Keywords
INTRODUCTION
The prevalence of atrial fibrillation (AF) is increasing inexorably in recent years, owing to the aging population, the longer survival of patients with heart disease and, of course, the increased frequency with which it is diagnosed, among other factors, and it has become an important public health problem, especially because of the associated risk of stroke and mortality.1
The annual risk of stroke in patients with AF depends on the number of associated risk factors. Two of these major factors are age and hypertension (HT),2 and, thus, it is essential to identify the patients in whom these 2 conditions coincide in order to adopt the proper preventive measures and diminish the cardioembolic events, occasionally asymptomatic, which can contribute to vascular dementia and to the deterioration of cognitive function in these patients.3
Despite the fact that a number of studies have demonstrated that oral anticoagulation reduces the risk of stroke by 66%, in routine practice, this treatment can be seen to be underutilized, especially in women and older patients, owing to the risk of bleeding and the need for periodic monitoring, among other factors.4,5
In Spain, there have been no recent studies analyzing the management of cardioembolic aspects in order to prevent this arrhythmia in the patient who is both hypertensive and elderly, two of the most prevalent conditions associated with AF and a higher risk of cardioembolism. The objective of this study was to determine the prevalence of AF in hypertensive patients 65 years and older receiving medical care in outpatient clinics and to analyze the use of antithrombotic drugs in this population.
METHODS
The FAPRES registry resulted from a cross-sectional, observational, multicenter epidemiological study, carried out in the health care setting, designed to determine the prevalence of AF in patients aged 65 years and over with a clinical diagnosis of HT in the Valencian Community in eastern Spain. The study took place between June and December, 2008. It involved the participation of 69 researchers from primary care and in-hospital HT units in the Spanish provinces of Alicante, Castellón, and Valencia, in a proportion in accordance with the population of each.
Study Population
For the 5 weeks' duration of the recruitment period, each researcher included consecutively the first 3 patients who came to his or her office on the first day of the workweek, provided they met all the inclusion criteria and none of the exclusion criteria.
The inclusion criteria were: a) age ≥65 years; b) a previous diagnosis of HT at least 3 months prior to the start of the study (office arterial blood pressure ≥140/90 mmHg on several occasions or with previous antihypertensive therapy); and c) consent to participate in the study. The exclusion criteria were age <65 years, arm circumference >42 cm, refusal to consent to participate in the study or conditions that made the patient unfit to take part in the study (for example, evident failure to cooperate, dementia, etc).
Written informed consent was collected from all the patients and the study was carried out in compliance with the principles of the Declaration of Helsinki (Edinburgh amendment, 2000), after having been approved by the hospital ethics committee (Clinical Research Ethics Committee, Hospital General Universitario de Castellón).
Clinical Evaluation
The risk factors and the cardiovascular history of the patients were gathered using a standardized questionnaire. We recorded the age in years, sex, anthropometric data, time elapsed since onset of HT, history of early cardiovascular disease in the immediate family (<65 years of age in women, <55 years of age in men) and personal history of high alcohol consumption, sedentary lifestyle, smoking, diabetes mellitus, dyslipidemia, structural heart disease (coronary artery disease or heart failure), previous stroke, peripheral artery disease, and renal disease.6 The background data also included any previously documented episodes of AF in order to identify cases of paroxysmal or persistent AF that had reverted to sinus rhythm.
