To analyze the association between higher body mass index and waist circumference, and the prognostic values of both indicators in total and cardiac mortality in patients with chronic heart failure.
MethodsThe study included 2254 patients who were followed up for 4 years. Obesity was classified as a body mass index ≥30 and overweight as a body mass index of 25.0-29.9. Central obesity was defined as waist circumference ≥88 cm for women and ≥102cm for men. Independent predictors of total and cardiac mortality were assessed in a multivariate Cox model adjusted for confounding variables.
ResultsObesity was present in 35% of patients, overweight in 43%, and central obesity in 60%. Body mass index and waist circumference were independent predictors of lower total mortality: hazard ratio=0.84 (P<.001) and hazard ratio=0.97 (P=.01), respectively, and lower cardiac death (body mass index, hazard ratio=0.84, P<.001; waist circumference, hazard ratio=0.97, P=.01). The interaction between body mass index and waist circumference (hazard ratio=1.001, P<.01) showed that the protective effect of body mass index was lost in patients with a waist circumference >120cm.
ConclusionsMortality was significantly lower in patients with a high body mass index and waist circumference. The results also showed that this protection was lost when these indicators over a certain limit.
Keywords
Obesity is an important public health issue that is reaching epidemic proportions in developed and developing countries. According to the World Health Organization, more than 1400 million adults were overweight in 2008; within this group, obesity affected more than 200 million men and nearly 300 million women.1 Obesity itself is considered a chronic disease but it is also an important risk factor for cardiovascular disease. Numerous studies have shown that central obesity—measured by waist circumference (WC)—is associated with greater risk of cardiovascular disease.2–4
The role of obesity in mortality from heart failure (HF) has become controversial with the description of the so-called obesity paradox, which suggests that overweight or obese patients have a better prognosis, despite higher cardiovascular risk. In contrast, cardiac cachexia is associated with higher mortality. Although the mechanisms by which the prognosis of obese patients improves remain unknown, some studies indicate that improvement may be related to the ratio of lean mass to adipose mass, or that measuring nutritional parameters could be more important in determining the relationship between obesity and a lower risk of death.5,6 Central obesity also seems to have a predictive effect in patients with HF,7 although studies of the issue are scarce. In addition, it is unknown whether the protective effect is lost above a certain degree of central obesity.
The main aim of this study was to analyze the association between a higher body mass index (BMI) and WC, and the prognostic value of both indicators for total and cardiac mortality in patients with chronic HF hospitalized in cardiology units in Spanish hospitals.
METHODSWe enrolled patients on the REDINSCOR (Spanish Heart Failure Network, Red Española de Insuficiencia Cardiaca) registry, a prospective observational study conducted in the HF units of 18 Spanish hospitals. The protocol was approved by the research committees of participating institutions and all patients gave written informed consent.
Patients were included in the study between 2007 and 2011 assuming they met the following criteria: age ≥18 years, symptomatic HF (New York Heart Association functional class II-IV), >24h prior hospitalization for HF in the previous year, being under optimized treatment regimens in line with established clinical practice guidelines,8 and having any of the following echocardiographic abnormalities: ≤40% left ventricular ejection fraction, ≥60mm end-of-diastole diameter, abnormal ventricular relaxation typical of diastolic dysfunction, and ≥14mm interventricular septum and/or posterior wall thickness. We excluded patients with reversible new-onset acute HF and severe valvular disease susceptible to surgical repair, right HF secondary to chronic cor pulmonale or congenital heart disease and/or a concomitant terminal disease.
ProcedureThe data collection questionnaires were specially designed for the study and data was gathered when registering patients on a web site.9 We performed monthly quality control checks during follow-up and data inclusion.
