — |
| RASI | 66 (79.5) | 210 (95.5) | < .001 | — | — |
| β-blockers | 33 (39.8) | 171 (77.7) | < .001 | 3.7 (1.5-9.4) | .006 |
| Optimal treatment a | 27 (32.5) | 163 (74.1) | < .001 | — | — |
| Functional class assessed | 16 (19.3) | 218 (98.2) | < .001 | 196 (61.8-619.7) | < .001 |
| Anticoagulation in event of AF | 35 (85.4) | 133 (93.7) | NS | — | — |
AF, atrial fibrillation; CI, confidence interval; NS, not significant; OR, odds ratio; RASI, renin-angiotensin system inhibitors.
Data from the univariate analysis are expressed as n (%), except for age, which is expressed as mean (standard deviation).
a RASI+β-blocker.
The number of echocardiographic studies increased significantly (OR=1.9) and the indication for anticoagulation therapy (OR=7.1) also increased significantly (Table 5). Integration was associated with a reduction in the number of patients who required long-term follow-up by the cardiologist.
Table 5. Results in Patients With Atrial Fibrillation.
| Variable | Univariate analysis | Logistic regression model | |||
| Conventional care (n=290) | Integrated care (n=223) | P | Adjusted OR (95% CI) | P | |
| Age, years | 78.1 (8.1) | 75.9 (8.5) | .003 | — | — |
| Women | 154 (53.1) | 120 (53.8) | NS | — | — |
| Echocardiogram | 208 (71.7) | 191 (85.7) | < .001 | 1.9 (1.2-3.1) | .008 |
| Anticoagulation | 201 (69.3) | 211 (94.6) | < .001 | 7.1 (3.8-13.5) | < .001 |
CI, confidence interval; NS, not significant; OR, odds ratio.
Data from the univariate analysis are expressed as n (%), except for age, which is expressed as mean (standard deviation).
The PCC of origin did not have a significant influence on the results for the 3 diseases studied.
Satisfaction of the Physicians in Primary CareResponses were obtained from 101 family physicians in the survey of conventional care and from 103 in the integrated care survey (Table 6). An improvement was observed in both the overall satisfaction and in terms of information, problem resolution, and, especially, aspects of communication and access from primary care to the cardiologist.
Table 6. Results of Satisfaction Questionnaires Administered to Primary Care Physicians.
| Conventional care (n=101) | Integrated care (n=103) | k | |
| Are you satisfied with the established pathways for patient access to the cardiologist? | 5.4 (2.8) | 6.1 (2.6) | 0.002 |
| Are you satisfied with the information your patients receive from the cardiologist? | 3.6 (3) | 7.5 (2) | 0.004 |
| How would you assess the accessibility to the cardiologist for primary health care professionals? | 3.8 (2.9) | 7.3 (2.4) | 0.005 |
| How would you assess communication with the cardiologist? | 2.6 (2.6) | 8 (2.2) | 0.015 |
| Are you satisfied with the outcomes and orientation of the cases consulted with the cardiologist? | 4.5 (2.9) | 7.8 (2) | 0.02 |
| How satisfied are you in general with the current specialist care system in cardiology? | 4 (2.4) | 7.4 (2) | 0.006 |
Questions were answered on a scale of 0 (not at all satisfactory) to 10 (fully satisfied). Data are expressed as mean (standard deviation).
k <0.2 indicates low agreement between the results for conventional and integrated care.
For patients attended by the cardiologist in the districts studied, there was a decrease in requests for complementary tests in the first full year of integration compared with the last full year of conventional care. Requests for echocardiography decreased from 1081 to 701 (–35.1%); for Holter monitoring from 311 to 192 (–38.2%); isotope stress tests from 303 to 177 (–41.5%); and conventional stress tests from 220 to 44 (–80%). The number of referrals by the outpatient cardiologist to a hospital outpatient clinic was 349 with conventional care and only 20 after integration (a decrease of −94.9%). There was no increase in the number of admissions to hospital for cardiovascular disease in patients of the PCC studied (441 vs 430 admissions/year).
DISCUSSIONOur study shows that integrated care can optimize the distribution of care of long-term patients between family physicians and cardiologists. After integration, the diseases responsible for long-term follow-up by the cardiologist were those agreed to in the guidelines: ischemic heart disease, heart failure, valve disease, and atrial fibrillation. The primary care team takes on a lead role in the long-term follow-up of stable patients, with the cardiologist as consultant. Previous studies have shown that care of cardiovascular patients can benefit from cardiologist involvement, both directly as the persons responsible and as cardiovascular consultants.22, 23 Weekly sessions in the office, shared medical records,24 and access to the cardiologist for the family physician allow direct resolution of cases in primary care, with the specialist consultations being reserved for the most needy patients, previously defined in joint guidelines. The consultancy sessions are an essential element of integration because, in addition to discussion of cases, they encourage close communication between the cardiologist and family physicians, and they also become a teaching tool.
Chronic ischemic heart disease was the most frequent reason for long-term follow-up in cardiology clinics and this reason increased as a percentage after integration. Previous studies indicate that adherence to clinical practice guidelines does not meet the desired goals.14, 17, 25 Our study shows that integrated care was associated with an improvement in the parameters studied, particularly in the case of statin therapy, cholesterol monitoring, blood pressure monitoring, recording of the ejection fraction, and optimized medical treatment.