Any patient with a history of diabetes mellitus or who was receiving treatment for that disease at the time was considered to be diabetic. Those patients with a history of elevated low-density lipoprotein cholesterol (LDL-C) (>160 mg/dL) or who were receiving treatment involving their diet or lipid-lowering drugs were considered to have hypercholesterolemia.7 Patients who reported having consumed at least 1 cigarette a day for the preceding month were considered to be smokers.8 In contrast, any patient who had stopped smoking at least one year earlier was considered to be an ex-smoker. Those who reported that they walked actively for at least 30 minutes a day or participated in some type of sport 3 days a week were considered nonsedentary,9 and patients who admitted to drinking 4 beers, 4 glasses of wine, 2 whiskies or similar beverages, or more, daily were considered to be drinkers.10 Renal disease was considered to be present in those patients with a history of microalbuminuria (20-299 mg/24 h), proteinuria (300 mg/24 h or higher) or elevated serum creatinine (>1.2 mg/dL in women and >1.3 mg/dL in men).11
The drug therapy being received by each patient at the time of the visit, specifically antihypertensive agents and treatments to prevent cardioembolic events (anticoagulants and platelet antiaggregants), was recorded. A physical examination was also carried out to collect anthropometric data (weight, height and abdominal circumference); in addition, arterial blood pressure was taken on 2 consecutive occasions, and the mean of the 2 measurements was employed as the reference value. The analytical data were gathered from the medical record, if it was dated within the preceding 6 months, or were requested of the laboratory at the time of recruitment. The glomerular filtration rate was determined using the formula of the Modification of Diet in Renal Disease (MDRD) study. The questionnaire with the medical record was sent via CRD (the same platform utilized in the Cardiorisc project, available from: www. cardiorisc.com) to a data processing center.
All of the patients also underwent an electrocardiogram (ECG) that was sent by ordinary mail to a referral center, where two expert cardiologists who did not have access to the clinical data corresponding to the patients independently analyzed the cardiac rhythm. When there was a discrepancy between the 2, a third specialist was consulted. Other parameters analyzed in the ECG were the heart rate, the presence of left ventricular hypertrophy (LVH) (applying the Sokolov criteria, the Cornell criteria or ventricular overload), interventricular conduction disturbances and Q waves indicative of myocardial necrosis. A randomized external audit of 10% of the questionnaires received was carried out to verify the reliability of the data provided.
The group of patients with AF included all those in whom the ECG demonstrated the presence of said arrhythmia (regardless of whether or not it had been diagnosed previously) or who had a documented history of AF, even if they were in sinus rhythm at the time of the test and, thus, probably had paroxysmal or cardioverted AF. In the case of atrial flutter, the patient was included in the AF group, given that the antithrombotic recommendations are similar. Likewise, for the purpose of analyzing the antithrombotic therapy (anticoagulation or antiaggregant therapy) according to the type of AF, the patients with this arrhythmia were divided into 3 groups: a) patients with a history of AF in whom the arrhythmia was detected in the ECG (known permanent AF); b) patients with a history of AF and in sinus rhythm at the time of the test (previous episode of AF); and c) patients with no history of AF and with AF at the time of the ECG (previously undiagnosed AF). Finally, the patients' CHADS2 scores (congestive heart failure, hypertension, age >75 years, diabetes mellitus, and prior stroke or transient ischemic attack) of the patients with AF were determined to assess the risk of stroke and the correct indication for anticoagulation therapy (CHADS2 score >1).12 The contraindications for anticoagulation were also recorded in the study.
Statistical Analysis
All the data collected in the study are expressed in terms of central tendency, measures of dispersion and relative frequencies. The results in the three groups of patients analyzed were compared. Student t test was utilized for the comparison of the quantitative variables between the 2 major groups of individuals (those having and those not having AF); the categorical variables were compared using the c2 test, and we calculated the measures of effect (odds ratio [OR] for the categorical variables and the differences between means for the quantitative variables). In the comparative analysis of antithrombotic therapy according to the type of AF in the three groups, analysis of variance (ANOVA) was employed. To determine the variables independently related to the presence of AF (in the ECG or in a previous episode), we performed multivariate logistic regression analysis, including all the variables that proved to be significant in the univariate analysis and those with known clinical relevance. A P value of less than .05 was considered to indicate statistical significance. The analysis was carried out with the SPSS statistical software package (version 15).
RESULTS
The study included a total of 1028 hypertensive patients, with a mean age of 72.8 years, 52.7% of whom were women. In all, 82.5% of the patients were recruited from primary care offices (848 cases) and the remainder from hospital HT units.