Information on the main risk factors was recorded at the start of the study, during the first outpatient visit following hospitalization. The independent variables recorded were age, sex, high blood pressure (defined as systolic blood pressure ≥140mmHg/diastolic blood pressure ≥90mmHg with or without drug treatment), weight, height, BMI (normal, <25; overweight, 25.0-29.9; obese, ≥30), central obesity (WC ≥88cm in women and ≥102cm in men), diabetes mellitus (defined as a history of criteria of diabetes mellitus or the need for medication), dyslipidemia (history of criteria of dyslipidemia or the need for medication), smoking (“smoker”, 1 or more cigarettes per day; “ex-smoker”, no cigarettes in the last 6 months), history of alcoholism (yes/no), anemia (hemoglobin <120g/L in women and <130g/L in men) and prescription of medication.
Information on the dependent variable of mortality was obtained from medical records and family members. We collected data on total and cardiac mortality. Cardiac mortality included mortality from sudden death, refractory HF, and myocardial infarction. Patients who underwent urgent heart transplantation were classified as death from refractory HF. In all patients, the researcher had to provide details about the death episode. All deaths were reviewed by a mortality committee to validate the cause. Patients lost during follow-up and those undergoing elective heart transplantation were censored.
Statistical AnalysisContinuous variables are expressed as mean (standard deviation) or median [interquartile range], as appropriate. Categorical variables are presented as percentages. We conducted a descriptive analysis, chi-squared and McNemar's tests for categorical variables. To compare continuous variables, we used analysis of variance (ANOVA) and Student's t test for independent related samples.
Multivariate analysis was conducted using Cox proportional hazard modelling. The variables that were significant in the univariate model (P<.1) were included in the multivariate model and the backward stepwise method was used to identify independent risk factors. We also studied the interaction between BMI and WC. We determined the adjustment of the model with clinically relevant variables. The proportionality assumption of the Cox model hazard ratio (HR) was determined using Schoenfeld residuals. The discrimination of the model was calculated with Harrell's C-index, and calibration of the model was calculated with the Gronnesby and Borgan test. Simple imputations with multivariate regressions were used for all variables with <5% missingness (except brain natriuretic peptide [BNP] and N-terminal probrain natriuretic peptide [NT-proBNP], which did not meet this criterion).10–13 A value of P<.05 was considered statistically significant. The analysis was performed with SPSS 19 and Stata 12 software.
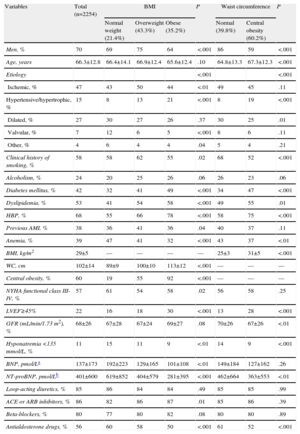
RESULTSWe included 2254 patients, of which 70% were men. The mean age was 66 (13) years. Some 43% were overweight, 35% were obese, according to their BMI, and 60% had central obesity with a mean WC of 103 (13) cm in men and 101 (15) cm in women. However, we also identified 15 patients (0.7%) with a low BMI (<18.5) who were not analyzed separately as they were too few in number. Table 1 compares baseline clinical characteristics according to BMI and WC. In the group of obese patients, we found a higher percentage of women and a greater incidence of a hypertensive or hypertrophic etiology, diabetes mellitus, dyslipidemia, and high blood pressure. In the normal weight group, we found more anemia, worse New York Heart Association functional class, more depressed left ventricular ejection fraction, more hyponatremia and higher BNP values. A higher WC was significantly associated with the same parameters as obesity and overweight. In this cohort, BMI correlated significantly with WC, with Pearson's r=0.77 (95% confidence interval [95%CI], 0.75-0.78; P<.001).
