To the Editor,
Stress echocardiography offers diagnostic capacity for the detection of myocardial ischemia that is superior to stress testing with an electrocardiogram (ECG), irrespective of patient age or sex,1 and its use is preferable to dobutamine stress echocardiography in subjects able to exercise.2 The test is indicated in the diagnosis of ischemic heart disease in patients with suspected coronary disease or pathological baseline ECG and inconclusive conventional stress testing; in this type of patient, the test provides relevant prognostic information to predict mortality and major cardiovascular events.3
We describe a 59-year-old man with hypertension as the only cardiovascular risk factor. Some years previously, he had experienced an angina-like episode; however, the stress test was negative for ischemia and he was asymptomatic afterwards. Recently, the patient was again referred to our hospital for stress echocardiography following an episode of chest pain at rest. An echocardiographic study at rest showed no regional contractility abnormalities.
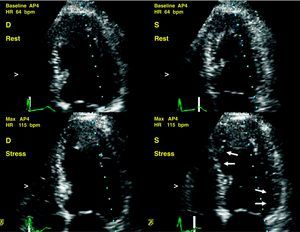
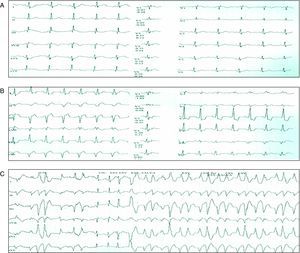
During the cycle-ergometer test without beta blockers, the patient completed World Health Organization Stage V (125W) but did not achieve submaximal heart rate and, therefore, 1 mg of intravenous atropine was administered. At that point he developed apical septal, lateral basal, and posterior hypokinesis (Figure 1) and symptoms of angina with concomitant vegetative syndrome. The surface electrocardiogram showed ST-segment depression >1 mm in leads I, aVL, and V3-V4 and development of bifascicular block (complete right bundle-branch block, bundle of His, and left anterior bundle-branch block), followed by runs of polymorphic ventricular tachycardia (Figure 2). Once intravenous atenolol was administered, the ECG abnormalities and regional contractility returned to normal, and the patient remained asymptomatic. The test was considered positive, and the patient was admitted to the cardiology department to investigate potential coronary disease.
Figure 1. Stress echocardiography. Development of apical septal, lateral basal, and posterior hypokinesis during maximum exertion following the administration of intravenous atropine (arrows). bpm, beats per minute; D, end-diastolic; HR, heart rate; S, end-systolic.
Figure 2. A, electrocardiogram at rest. B, electrocardiogram following atropine administration in World Health Organization Stage 5: ST-segment depression >1 mm in leads I, aVL, and V3-V4 and development of bifascicular block (complete right bundle-branch block, bundle of His, and left anterior bundle-branch block). C, runs of polymorphic ventricular tachycardia.
Although the enzyme panel on admission showed a maximum troponin I peak of 0.73 ng/mL (normal values, <0.3 ng/mL), the hemodynamic study found coronary arteries without significant stenosis. A subsequent cardiac magnetic resonance showed no significant findings. The patient was discharged with follow-up by the outpatient service and remained asymptomatic in the following months.
The use of atropine during pharmacological stress echocardiography to achieve submaximal heart rate is a regular practice that is described in the clinical practice guidelines and improves test sensitivity. Nonetheless, standard use during stress echocardiography is not described in the guidelines, and the potentially serious adverse effects that result are not reported in the literature, despite routine use in some echocardiography laboratories. Although the safety of the various stress echocardiography modalities has been previously evaluated in our setting,4 with similar percentages of complications as in previous series,5 including ventricular arrhythmia (<0.5%), these studies do not include the practice of mixed protocols such as the one reflected in our case. Moreover, drugs administered during physiological stress to enhance test sensitivity and increase the heart rate may conversely reduce specificity, as observed after coronary angiography.
The complication described in the present case illustrates the risk of triggering ventricular arrhythmia during maximum stress caused by administering atropine, and could raise questions about routine use in this clinical context.
Corresponding author: paya_rafser@gva.es