Keywords
INTRODUCTION
Myxomas are the most frequent benign primary cardiac tumor. In 90% of cases myxomas occur as single tumors, usually in the left atrium (75% of cases), followed by the right atrium (18%) and, less frequently, the ventricles (8%).1 Myxomas of the right atrium can remain undiagnosed for a long time due to the absence or non-specificity of symptoms. These tumors are sometimes diagnosed after an episode of pulmonary embolism with no clear origin or when, due to their large size, they cause obstruction of the tricuspid valve or venous return, originating right cardiac insufficiency.
A case is reported of an asymptomatic young male patient with positive APA in which a right atrial mass suggestive of myxoma was diagnosed after a differential diagnosis with atrial thrombus was made.
CLINICAL CASE
A 28-year-old man with no personal history of interest but with a family history that included the death of a sister at the age of 34 years due to a syndrome of polymyositis overlapping with progressive systemic sclerosis that affected the myocardium. The patient was referred for study after a prolonged partial thromboplastin time (PTTa) was detected in a routine laboratory test.
The patient was asymptomatic and the physical examination was normal. The differential blood count, general biochemistry, electrocardiogram, and chest radiograph showed no abnormalities. The only finding, in the coagulation study, was prolongation of PTTa to 42 seconds (reference 26,5), with a ratio of 1.3. The immunological study disclosed the presence of weakly positive lupus anticoagulant (LA) and high anticardiolipin antibody titers (ACA): IgG ACA, 41 GPL (0-23) and IgM ACA, 15 MPL (0-11). The rest of the immunological study and the thrombophilia study were normal.
Transthoracic echocardiography (TTE) revealed a homogeneous, slightly lobulated 4 cm×3 cm mass inside the right atrium, adhered to the interatrial septum, that protruded slightly during diastole towards the tricuspid valve without obstructing the inferior vena cava (Figure 1). The rest of the examination was normal. The study was completed with transesophageal echocardiography and magnetic resonance imaging (Figure 2), which confirmed the findings of TTE and excluded the presence of other intracavitary masses. Although the first diagnosis considered was atrial myxoma, the differential diagnosis was made with thrombus and the decision was made to initiate oral anticoagulation with acenocoumarol. The follow-up TTE performed after one month of treatment did not reveal any change in the size or morphology of the atrial mass.
Fig. 1. Transthoracic echocardiography. Upper image: longitudinal parasternal right-cavity plane showing the tumor inside the right atrium and its relation with the tricuspid valve. Lower image: apical four-chamber plane in which the tumor adhered to the interatrial septum is apparent. MYX indicates myxoma; RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle; T, tricuspid valve.
Fig. 2. Magnetic resonance image. Left: oblique sagittal plane in which the tumor adhered to the interatrial septum is visible. Right: cross-sectional four-cavity plane showing the tumor inside the right atrium. MYX indicates myxoma; RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle; Ao, aorta; IVC, inferior vena cava.
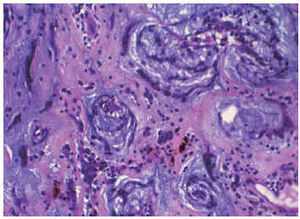
The patient underwent surgery with extracorporeal circulation and cannulation of both cavas. Access to the tumor mass was obtained by right atriotomy. The tumor had a broad base of insertion on the interatrial septum so the septum had to be repaired with a pericardial patch after tumor resection. Histopathological study of the tumor mass confirmed the diagnosis of myxoma (Figure 3). After 4 months of follow-up the patient is asymptomatic, PTTa is normal, and APA is negative.
Fig. 3. Histopathological image showing a typical cluster of myxomatous cells of spindle-shaped appearance arrayed around vascular channels, interspersed with abundant extracellular myxoid matrix.
DISCUSSION
Right atrial myxoma is a frequent tumor that is difficult to diagnose in early stages due to the absence of symptoms or the non-specificity of the cardiological and systemic manifestations that it causes. Constitutional symptoms and hematological abnormalities are present in up to 90% of patients with myxoma and include, among other symptoms, weight loss, fever, anemia, increased erythrocyte sedimentation rate, and hypergammaglobulinemia, which can simulate connective tissue disease.1,2
In this case the tumor was discovered by TTE performed in the course of the systematic study of a patient with positive APA. APA are a heterogeneous group of immunoglobulins against negatively charged phospholipids of the cell membranes. The APA include LA and ACA. These antibodies have been described in diverse situations, such as systemic autoimmune diseases, fundamentally systemic lupus erythematosus, after infectious processes or exposure to drugs, in association with neoplasms, as well as in healthy patients.3 Some cardiac tumors, like papillary fibroelastoma and myxoma, have also been associated with the presence of APA in serum.4-6
Patients with cardiac myxomas present high serum concentrations of IL-6 that normalize after the tumor is removed.7,8 IL-6 is a cytokine that stimulates the synthesis of acute-phase reagents and promotes the differentiation of B lymphocytes, which induce the synthesis of immunoglobulins and autoantibodies, including APA. In the case reported here, the normalization of coagulation abnormalities and negativization of antibody titers after the tumor was removed seem to indicate that the myxoma originated the immunological reaction observed in the patient by means of IL-6 production.
The presence of these autoantibodies has been related to the appearance of recurrent venous or arterial thrombosis, repeated miscarriages and/or thrombocytopenia, constituting the so-called antiphospholipid syndrome (APS). This syndrome can appear in primary form in patients without clinical or serological evidence of another disease or secondary to one of the diseases mentioned. The most frequent cardiological manifestations of APS include myocardial infarction due to coronary artery thrombosis and valve lesions.9,10 Intracavitary thrombosis, although much rarer, is another cardiac manifestation associated with APS. In the literature reviewed, a total of 9 patients diagnosed as APS were found to have intracardiac thrombi, which generally simulated a myxoma, and the definitive diagnosis could only be established by histopathological study.11-17 In all the cases reviewed, the thrombi described were found in the right cavities (8 in the right atrium and 1 in the right ventricle). The majority (7) were single thrombi.
Although the presence of APA does not necessarily imply the appearance of clinical manifestations of APS, the risk of suffering a thrombosis seems to be greater in patients in which high ACA titers are detected, with IgG values >40 GPL in patients with previous thrombosis, as shown by the results of two prospective studies in recent years.18,19 In our patient, the morphological characteristics of the atrial mass suggested myxoma, but the presence of high ACA IgG levels suggested the possibility of a primary APS whose only manifestation was an intracardiac thrombus.
The interest of the present case derives from the fact that the myxoma was diagnosed after performing routine TTE as part of the systematic work-up of an apparently healthy patient with persistently positive APA determinations. The fact that the immunological abnormalities normalized after excision of the tumor seems to indicate that the myxoma was its cause, although this association could have been merely accidental. On the other hand, the presence of an intracardiac mass in a patient with APA makes the differential diagnosis between intracavitary thrombosis and myxoma difficult. In such patients, treatment with oral anticoagulants seems reasonable until a definitive diagnosis can be reached, which can only be established after surgical excision and an anatomopathological study of the tumor mass.
ACKNOWLEDGMENTS
To Sonia Alonso, resident physician of the Pathology Department of the Hospital General Universitario, for her assistance in developing this communication.
Correspondence: Dra. E. Esteban Esteban.
Servicio de Cardiología. Hospital Arnau de Vilanova.
C/ S. Clemente, 12. 46015 Valencia. España.
E-mail: ma.estebane@comv.es