Baseline Characteristics of Patients According to Body Mass Index and Central Obesity
| Variables | Total (n=2254) | BMI | P | Waist circumference | P | |||
| Normal weight (21.4%) | Overweight (43.3%) | Obese (35.2%) | Normal (39.8%) | Central obesity (60.2%) | ||||
| Men, % | 70 | 69 | 75 | 64 | <.001 | 86 | 59 | <.001 |
| Age, years | 66.3±12.8 | 66.4±14.1 | 66.9±12.4 | 65.6±12.4 | .10 | 64.8±13.3 | 67.3±12.3 | <.001 |
| Etiology | <.001 | <.001 | ||||||
| Ischemic, % | 47 | 43 | 50 | 44 | <.01 | 49 | 45 | .11 |
| Hypertensive/hypertrophic, % | 15 | 8 | 13 | 21 | <.001 | 8 | 19 | <.001 |
| Dilated, % | 27 | 30 | 27 | 26 | .37 | 30 | 25 | .01 |
| Valvular, % | 7 | 12 | 6 | 5 | <.001 | 8 | 6 | .11 |
| Other, % | 4 | 6 | 4 | 4 | .04 | 5 | 4 | .21 |
| Clinical history of smoking, % | 58 | 58 | 62 | 55 | .02 | 68 | 52 | <.001 |
| Alcoholism, % | 24 | 20 | 25 | 26 | .06 | 26 | 23 | .06 |
| Diabetes mellitus, % | 42 | 32 | 41 | 49 | <.001 | 34 | 47 | <.001 |
| Dyslipidemia, % | 53 | 41 | 54 | 58 | <.001 | 49 | 55 | .01 |
| HBP, % | 68 | 55 | 66 | 78 | <.001 | 58 | 75 | <.001 |
| Previous AMI, % | 38 | 36 | 41 | 36 | .04 | 40 | 37 | .11 |
| Anemia, % | 39 | 47 | 41 | 32 | <.001 | 43 | 37 | <.01 |
| BMI, kg/m2 | 29±5 | — | — | — | — | 25±3 | 31±5 | <.001 |
| WC, cm | 102±14 | 89±9 | 100±10 | 113±12 | <.001 | — | — | — |
| Central obesity, % | 60 | 19 | 55 | 92 | <.001 | — | — | — |
| NYHA functional class III-IV, % | 57 | 61 | 54 | 58 | .02 | 56 | 58 | .25 |
| LVEF≥45% | 22 | 16 | 18 | 30 | <.001 | 13 | 28 | <.001 |
| GFR (mL/min/1.73 m2), % | 68±26 | 67±28 | 67±24 | 69±27 | .08 | 70±26 | 67±26 | <.01 |
| Hyponatremia <135 mmol/L, % | 11 | 15 | 11 | 9 | <.01 | 14 | 9 | <.001 |
| BNP, pmol/La | 137±173 | 192±223 | 129±165 | 101±108 | <.01 | 149±184 | 127±162 | .26 |
| NT-proBNP, pmol/Lb | 401±600 | 619±852 | 404±579 | 281±395 | <.001 | 462±664 | 363±553 | <.01 |
| Loop-acting diuretics, % | 85 | 86 | 84 | 84 | .49 | 85 | 85 | .99 |
| ACE or ARB inhibitors, % | 86 | 82 | 86 | 87 | .01 | 85 | 86 | .39 |
| Beta-blockers, % | 80 | 77 | 80 | 82 | .08 | 80 | 80 | .89 |
| Antialdosterone drugs, % | 56 | 60 | 58 | 50 | <.001 | 61 | 52 | <.001 |
ACE inhibitors, angiotensin converting enzyme inhibitors; AMI, acute myocardial infarction; ARB, angiotensin II receptor antagonists; BMI, body mass index; BNP, brain natriuretic peptide; GFR, glomerular filtration rate (MDRD-4 method); HBP, high blood pressure; LVEF, left ventricular ejection fraction; NT–proBNP, N-terminal pro-brain natriuretic peptide; NYHA, New York Heart Association; WC, waist circumference.
Patients were followed-up for a maximum 48 months (median, 21 months).
