To the Editor,
Heyde's Syndrome is described as an association between aortic stenosis and bleeding due to intestinal angiodysplasia.1 This hemorrhagic syndrome has been linked to an acquired deficit of Type IIa von Willebrand factor.
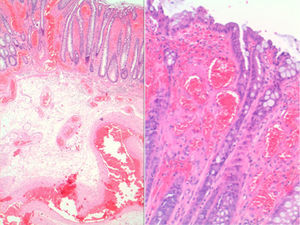
We present the case of an 89-year-old woman with a personal history of hypertension, dyslipidemia and known, but unstudied, systolic murmur. She came to the accident and emergency department due to an episode of syncope and melena. On laboratory analysis hemoglobin values were found to be 6.4g/dL with a hematocrit of 18%. In view of these results, the patient needed a transfusion and was admitted so that the anemia could be studied. An abdominal contrast computed tomography, colonoscopy and oral endoscopy were performed, but the bleeding site was not found. As hemorrhage persisted and repeated transfusions were necessary, emergency surgery was performed. During surgery, intraoperative endoscopy was performed, and the bleeding site was found in the proximal ileum. A corresponding intestinal resection was carried out at that level. A pathology study found the resected tissue to be compatible with intestinal angiodysplasia (Figure 1).
Figure 1. Histological preparation of the colon wall in which thin-walled endothelial-lined vessels with ectasia are seen (H–E, ×10 and ×120).
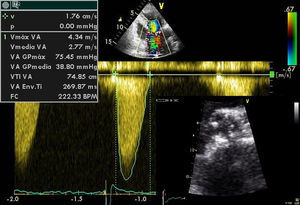
The patient progressed favorably, and on discharge was referred to the Cardiology Department so that her murmur could be studied. An echocardiogram was requested and showed a calcified aortic valve with a maximum gradient of 75mmHg, a mean gradient of 38mmHg and an effective area of 0.7cm2, all of which is compatible with severe aortic stenosis (Figure 2). It also showed a non-dilated left ventricle with slight hypertrophy and preserved systolic function. An enhanced coagulation study was requested, including platelet function and measurement of the function and concentration of von Willebrand complex: factor VIII (PFA-100), which was normal. Elective minimally invasive valve replacement surgery was proposed, which the patient rejected.
Figure 2. Image of aortic short axis transthoracic echocardiogram showing thickening of valve leaflets with restricted opening and with continuous Doppler showing elevated transvalvular gradients.
Angiodysplasia is a degenerative disease of the intestinal mucosa related to the aging process and one of the main causes of gastrointestinal bleeding in the elderly. Its association with aortic stenosis is well known.1,2 Many mechanisms have been considered to explain this syndrome; currently the most prominent is an acquired deficit of Type IIa von Willebrand factor, characterized by a loss of the largest VWF multimers,3 although this causal relationship cannot always be demonstrated, as in this case.
Von Willebrand factor is a high-molecular-weight multimeric protein secreted by endothelial cells that stimulates platelet adhesion and aggregation when there is vascular damage. These multimers are cleared by plasma proteases that are especially active in turbulent blood flow situations.
In aortic stenosis, fragmentation of VWF multimers is increased, which reduces their number and predisposes bleeding.4 Studies have reported that these coagulation anomalies are directly related to the severity of aortic stenosis and are reversible after valve replacement if successful, so that recurrence of bleeding could be an indication of persistent stenosis.5 Therefore, although in some cases of extensive bleeding, such as this one, intestinal resection is necessary, many authors have shown that gastrointestinal bleeding ceases after valve replacement, being even more likely to prevent recurrences than intestinal resection.2
Heyde's Syndrome is an entity to be kept in mind, even more nowadays with an aging population, when assessing patients with a history of bleeding or anemia, especially when the bleeding site is not found on initial examination. Based on these data, we propose the hypothesis that this association could be a new indication for valve replacement; however, gastrointestinal bleeding is not used as an indicator in current clinical practice guides.6
Received 25 March 2010
Corresponding author. Tel.: +34 616285029. aggarciamartin@gmail.com