The analysis of the ECG revealed that 6.7% of the patients had AF (67 cases of AF and two of atrial flutter), and that the arrhythmia had not been previously diagnosed in 17 cases (1.7%). A linear increase was observed in the prevalence of AF in the ECG in relation to age, going from 3.2% in patients between the ages of 65 and 69 years to 11.9% in those over the age of 80 years. In addition, 37 patients in sinus rhythm had a history of AF (3.6%), which could correspond to paroxysmal or permanent forms reverted to sinus rhythm; thus, the total prevalence of AF in our series was 10.3%. The prevalence was significantly higher among the patients recruited from the HT units than among those from primary care (23.9% vs 7.4%; P<.001).
The mean age of the patients with AF (a previous episode or ongoing AF) was older and these individuals also were more likely to have a history of associated heart disease (ischemic heart disease or heart failure) and a longer history of HT (Table 1). Left ventricular hypertrophy and changes in the QRS complex were more common in this population. In contrast, the glomerular filtration rate was lower in the patients with AF (Table 2). When we analyzed the group of patients in whom AF had not previously been diagnosed (17 cases), we observed that they were significantly younger than the patients with known ECG evidence of AF (72.5 [3.6] years vs 76.7 [6.3] years; P<.05), exercised more and were less likely to have a history of heart failure; in contrast, there were no differences with respect to the ventricular response in the ECG. This lesser clinical impact could probably justify in part the failure to detect the arrhythmia.
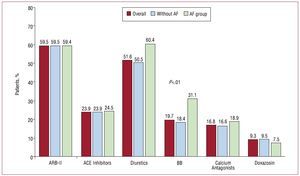
A large number of the patients received drugs to block the renin-angiotensin axis to control their HT. The figure shows the antihypertensive drugs employed in our population. No differences were observed between the subgroups analyzed, with the exception of the significantly greater use of beta blockers among the patients with AF (31.1% vs 18.4%; P<.01).
Figure 1. Antihypertensive treatments utilized in the population. Comparison according to subgroups. ACE indicates angiotensin converting enzyme; AF, atrial fibrillation; ARB, angiotensin receptor blockers (angiotensin II receptor antagonists); BB, beta-blockers.
If we analyze the anticoagulation therapy according to the type of AF, we observe that the prevalence of anticoagulation among patients with known AF (52 cases) is 71.2%, whereas 3 of the 17 patients with previously undiagnosed AF (17.6%) received anticoagulation for other reasons (Table 3). The rate of anticoagulation in the group of patients with a previous episode of AF and in sinus rhythm at the time of the examination was 37.8% (14 patients). We observed that 73 of the 106 patients with AF had a CHADS2 score >1 (68.9%), with a higher proportion (80.8%) in the group with persistent AF (Table 3). If we analyze the adjustment of the anticoagulation therapy as defined by the patients in whom anticoagulation is indicated by a CHADS2 >1 and who are receiving treatment, we observe that 76.2% of the group with permanent AF, 41.7% of the group with a previous episode and 14.3% of the group with undiagnosed AF were correctly treated. Anticoagulation therapy was contraindicated in only three patients with AF (2.8%).
In the multivariate analysis, the factors associated with the presence of AF (during the ECG or a previous episode) were age, structural heart disease (coronary artery disease or heart failure), alcohol consumption and LVH due to ventricular overload (Table 4). In contrast, physical exercise was associated with a reduction in the risk of AF, nearly achieving significance.
DISCUSSION
Our report is one of the few studies carried out in Spain that analyze the prevalence and the antithrombotic treatment of AF in a population characterized as being hypertensive and over 65 years of age, regardless of the type of AF (previous history or ongoing AF) and it demonstrated a total prevalence of 10.3%, with a very high rate of use of antithrombotic drugs, especially among the patients with known AF detectable in the ECG. Moreover, it reflects the fact that, in 1 of 4 patients with AF according to the ECG, the presence of said arrhythmia had not been detected, with the therapeutic and prognostic implications that this circumstance entails.