During follow-up, 475 deaths occurred, of which 341 (72%) were from cardiac causes. Total and cardiac mortality at 4 years were 21% and 15%, respectively. Total mortality was lower in patients with a higher BMI: 21.3% in the overweight and 16.4% in the obese groups compared with 28.4% in patients with normal weight (P<.001). The same trend was found for WC: 18.9% in the central obesity group vs 24.3% in patients with normal WC (P<.01). We found a similar trend for cardiac death; mortality was lower in patients with higher BMI: 15.4% in the overweight and 12.3% in the obese groups vs 19.3% in patients with normal weight (P<.01). Concerning WC, we also found lower mortality in obese patients: 13.9% in the central obesity group vs 17.1% in the normal WC group (P=.04).
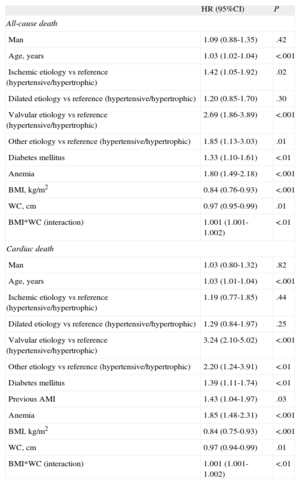
Multivariate AnalysisPredictors of total mortality were identified using multivariate Cox proportional hazard modeling adjusted for confounding variables (Table 2), in which both higher BMI and WC were identified as factors associated with lower mortality (respectively, HR=0.84; 95%CI, 0.76-0.93; P<.001; HR=0.97; 95%CI, 0.95-0.99; P=.01] with interaction between both (HR=1.001; 95%CI, 1.001-1.002; P<.01). In this interaction, a higher WC attenuated the protective effect of a higher BMI. More detailed analysis of interaction found that in patients with a BMI≥35, a higher WC was associated with worse survival; in fact, when WC was >120cm, we found that higher BMI ceased to have any significant protective effect. Other factors associated with greater total mortality were ischemic and valvular etiology, age, anemia and diabetes mellitus. All models were adjusted for relevant clinical variables such as sex, New York Heart Association functional class, left ventricular ejection fraction, hyponatremia, and glomerular filtration rate, but we found no significant changes in the HR of BMI and WC (change <3%)14; therefore, we opted for the reduced model. The multivariate model obtained a Harrell's C-index of 0.8. The Gronnesby and Borgan test of validity of adjustment showed good calibration of the model (P=.26).
Cox Proportional Hazard Modelling
| HR (95%CI) | P | |
| All-cause death | ||
| Man | 1.09 (0.88-1.35) | .42 |
| Age, years | 1.03 (1.02-1.04) | <.001 |
| Ischemic etiology vs reference (hypertensive/hypertrophic) | 1.42 (1.05-1.92) | .02 |
| Dilated etiology vs reference (hypertensive/hypertrophic) | 1.20 (0.85-1.70) | .30 |
| Valvular etiology vs reference (hypertensive/hypertrophic) | 2.69 (1.86-3.89) | <.001 |
| Other etiology vs reference (hypertensive/hypertrophic) | 1.85 (1.13-3.03) | .01 |
| Diabetes mellitus | 1.33 (1.10-1.61) | <.01 |
| Anemia | 1.80 (1.49-2.18) | <.001 |
| BMI, kg/m2 | 0.84 (0.76-0.93) | <.001 |
| WC, cm | 0.97 (0.95-0.99) | .01 |
| BMI*WC (interaction) | 1.001 (1.001-1.002) | <.01 |
| Cardiac death | ||
| Man | 1.03 (0.80-1.32) | .82 |
| Age, years | 1.03 (1.01-1.04) | <.001 |
| Ischemic etiology vs reference (hypertensive/hypertrophic) | 1.19 (0.77-1.85) | .44 |
| Dilated etiology vs reference (hypertensive/hypertrophic) | 1.29 (0.84-1.97) | .25 |
| Valvular etiology vs reference (hypertensive/hypertrophic) | 3.24 (2.10-5.02) | <.001 |
| Other etiology vs reference (hypertensive/hypertrophic) | 2.20 (1.24-3.91) | <.01 |
| Diabetes mellitus | 1.39 (1.11-1.74) | <.01 |
| Previous AMI | 1.43 (1.04-1.97) | .03 |
| Anemia | 1.85 (1.48-2.31) | <.001 |
| BMI, kg/m2 | 0.84 (0.75-0.93) | <.001 |
| WC, cm | 0.97 (0.94-0.99) | .01 |
| BMI*WC (interaction) | 1.001 (1.001-1.002) | <.01 |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; BMI, body mass index; HR, hazard ratio; WC, waist circumference.
