To the Editor:
Acute myocarditis is a rare disease with a very diverse etiology. It produces a wide spectrum of clinical manifestations and in some cases has a fulminant course. The degree of echocardiographic impairment of myocardial contractility is also highly variable, ranging from no abnormalities to a severe deterioration in systolic function. The pattern of the condition may be diffuse or focal, and it can sometimes simulate ischemia, infarction or primary cardiomyopathy.1
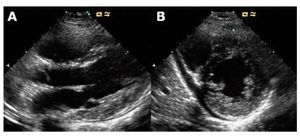
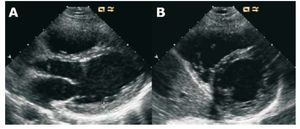
We report on a patient of 17 years with no relevant medical history who was admitted to the emergency room with a clinical profile of asthenia, fever up to 38.3°C, and chest pain characteristic of pericarditis lasting 24 h. The physical examination was normal. The electrocardiogram showed a diffuse, concave increase in ST. Analysis showed leukocytosis with left shift but without eosinophilia and elevation of creatine kinase (CK), 390 U/L, and troponin-I (TnI), 8.96 ng/mL. After a diagnosis of acute myopericarditis, probably viral, treatment was started with high-dose salicylates and the patient was admitted to the ward. The rheumatological test battery was normal. We performed an echocardiogram, which showed a diffuse, light pericardial effusion as well as notable thickening of the basal and middle segments of the posterior wall of the left ventricle (LV). Thickening was up to 13 mm with extension to the posterior papillary muscle. Mild hypokinesia was also observed in these segments (Figure 1). The rest of the myocardium showed normal thickness and contractility (septum, 9 mm); the ejection fraction was also normal (65%). The patient progressed favorably; the pain disappeared and there was a decrease in CK and TnI, after a peak of 436 U/L and 13.5 ng/mL, respectively. An echocardiogram performed 5 days later showed normalization of the thickness (9 mm) and contractility of the posterior wall infarction and complete resolution of the effusion (Figure 2). Cardiac magnetic resonance imaging (MRI) during the acute phase and convalescence showed some points of late gadolinium enhancement in the LV lateral wall; myocardial thickness and contractility were normal.
Figure 1. Echocardiogram on admission. Parasternal long axis view (A) and short axis (B) in diastole. There is an asymmetrical thickening of the posterior wall involving the posterior papillary muscle, and slight pericardial effusion.
Figure 2. Echocardiogram 5 days after admission. Parasternal long axis view (A) and short axis (B) in diastole. Normalization of the myocardial thickness in the posterior wall and posterior papillary and resolution of the pericardial effusion can be seen.
Localized and diffuse transient myocardial thickening may be observed in acute myocarditis with interstitial edema being postulated as the most likely pathologic substrate. In a series consisting of 25 patients with acute myocarditis who underwent echocardiogram and endomyocardial biopsy (in the acute phase and during convalescence), a significant decrease in myocardial thickness was observed between the acute and the convalescent phase, both in the septum (from 14.3 [3.7] to 9.7 [1.7] mm) and in the posterior wall (13.3 [2.4] to 10.2 [1.7] mm). The reduction of the edema shown by the biopsy was also significant: interstitial edema was observed in 88% of patients in the acute phase compared to only 28% in the convalescent phase.2 In another study of 25 patients with lymphocytic myocarditis, the prognostic significance of myocardial thickness measured in the acute phase was investigated, and it was found that thickness was considerably greater in the group that evolved into a fulminant myocarditis compared to the group which did not evolve to a fulminant condition.3
Transient myocardial thickening is an uncommon finding that should be recognized in patients with acute myocarditis. It is due to interstitial edema and appears to have a poor prognosis, as it has been associated with a fulminant course. In the echocardiographic study, it can mimic hypertrophic cardiomyopathy. In this regard, MRI can be useful because of its higher sensitivity in detecting edema. It can also provide additional prognostic data on aspects such as the extension of the inflammation.4 In the absence of MRI, checking resolution using serial echocardiograms would be a better option than endomyocardial biopsies because of their greater safety.