Keywords
INTRODUCTION
Cardiac pseudoaneurysm is an extremely rare lesion. Following a small cardiac rupture, the blood remains in an adjacent cavity, whose wall is composed of pericardium, fibrin or synthetic surgical materials. The pseudoaneurysm gradually increases in size, often compressing the nearby structures. Unlike true aneurysms, the absence of myocardial tissue in the wall of a false aneurysm implies a considerable risk of rupture.1 Pseudoaneurysm has been described in children after right ventriculotomy, usually caused by dehiscence of the sutures used to place materials between the ventricle and the pulmonary artery.2,3
CASE STUDY
A 2-year-old infant girl with a history of complete repair of tetralogy of Fallot at 4 months of age was seen. In this prior surgery, the outflow tract was reconstructed with autologous pericardium in the posterior wall and bovine pericardium in the anterior wall (Sulzer Carbomedics, CF 412R), in order to connect the right ventricle with the pulmonary artery. No incision was made in the hypoplastic pulmonary annulus, since it was traversed by the left coronary artery, which arose from the single anterior coronary. During follow-up, the patient developed stenosis of the distal suture of the outflow tract in the pulmonary artery. She was admitted to the hospital for precordial pain, pallor and sweating while walking that abated with rest.
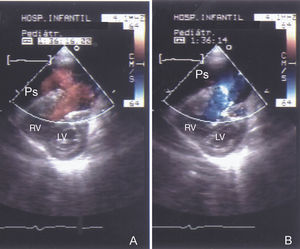
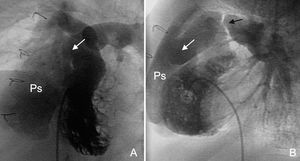
The examination revealed labored breathing, mild bilateral swelling of the eyelids and Grade III/VI pulmonary systolic ejection murmur. There was no evidence of myocardial ischemia in the electrocardiogram, which showed right bundle-branch block. Cardiac enzymes were normal. Review of the serial chest x-rays revealed progressive growth of the right cardiac contour over the previous 8 months. The diagnosis was based on echocardiography (Figure 1), and later confirmed by right ventriculography (Figure 2). The hemodynamic study also showed increased right ventricular diastolic pressure (40/8-15 mm Hg) and increased pressure in the right atrium (18/12; mean, 15 mm Hg).
Figure 1. Two-dimensional color Doppler echocardiography. Short-axis parasternal view. Rupture of the pericardial tunnel anterior wall, connecting the tunnel to the pseudoaneurysm (Ps) cavity. Bidirectional (back-and-forth) blood flow between the right ventricular outflow tract and the Ps, characteristic of this lesion: A. Systole: from the right ventricle toward the Ps. B. Diastole: flow in the opposite direction. RV indicates right ventricle; LV, left ventricle.
Figure 2. Right ventriculography. Four-chamber (A) and lateral (B) views. Note contrast outflow in the right ventricular outflow tract (white arrow) with opacification of a large cavity immediately below the sternum, anterior to the right ventricle (Ps). The lateral view shows considerable narrowing at the pulmonary suture of the pericardial conduit (black arrow).
The patient underwent emergency cardiopulmonary bypass and femoral artery cannulation. The pericardial conduit, which presented an anterior wall rupture, was replaced with a cryopreserved pulmonary homograft. There were no postoperative complications.
DISCUSSION
Formation of a pseudoaneurysm can have catastrophic consequences, including rupture, infection, thromboembolism, syncope, mediastinal compression, etc; hence repair is of vital importance.4 In the few references on this subject in the literature, the main causes cited are elevated residual right ventricular pressures and the use of patches, homografts, or conduits to reconstruct the outflow tract, with dehiscence of the surgical sutures being the cause of the pseudoaneurysm.2,5,6 We are not aware of any case reports, such as ours, in which the patient survived after the bovine pericardial patch had ruptured through the middle. Because cardiac rupture probably occurs in a slow, contained manner, patients tend to be asymptomatic for several months, and therefore a high index of suspicion is required when radiological studies show new mediastinal masses adjacent to the heart or localized increases in size. The symptoms tend to present when the pseudoaneurysm is advanced. In our patient, precordial pain was caused by detachment of the pericardium from the roof of the right atrium several months after silent rupture of the patch.
Echocardiography is an excellent diagnostic method7; however, we believe that it is important to use catheterization to study the right chamber pressures. In our case, the elevated end-diastolic ventricular and atrial pressures may have been influenced by limited filling in both chambers, secondary to compression by the adjacent pseudoaneurysm. Catheterization is also useful to delimit the location and anatomical relationships of the pseudoaneurysm, particularly with regard to the sternum. When resternotomy is the approach used for repair of a retrosternal pseudoaneurysm, femoral artery, and central vein cannulation must be used for circulatory bypass prior to the sternal incision.8 We performed arterial perfusion using the femoral route, establishing a right bypass with aspiration through the orifice of the pseudoaneurysm until the right atrium was cannulated. The procedure was performed without clamping the aorta and with the heart beating. Magnetic resonance imaging has recently shown to be an excellent alternative for anatomic study of this lesion.9
Correspondence: Dr. A. Moruno Tirado.
Sección de Hemodinámica. Hospital Infantil Virgen del Rocío.
Avda. Manuel Siurot, s/n. 41013 Sevilla. España.