In heart failure, integrated care increased the number of patients in follow-up with respect to the conventional system. Integration may make it easier to identify patients with serious disease who stand to benefit from coordinated specialist management. In the conventional model, such patients may be lost among the 3 separate levels of care. The effect of the intervention is shown by the better reporting of the functional class and the increased prescription of β-blockers, which were used at an appropriate level for ideal clinical practice, compared to those reported in Spanish practice.26, 27, 28, 29
In atrial fibrillation, the integrated model makes it possible to reduce the number of patients who require long-term follow-up with the cardiologist, given that consensus guidelines state that stable patients can be followed up directly by the family physician, with the cardiologist as consultant. In patients in follow-up with the cardiologist, of note was the impact on the indication of anticoagulants and the increase in diagnostic echocardiograms, which were at acceptable levels with respect to previous studies.30
Integration was not accompanied by an increase in resource usage for the health system. The number of hours that the cardiologist dedicated to each PCC was maintained and the number of requests for complementary tests decreased in absolute terms. The number of referrals from the outpatient cardiologist to the hospital clinic also decreased and duplication of specialist care was avoided.
It is difficult to discern which aspects of the model of integrated care had most influence on the changes in clinical practice observed. Drafting of clinical guidelines, agreed upon by players in the integration of levels of care within the districts, may increase adherence to the recommendations. Shared medical records are essential and help in patient follow-up, as the cardiologist can access information from primary care (analysis, monitoring of risk factors by nursing staff, treatment, and complementary tests). Such sharing also provides a means whereby the family physicians and nursing staff can seek the opinions of a specialist. This avoids duplicate tests and optimizes the prescription of medication. Direct communication between primary care professionals and specialists and the consultancy sessions are also essential and ensure rigorous patient follow-up by the cardiologists, as what they do is seen by the family physicians and taken as an example to be followed. Another aspect to consider is that the cardiologist has the same complementary tests and indications for procedures available in the outpatient clinic as in the hospital clinic. This allows the cardiologists to perform their work and appropriately monitor complex cases.
Integration favors the sharing of responsibility for coordination of care procedures between the clinical cardiologist and the family physician.24, 31 In a health system that is looking to better utilize its resources, cooperation is required between different professionals who deal with a common disease or process, and the patient should be at the center of the process. In this multidisciplinary work, cardiologist and family physician share the leadership. In our model, a clinical group is formed with the participation of professional physicians and primary care and hospital nurses to guarantee coordination, draft joint guidelines and protocols, encourage professional relationships, and incentivize teaching and research activities.
Our study shows that the satisfaction of family physicians increases with integrated care. Although integration increases the workload in primary health care, it elevates the work of the family physicians who, with the cardiologist as a consultant, take on a lead role that allows them to improve the care received by their patients with cardiovascular disease.
Our study shows that integrated care, as an organizational intervention, allows greater adherence to clinical guidelines for variables that have been widely shown to improve morbidity and mortality,12, 18, 21 and so it is reasonable to think that the integration is beneficial for the patients. However, due to the study design, it was not possible to quantify the direct effect of the intervention on mortality, major events, or admissions. Prospective follow-up would be required to compare PCC that underwent integration with others that use a conventional model.
The study has some other limitations. As this was an observational study, we cannot categorically demonstrate that the results seen were a direct consequence of the new model, although it seems reasonable to assume that the change of model was crucial to the improvements observed. Likewise, we cannot differentiate between which characteristics of the multidisciplinary intervention performed had the greatest influence. The model was applicable in our region and it might be possible to extrapolate to other regions in Spain, but each region has its own organizational characteristics that influence clinical practice and so each integration model should be designed by adapting to those characteristics. Our study focused on the impact on patients in long-term follow-up, and not on patients with acute conditions referred for diagnosis. Satisfaction with primary health care was evaluated by comparison with the model of specialist care, but not by assessing patient satisfaction and quality of life.
CONCLUSIONSAfter applying the integrated care model to cardiology, improved long-term monitoring and treatment of patients with ischemic heart disease, heart failure, and atrial fibrillation were observed for the variables studied. Integration allows a redistribution of the chronic patients between primary care and cardiology, with increased follow-up of the patients with most serious disease by the cardiologist while follow-up of stable patients is performed by the family physicians, with the cardiologist as consultant. The satisfaction of the family physicians increased after integration, particularly in view of the better communication and coordination with the cardiologist. Integration was not accompanied by an increase in resource usage.
CONFLICT OF INTERESTSDr Magda Heras belongs to the HERACLES Network, Spanish Ministry of Science and Innovation, Instituto de Salud Carlos III.
Acknowledgments
We would like to thank the primary care physicians, cardiologists, nursing staff, and administrative staff of the primary care teams of our health district (Centros de Atención Primaria Carles Ribas, La Marina, Sants, Carreras-Candi, Numància, Consell de Cent, Magoria, Montnegre, CAPSE Rosselló y Casanovas, Les Corts, and Les Hortes), whose cooperation was essential to implement the integrated care program.
We also thank Carlos Cervera for his assistance with the statistical analysis.
Received 26 October 2010
Accepted 28 February 2011
Corresponding author: Servicio de Cardiología, Hospital Clínic, Villarroel 170, 08036 Barcelona, Spain. cfalces@clinic.ub.es