Similarly, for cardiac mortality (Table 2), we also found that both BMI and WC were protective factors (HR=0.84; 95%CI 0.75-0.93; P<.001; and HR=0.97; 95%CI, 0.94-0.99; P=.01), with interaction between them (HR=1.001; 95%CI, 1.001-1.002; P<.01). In their interaction, we again found that a higher WC attenuated the size of the protective effect of BMI. Other associated risk factors were valvular etiology, age, a history of acute myocardial infarction, anemia, and diabetes mellitus. Similarly, all models were adjusted for the variable sex. The final model was adjusted for clinically relevant variables but we found no significant changes in the HR of BMI and WC (change <5%)14 and opted for the reduced model, as in the case of total mortality. The multivariate model obtained a Harrell's C-index of 0.69. The Gronnesby and Borgan test of validity of adjustment showed good calibration of the model (P=.36).
DISCUSSIONMost Relevant FindingsThe results of this study confirm the “obesity paradox”15 in patients hospitalized for HF in the REDINSCOR registry for both BMI and WC. Hence, patients with greater BMI and WC have lower total and cardiac mortality. However, in obese patients with a BMI close to 35, the protective effect of central obesity disappears. These results support the recommendation to measure WC as well as calculating BMI to best determine the risk of total and cardiac mortality in HF.
Obesity ParadoxIn recent years, several studies have shown an association between a higher BMI and lower mortality in patients with chronic disease such as chronic kidney failure, rheumatoid arthritis, cancer and, especially, coronary heart disease.16–21 A meta-analysis22 including 40 studies with a total 250 152 patients with ischemic heart disease demonstrated that BMI as an indicator of overweight and obesity was associated with a 16% and 12% lower risk of mortality, respectively. Although several studies point to the obesity paradox,23 much controversy remains about the prognostic value of overweight and obesity and few studies have analyzed the role of central obesity.24 Zamora et al.18 studied 501 patients with HF and 30% median ejection fraction and identified a higher BMI as an independent predictor of lower total mortality at 2 years. Nevertheless, in a subsequent study, the beneficial effect of higher weight was only demonstrated in patients without ischemic heart disease.25 The DIAMOND-CHF registry,26 including 4700 patients with HF and in New York Heart Association functional class III-IV, found improved prognosis associated with greater BMI only in patients with better ventricular function, whereas prognosis worsened in patients with systolic dysfunction. In Spain, a recent study27 using Minimum Basic Data Set data on patients hospitalized for HF found that a diagnosis of obesity reduced mortality and readmissions. Our results confirm earlier findings reported by Zapatero et al.27 and, moreover, confirm the role of WC as a significant independent predictor of lower mortality, but with an attenuating effect in inverse relation between BMI and mortality. Notably, in contrast to Zapatero et al.,27 we included patients prospectively, with direct data collection and >4 years’ follow-up.
Several studies have analyzed possible causal mechanisms underlying the obesity paradox but it seems more than likely that multiple factors are involved. Hence, in obese individuals with HF, symptoms can appear earlier, and therefore diagnosis and treatment occur at earlier stages of the disease. The paradox could also be explained by the greater metabolic reserve in obese individuals, making them more resistant to the increase in catabolism found in of patients with HF. Similarly, obese patients have higher tumor necrosis factor-α (TNFα) receptor values than patients with HF, which could attenuate the negative impact of high TNFα concentrations. Obese patients also have an increase in plasma lipoproteins, which could counter high lipopolysaccharide values, which are a powerful stimulus to the release of inflammatory cytokines.28–33 Finally, cardiac cachexia has been associated with higher mortality, and therefore its absence would improve prognosis, and obesity could be a marker of better prognosis.
