To the Editor,
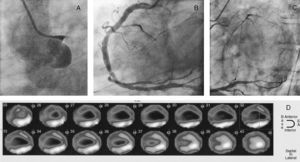
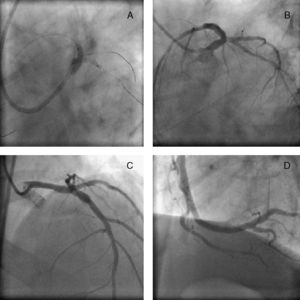
A 54-year-old, Caucasian, hypertensive, cigarette smoking man with hypercholesterolemia and without previous cardiovascular events or history of chest pain was hospitalized for dyspnea and increased New York Heart Association (NYHA) scale. Both physical and electrocardiogram examination were within normal limits. Echocardiogram showed anterior-apical akinesia and hipokinesia of the remaining segments with severe left ventricular dysfunction: left ventricular ejection fraction (LVEF) 20%. Cardiac catheterization was then performed. Left main coronary artery (LMCA) was occluded at its very proximal portion (Figure 1A). Right coronary artery (RCA) had a severe stenosis in the mid-distal segment (Figure 1B). The collateral flow ran from septal branches to the left anterior descending (LAD) and from lateral branches to the left circumflex (LCX) showing a left coronary artery without stenotic lesions (Figure 1C). A myocardial single photon emission tomography (SPECT) showed preserved viability in the inferior-lateral portion; no perfusion was detected in the anterior-apical segments, suggesting necrosis (Figure 1D). The patient was then evaluated by cardiac surgeons who contraindicated a coronary artery bypass graft due to the absence of viability in the anterior wall. We then performed a percutaneous coronary intervention (PCI) of RCA, following an attempted PCI of the LMCA. The decision was based on no history of myocardial infarction, suggesting presence of severely hypoperfused but potentially still viable myocardium. The procedure was successful: we implanted a Paclitaxel-eluting stent 3.5×28mm on LMCA-LAD, followed by a kissing balloon on LAD-LCX (Figure 2A-C); subsequent intravascular ultrasound examination guided expansion optimization. Two days later, we performed a PCI of RCA using a bare metal stent 4.5×12mm (Figure 2D). Intraprocedural intra-aortic balloon pump device could not be used due to the occlusion of the left common iliac artery. The patient was then discharged asymptomatic with clopidogrel, acetylsalicylic acid, beta blocker, angiotensine-converting enzyme inhibitor-I, and statin as pharmacological treatment. At 1 month follow-up visit he was asymptomatic and reported no cardiac events; the echocardiogram showed a slight LVEF improvement (26%); no change was made in pharmacological therapy. At 4 months follow-up the patient reported an improvement in physical capacity, in accordance with an echocardiogram showing further LVEF improvement (43%). No inducible ischemia was detected in an ECG treadmill test at 12 months follow-up. The patient was totally asymptomatic and the echocardiogram confirmed the improvement in the LVEF (46%). Chronic total occlusion (CTO) of the LMCA is a rare but critical condition that can exist only in patients with a dominant RCA and good collateral formation.1, 2, 3 The clinical course of this condition is varied4, 5 and its correct treatment is still unclear, debating between percutaneous and surgical revascularization. In the case we present, however, coronary artery bypass graftwas avoided because of the absence of perfusion in the anterior-apical segments (revealed by SPECT) and the high operative risk due to low LVEF.
Figure 1. A-C: Admission angiography. D: Admission single photon emission tomography.
Figure 2. A: Percutaneous coronary intervention on left main coronary artery. B and C: Left main coronary artery after percutaneous coronary intervention. D: Right coronary artery after percutaneous coronary intervention.
The PCI was programmed with an Intraprocedural intra-aortic balloon pump as a supportive device that could not be used because of the occlusion of the left common iliac artery. In this case, we had no hemodynamic complications or arrhythmic events, probably due to the presence of a CTO with a well collateralized LMCA (“protected LMCA”). The most important aspect of this case is the improvement of LVEF. Even though SPECT showed a large necrotic portion, this patient received an important benefit from revascularization, probably because the LMCA occlusion did not occur acutely but was a chronic progressive condition with the development of good collateral flow that lead to severely hypo-perfused but still viable myocardium.
Although we did not perform a pre-PCI cardiac positron emission tomography or a follow up SPECT, myocardial hibernation remains the most likely hypothesis explaining the improvement of the left ventricular systolic function.
Corresponding author: gioel.gabrio.secco@gmail.com