INTRODUCTION
Patients who are referred for cardiac surgery are increasingly older and present with a high prevalence of cardiovascular risk factors.1,2 Nevertheless, a number of nonsurgical measures for secondary prevention are reportedly underused, both in cardiovascular surgery departments3,4 and other settings.5-8 For this reason, we
decided to carry out a study to analyze the magnitude of the problem and evaluate the efficacy of an intervention focusing on improving prescription of secondary cardiovascular prevention measures in patients who undergo cardiac surgery.
METHODS
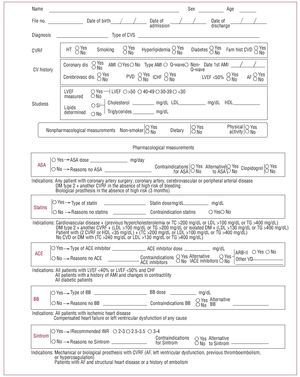
We reviewed the pharmacological measures for secondary cardiovascular prevention recommended in the major clinical practice guidelines.9-14 The conclusions compiled are summarized in Table 1.
An agreement was reached by which no patient would be discharged from the hospital in 2003 without the completion of a form (Figure 1) that included personal details, diagnosis, type of surgery, cardiovascular risk factors, and personal history of each. In addition, any drug treatment prescribed for cardiovascular prevention should be recorded. The document made it necessary to review, on an individual basis, the indication and dosage of each drug or, should it be the case, the reason for which it had not been prescribed. A candidate was defined as that patient in whom a drug was indicated, according to the clinical practice guidelines, and an optimal candidate as a patient with indication and no contraindications. Subsequently, a study was designed to compare the group of patients who were discharged during 2003 with a control group consisting of the patients who were discharged in 2002, for whom the form was completed retrospectively.
Figure 1. ACE indicates angiotensin-converting enzyme; AMI, acute myocardial infarction; ARB, angiotensin receptor blocker (angiotensin II receptor antagonist); ASA, acetylsalicylic acid; AF, atrial fibrillation; AMI, acute myocardial infarction; BB, beta-blocker; CHF, congestive heart failure; CV, cardiovascular; CVD, cardiovascular disease; CVRF, cardiovascular risk factor; CVS, cardiovascular surgery; DM, diabetes mellitus; HDL, high-density lipoprotein; HT, hypertension; INR, international normalized ratio; LDL, low-density lipoprotein; LVEF, left ventricular ejection fraction; PVD, peripheral vascular disease; TC, total cholesterol; TG, triglycerides; VD, vasodilator.
Statistical Analysis
We carried out a descriptive analysis of the characteristics of the patients in each group to assess their homogeneity. The 2 groups were then compared in terms of prescription rates, adjusted to the different prevention measures employed in each. Student t test was used for the comparison of 2 means and ANOVA for the comparison of more than 2 means. The proportions were analyzed by the c2 test.
RESULTS
A total of 710 patients were recruited (369 in 2002 and 341 in 2003). Table 2 shows the clinical characteristics of each group. The rates of utilization of the secondary prevention treatments in the 2 groups (2002/2003) are given below.
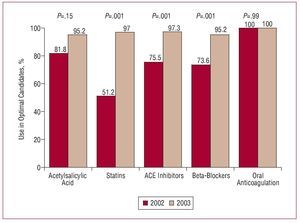
Figure 2 summarizes the percentage of optimal candidates in whom the corresponding secondary prevention measures were applied before and after the intervention.
Figure 2. Percentage of optimal candidates who received the indicated treatment in 2002 and 2003. ACE indicates angiotensin-converting enzyme.
Treatment with acetylsalicylic acid was received by 81.8% of the optimal candidates in 2002 and by 95.2% in 2003 (P=.15).
The number of patients who were optimal candidates for statin therapy was 203 (55%) in 2002 and 228 (66.8%) in 2003. Of these, 104 (51.2%) and 195 (97%), respectively, received treatment with statins (P<.001).
In 2002, 97.8% of the patients were optimal candidates for treatment with angiotensin-converting enzyme (ACE) inhibitors, whereas the percentage for 2003 was 92.3%; of these, 75.5% received ACE inhibitors in 2002 and 97.3% in 2003 (P<.001).
With respect to treatment with beta-blockers, 89% were optimal candidates in 2002 and 89.9% in 2003; of these patients, 73.6% received these drugs in 2002 and 95.2% in 2003 (P<.001).
All the optimal candidates for oral anticoagulation therapy in the 2 groups received this treatment.
DISCUSSION
The present study demonstrates that a simple and inexpensive intervention, such as the agreement of the members of a department to complete a reminder form prior to the discharge of each patient, can improve the use of secondary prevention drug treatments in patients who have undergone cardiac surgery.
A number of secondary cardiovascular prevention measures have been shown to be capable of improving survival and reducing the incidence of new cardiovascular events.9-14 Despite the fact that cardiovascular prevention measures are employed effectively prior to surgery, the incidence of cardiovascular risk factors in patients referred for cardiac surgery remains high. A number of studies have been carried out to verify the degree of compliance with the recommendations of the clinical practice guidelines in cardiac patients. These studies have demonstrated both the underuse of these recommendations and the wide variability in their use, both in Spain5,6 and in other parts of the world.7,8 Although several reports have analyzed the processes related to the improved quality of patient management in the field of cardiology,15-20 there is much less information on the patients who undergo cardiac surgery. We have managed to optimize the prescription of all the pharmacological measures, achieving a rate of compliance on the part of optimal candidates of nearly 95%. Our written form is an inexpensive, simple, highly manageable and reproducible tool that takes very little time to complete. It might be logical to think that, being subjected to a protocol to such a great extent, the tool should have resulted in a utilization rate of 100%; however, it must be taken into account that the introduction of a new tool in a department requires a certain amount of time and training.
One of the limitations of the study is that, since there is no nonintervention control group, the establishment of a cause-effect relationship may be questionable.
We consider that it would not have been ethical to fail to offer a system that was clearly going to improve the quality of care to all patients and, thus, we decided to use a historical control group.
In conclusion, a simple and inexpensive intervention, based on a manageable and reproducible document, is capable of producing a very substantial improvement in the use of secondary prevention methods in patients subjected to cardiac surgery.
Correspondence: Dr. G. Reyes Copa. Hospital Universitario La Princesa.
Diego de León, 62. 28006 Madrid. España.
E-mail: guillermo_reyes_copa@yahoo.es
Received May 28, 2007.
Accepted for publication November 13, 2007.