Prognostic Value of Waist Circumference MeasurementCurrently BMI (weight in kilos divided by height in meters squared) is generally used as a marker of general adiposity; however, several authors have questioned its suitability since BMI does not distinguish between adipose mass and muscle mass, which could lead to incorrect assumptions about the association between obesity and mortality in HF patients. Therefore, it is becoming increasingly clear that measuring total body fat and using markers of central fat such as WC could be better than using BMI alone.15,34 Hence, we measured both BMI and WC in patients with chronic HF.
A higher WC is the most specific marker of central obesity. Together with diabetes mellitus and high blood pressure, it constitutes metabolic syndrome, which is associated with greater cardiovascular risk. The prognostic value of a higher WC in HF has been studied little. In 344 patients with HF and systolic dysfunction, Clark et al.35 analyzed the prognostic value of BMI and WC and found lower total mortality in the group of patients with higher values of both parameters. The beneficial effect was similar in both sexes. However, these studies examined the effect of higher BMI and WC in patients with depressed ejection fraction and advanced HF. Our study included patients diagnosed with HF, without excluding either patients with preserved ejection fraction or others on the basis of HF etiology, thus providing information about the wider population with HF. In fact, in population-wide registries, around 50% of patients requiring hospitalization for HF have preserved ejection fraction. Our study confirmed that a higher BMI and WC were associated with better prognosis. Hence, the relationship between BMI and mortality tended to show a U-shaped curve, which is a type of relationship that usually also occurs in acute and chronic ischemic heart disease.36 For WC, we found a stronger relationship with mortality in J, which demonstrates the added value of measuring WC. Thus, with BMI values ≥35, a higher WC becomes a risk factor, whereas when WC is around 120cm, BMI loses its protective effect.
Total mortality in our study was 21% at 4 years, similar to that of other epidemiologic studies or registries of patients with HF, in which total mortality ranges between 20% and 25%.37,38 Unlike previous studies, in our study the beneficial effect of higher BMI and WC was observed in both total and cardiac mortality. However, as in previous studies, our obese patients were younger, more frequently women, with diabetes, high blood pressure, dyslipidemia and anemia, a lower incidence of smoking, and a higher incidence of ≥45% ejection fraction; the main etiology was hypertension, which was associated with low BNP values. Therefore, in principle, our patients had clinical characteristics associated with greater cardiovascular risk; however, a higher percentage of patients with preserved ejection fraction could be important as it contributes to better prognosis. Similarly, we found significantly lower concentrations of natriuretic peptides in patients with both higher BMI and WC. The reduction in BNP concentrations with increasing weight has been described elsewhere and may be associated with greater sodium and fluid retention, which can increase dyspnea and, therefore, be associated with earlier manifestations of disease even in patients with less severe HF.28,39
Limitations and Strengths of the StudyThe study was conducted in a national registry database of patients with HF, which could be considered a limitation. However, this registry was expressly designed to gather data on HF-related factors and exhaustive fulfillment of quality standards and validation of all data introduced by the participating centers was guaranteed. Moreover, data collection was prospective, which considerably improves data quality. A long follow-up period was analyzed, ensuring exhaustive analysis of total and cardiac mortality.
CONCLUSIONSThis study confirms low mortality in patients with chronic HF with greater BMI and WC, corroborating the validity of the obesity paradox in the patients studied. In view of the results, WC should be measured together with BMI to better predict the prognosis of chronic HF.
FUNDINGThe present study has been financed through a grant from the Spanish Ministry of Science and Innovation, (Redes de Investigación del Instituto de Salud Carlos III, REDINSCOR, RD06/0003) and by the European Regional Development Fund (ERDF).
CONFLICTS OF INTERESTNone declared.
The list of researchers collaborating in the REDINSCOR registry can be consulted in the supplementary material to this article.