To the Editor:
Platypnea-orthodeoxia syndrome is a rare entity characterized by dyspnea (platypnea) and hypoxemia with arterial oxygen desaturation (orthodeoxia) with orthostasis, both of which improve with recumbency. It is frequently associated with the presence of a patent foramen ovale (PFO). We describe the case of a patient who presented with this syndrome 2 months after pneumonectomy.
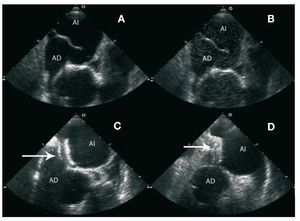
The patient was a 70-year-old male without cardiovascular risk factors or heart disease who was allergic to aspirin. He had undergone a partial right pneumonectomy for a malignant lung nodule. One month after surgery, he was referred with dyspnea at minimal effort and even at rest that improved with recumbency. On admission, there was notable arterial oxygen saturation at 83% in the supine position (with oxygen at 4 L), which fell to 67% on standing. Physical examination revealed moderate kyphoscoliosis, acrocyanosis, and no cardiac murmurs on auscultation. The electrocardiogram (ECG) showed sinus rhythm at 75 beats / min with a pattern of right bundle branch block and anterior hemiblock. The chest x-ray showed clear lung fields, aortic elongation, absence of cardiomegaly, and elevated right hemidiaphragm. Spirometry revealed a 79% Tiffenau rate. Pulmonary embolism was ruled out via ventilation-perfusion scintigraphy and high resolution computed tomography. The transthoracic echocardiogram (TTE) showed a slightly dilated aortic root, with absence of pulmonary hypertension, a left ventricle of normal dimensions, and preserved systolic function. Transesophageal echocardiography (TEE) revealed basal septal aneurysm with massive right-left transfer of atrial contrast (agitated saline) through the PFO (Figure 1A-B). The patient underwent percutaneous closure of PFO without complications using a 25 mm Amplatzer device controlled by intracardiac ultrasound. TEE showed that the device was appropriately positioned in the atrial septum (Figure 1C), without evidence of residual shunt after injection of agitated saline (Figure 1D).
Figure 1. A: transesophageal echocardiography (TEE) at 51° showing the atrial septal aneurysm and a large patent foramen ovale (PFO). B: evidence of left-right shunting after injection of contrast (agitated saline) from the right atrium (RA) to the left atrium (LA). C: TEE image at 21° showing the Amplatzer device (arrow) after percutaneous closure of PFO. D: no shunting (injection of contrast) after percutaneous closure of PFO.
The patient showed marked clinical improvement; acrocyanosis resolved and arterial oxygen saturation increased to 92%. At discharge, 6 months treatment with clopidogrel 75 mg daily was prescribed. The patient was asymptomatic at 3 years follow-up.
Dyspnea and hypoxemia are frequently present after pneumonectomy. When respiratory causes are ruled out, less frequent etiologies should also be ruled out. Platypnea-orthodeoxia syndrome is relatively rare and presents with dyspnea and arterial desaturation in an upright position.1 It is associated with the presence of PFO. The PFO is the usual cause of right-left shunting when pulmonary hypertension is present. In its absence, various mechanisms have been described.2,3 These mechanisms could involve abnormal anatomic relationships between inferior vena cava (IVC) atrial septum. With orthostatism, venous flow is preferentially directed from the IVC through the PFO into the left atrium, especially if a persistent eustachian valve is present. This mechanism is related to several conditions, such as aortic root dilation,4 kyphoscoliosis, paralysis of the right hemidiaphragm or pneumonectomy.5 Our patient had several of these conditions. It is likely that the platypnea-orthodeoxia syndrome is more common than is diagnosed. Therefore, given clinical suspicion and some predisposing factors, a TTE and TEE should be performed to rule out PFO. The treatment of choice is the closure of the defect with a special device using a percutaneous approach.6 Complications are minimal and the success rate is high. As demonstrated in this case, it is also accompanied by clear symptomatic improvement.