The CARDIOTENS 1999 study, with a cross-sectional design and carried out in the primary care and specialized settings in Spain, showed an overall prevalence of chronic AF of 4.8%, which reached 11.1% among individuals of >80 years of age.13 In this study, the diagnosis of AF was based on the background gathered from the medical records, as there was no protocol calling for the performance of an ECG, nor were the cases of paroxysmal or isolated AF recorded, a circumstance that may limit the estimate of the true prevalence of the arrhythmia. Atrial fibrillation is characterized by its temporal pattern, with periods in which the patient is in sinus rhythm; thus the need to search for this arrhythmia actively and repeatedly, especially in patients at risk, in order to reduce cardioembolic risk by means of the proper treatment. Another of the epidemiological studies carried out in Spain, the PREV-ICTUS study, involving a population of 7108 subjects over the age of 60 years (73% of them with HT), reported the observation of AF in the ECG of 8.5% of the patients, a prevalence that increases linearly with age, from 4.5% in subjects between the ages of 60 and 64 years to up to 16.5% in those over the age of 85 years.14 In this analysis, the patients with a previous episode of AF were not taken into account. It is surprising that the incidence of AF according to the ECG findings was slightly higher than that documented in our study, despite the fact that the risk was higher in our population given that all the patients were hypertensive. Evidently, we can not compare these results because the analysis of the ECG in the PREV-ICTUS study was not centralized and the reading was carried out by one of the researchers, with the limitations that this circumstance can entail. One explanation that can justify this lower prevalence of AF in the ECG in our population is the high rate of use of drugs that block the renin-angiotensin-aldosterone axis for the treatment of HT. In this respect, numerous published studies have shown a reduction in the incidence of AF with the use of angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB).15,16
From a practical point of view, one of the major advances in the treatment of patients with AF over the past few decades has been the demonstration of the fact that the incidence of embolic episodes is reduced by the treatment of high-risk patients with anticoagulation therapy. In large randomized studies on the prevention of stroke in AF, the major associated risk factors were advanced age, female sex, previous stroke or transient ischemic attack, HT and diabetes mellitus.17 A number of studies report rates of anticoagulation therapy in patients with AF of around 50%.18 Our results reveal a very high rate of use of these drugs among patients with AF according to the ECG, especially in the group of known AF, surpassing that reported in other studies carried out a few years ago in Spain. In a subanalysis of the CARDIOTENS study performed in 999 patients with AF, the use rate of antithrombotic agents was 33%, with lower levels in the primary care setting, and significantly lower levels among the oldest patients,19 despite the fact that it is in the latter population that the greatest net benefit is produced.20 The fear of falls and the risk of bleeding constitute the major limiting factor when it comes to deciding not to anticoagulate elderly patients.21 In this respect, a study was recently published that indicates that anticoagulation therapy is acceptable in patients over 80 years of age given the low risk if adequate follow-up of the treatment is carried out.22 This increase in the use of antithrombotic drugs in patients with AF over the past decade has also been corroborated in other countries.
A striking finding in our study is the lesser use of antithrombotic drugs in patients with previous episodes of AF who are in sinus rhythm and in whom they are indicated because of a CHADS2 score >1 (41.7%), despite the fact that the latest guidelines clearly indicate that the subtype of AF should not influence the decision as to whether or not to anticoagulate a patient and that this decision should be based on the risk factors and contraindications.23 This fact may reflect the limited awareness among physicians of the cardioembolic risk in these situations. Data from the Euro Heart Survey on Atrial Fibrillation corroborate this lower use of oral anticoagulation therapy in patients with paroxysmal AF (51%) with respect to those with persistent AF (80%) and permanent AF (76%), despite the fact that the researchers observed that the risk of stroke associated with paroxysmal AF is at least comparable to that found in persistent and permanent AF.24 These findings have also been confirmed by other studies carried out in different populations.25,26
Limitations
One of the major limitations to studies of this type is the number of subjects recruited and the degree to which our sample represents the universe of patients with this disease, since selection bias will always exist, taking into account the fact that the most seriously ill and motivated patients are those that usually come in contact with the health care system and are probably more highly represented in these studies. Despite this selection bias, our study shows the true management of the cardioembolic prevention of this arrhythmia in our setting, far from the large clinical trials. On the other hand, the cross-sectional nature of the study impedes the proper evaluation of cause and effect and can lead to unexpected associations, such as a better control of arterial blood pressure in patients with AF. Despite this circumstance, these limitations do not invalidate the results of our study, in which we analyze the presence of AF through the centralized analysis of the ECG in the hypertensive patient aged 65 years or older in a Mediterranean population.
