To the Editor,
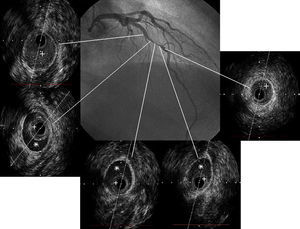
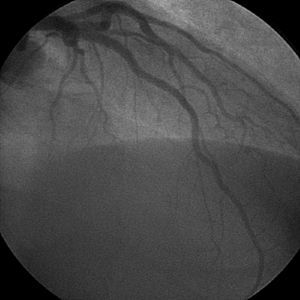
A 49-year-old woman with no cardiovascular risk factors was admitted to our department with high-risk non-ST-elevation acute coronary syndrome. Coronary angiography revealed severe stenosis in a segment located in the middle portion of the anterior descending artery, with no evidence of other lesions (Figure 1). Given the ambiguity of the angiogram and the absence of risk factors, we decided to perform intravascular ultrasound, which revealed localized dissection that had not been visible in the angiogram (Figure 1). There was no apparent intimal rupture but there was evidence of hematoma within the intima. Given the lack of information on the course of the lesion, and since it was located in the anterior descending artery of a young woman, we decided to perform angioplasty with implantation of a drug-eluting stent, with excellent angiographic results (Figure 2).
Figure 1. Lesion in the middle portion of the anterior descending artery in which a hematoma (*) is visible that has caused severe stenosis of the vessel lumen (+).
Figure 2. Final outcome.
Spontaneous coronary artery dissection is a rare cause of acute coronary syndrome (ACS) and sudden death. It has traditionally been described in 3 groups of patients1: patients with coronary artery disease, women during the peripartum period, and a heterogeneous group of patients with idiopathic disease, comprising individuals without cardiovascular risk factors, those with connective tissue disorders (Marfan syndrome, Ehlers–Danlos syndrome, etc.), and cases of intoxication.
There is a clear predominance of women (80% of cases), with a mean age at presentation of 40 years and 25% of cases occurring in the peripartum period. The overall incidence ranges from 0.1% to 1.1%.2 The most commonly affected artery in women is the anterior descending, whereas in men the right coronary artery is more often affected.1,2 Cases of multivessel dissection and of left main coronary artery dissection have also been described.
The pathophysiology involves hemorrhage between the medial layer and the external elastic lamina, leading to separation of the layers, expansion of a false lumen, and compression of the native lumen that results in ischemia.2 Rupture and hemorrhage of the vasa vasorum has been suggested as a potential mechanism.2,3 Eosinophilic infiltrates have also been observed in the dissected region, suggesting a possible inflammatory or vasculitic mechanism,2,3 although some authors maintain that the presence of inflammatory cells is a consequence rather than a cause of the dissection. The association with the peripartum period and the use of oral contraceptives supports the hypothesis that the condition occurs as a result of connective tissue changes induced by hormones (endogenous or exogenous) and the hemodynamic changes characteristic of pregnancy. Numerous cases have also been reported in association with acute changes in intrathoracic pressure.3 Nevertheless, in many patients, no clear trigger is observed and it is likely that there are multiple etiologies.
Diagnosis is based on observation of a radiolucent intimal flap in the coronary angiogram. Diagnosis using angiography alone is often difficult when there is no apparent intimal rupture, with no observable flap and only vessel stenosis visible. Consequently, the use of intravascular ultrasound is important in young patients with no cardiovascular risk factors in whom spontaneous coronary dissection is suspected, since this allows diagnosis and can differentiate between the false and true lumens.
Consensus is lacking on the most appropriate treatment options, which depend on factors such as the number of affected vessels, whether the left main coronary artery is affected, distal coronary flow, and clinical stability. Thus, patients who are clinically unstable or have poor distal flow should be treated by percutaneous transluminal coronary angioplasty (PTCA) in localized dissections, whereas surgical revascularization would be a more appropriate option in patients with multivessel dissections, long lesions, or lesions of the left main coronary artery. In patients who have ACS with localized dissection and who remain asymptomatic, hemodynamically stable, and have good distal coronary flow, conservative treatment can be employed with double antiplatelet therapy and β-blockers, with angiographic follow-up in a few months, since in many cases the dissection is found to completely reseal.2,3 Other authors favor early, aggressive treatment with revascularization, since the natural course of this process is poorly understood.
In the case of PTCA, intravascular ultrasound should be used to ensure that the guidewire is in the native lumen and that stent placement does not cause propagation of the dissection or protrusion of a thrombus at one end.3
Corresponding author. geoffyanes@hotmail.com