CONCLUSIONS
Our report shows a slightly lower prevalence of AF among hypertensive patients than that observed in other studies carried out in Spain, and reflects its strong association with advanced age, structural heart disease (including LVH according to the ECG) and alcohol consumption. In addition, it indicates a high rate of use of antithrombotic drugs (especially anticoagulants) among patients with known AF detected in the ECG, a circumstance that translates into a high awareness of the cardioembolic risk associated with this condition on the part of physicians. In contrast, less than half of the patients with a previous episode of AF and in sinus rhythm receive this treatment, despite their having a significant risk of stroke (CHADS2 score <1).
ACKNOWLEDGMENTS
The authors wish to thank the laboratory Lácer, for its contribution, help and constant dedication to this project. They also thank all the participating researchers, without whose daily work and effort the performance of this study would not have been possible.
FAPRES STUDY RESEARCHERS
Juan Alberola, Vicente Javier; Maestre Amat, Luis; Mateo Limiñana, José Manuel; Monleón Gómez, José; Montagud Moncho, Miguel; Guinot Martínez, Enrique; Gamón Pastor, José Blas; Salanova Penalba, Alejandro; Sanchis Domenech, Carlos; Pallares Carratala, Vicente; Palacios Del Cerro, Antonio; Pérez Martínez, Rafael; Baudet Dejean, Chantal; Pérez Alonso, Manuel; Fácila Rubio, Lorenzo; Sipan Sarrión, Yolanda; Saro Pérez, Eugenia; Villaro Gumpert, Juan; Cabrera Ferriols, M. Ángeles; Fraile Fraile, Belén; Carbonell Franco, Francisco; Cornejo Mari, Francisco Javier; Barberá Comes, Javier; Quiles Añon, Fernando; Llisterri Caro, José Luis; Almenar Cubells, Enrique; Casado González, Joaquín; Godoy Rocati, Diego; Martínez Guerola, Carmen; Bonet García, Jorge Alejo; Blázquez Encinar, Julio César; Botella Estrada, Carlos; Saen Alcoy, Montepio; Almarcha Pérez, Natividad; Salanova Chilet, Lorena; Torres Ferrando, Miquel; Debon Belda, Manuel; Fluixa Carrascosa, Carlos; Aznar Baset, Lucía; Vivancos Aparicio, Diego; Pineda Cuenca, Manuel; Obarrio Moreno, Alicia; Núñez Jorge, Carlos; Matoses Nacher, Daniel; Baño Aracil, Manuel; Balanza Garzón, Alicia; García Palomar, Carlos; Peña Forcada, Enrique; Raga Casasus, José; Martínez Lahuerta, Juan; Mendizábal Núñez, Andrea; Santos Alonso, Eufrosina; Corbí Pascual, Miguel; Lillo Sánchez, Antonio; Martorell Adsuara, Vicente; Sánchez Ruiz, Tomás; Ortiz Díaz, Francisco; Llinares Orts, José Francisco; Lahoz Ferrer, Julio; Morillas Blasco, Pedro; Pertusa Martínez, Salvador; Manclus Montoya, Carlos; Adriá Mico, José Manuel; Llaudes Soler, Ricardo; Castillo Castillo, Jesús; Llopis Martínez, Francisco; Ruiz De La Prada Abarzuza, Ignacio; Nebot Rico, Lidia.
ABBREVIATIONS
AF: atrial fibrillation
ECG: electrocardiogram
HT: hypertension
LVH: left ventricular hypertrophy
This study has been carried out with an unconditional grant from the Spanish laboratories Lácer.
Correspondence: Dr. P.J. Morillas Blasco.
Sección de Cardiología. Hospital Universitario de San Juan.
Ctra. Nacional 332 Alicante-Valencia, s/n. 03550 Sant Joan d'Alacant. Alicante. España.
E-mail: pedromorillas@teleline.es
Received November 7, 2009.
Accepted for publication February 22, 2010.