Keywords
INTRODUCTION
Optical coherence tomography (OCT) is a novel intracoronary diagnostic technique that offers a resolution of approximately 10 to 20 µm, around 10 times higher than that of other techniques, such as intravascular ultrasound (IVUS). Previous studies have assessed the application of OCT in the characterization of the different components of atherosclerotic plaques both in vitro and in vivo.1,2 This technique has been found to have a high sensitivity and specific than histology for the classification of the different types of atherosclerotic plaques.3 Given its high resolution, OCT makes it possible to identify plaques covered by a thin fibrous caps, less than 65 µm thick, referred to as thin cap fibroatheromas, which are more prone to rupture and to provoking acute coronary syndromes.4 It has also been utilized to estimate the collagen and macrophage content in atherosclerotic plaques.5,6 On the other hand, OCT has been applied to assess the results of stent implantation in patients who have undergone a percutaneous coronary intervention (PCI).7-9
The purpose of this report is to evaluate the outcome, according to OCT studies, in patients who underwent PCI in our center, whose angiographic images were optimal.
METHODS
Six patients who underwent PCI and presented optimal angiographic results after stent implantation (defined as a stenosis less than 20% in diameter, TIMI 3 distal flow, and the absence of abnormal images on visual estimation) were studied by OCT. In 2 patients, the study had been carried out prior to the PCI.
The PCI was performed according to the standard procedure. Four patients underwent balloon predilatation. The mean reference diameter at the level of the lesion, determined by quantitative angiography, was 3.01 mm and the mean diameter of the implanted stents was 3.3 mm (no significant differences); they were implanted at a mean pressure of 15 atm. None of the patients underwent balloon overdilation as the angiographic images did not appear to indicate the need for it.
The OCT study was then performed. A coaxial balloon catheter (Helios OBC, Lightlab Imaging, Inc., Westford, MA, USA) was advanced over an angioplasty guidewire to a site distal to the implanted stent. The guidewire was then withdrawn and the OCT probe (ImageWire, Lightlab Imaging, Inc., Westford, MA, USA) was advanced through the balloon to position it at least 5 mm distal to the stent. The balloon was withdrawn to a healthy segment proximal to the stent, it was inflated to a pressure of 0.5 to 0.6 atm, and the occlusion of the coronary flow was verified. Then, while flushing with saline was performed by means of manual injection at a constant rate via the balloon, the OCT probe was pulled back automatically at a rate of 1 mm/s. In those cases in which it was considered necessary, the pullback was repeated after leaving the deflated balloon in place for a few minutes. Finally, the balloon was deflated and withdrawn, together with the OCT probe, from the coronary tree and the absence of complications was verified.
The images were stored and subsequently analyzed in the system console (Lightlab, model M2, Lightlab Imaging, Inc., Westford, MA, USA). Mainly, the presence of dissections at the stent edges, tissue prolapse through stent struts and zones of incomplete stent apposition were evaluated, as was the presence of thin cap fibroatheromas in other segments of the vessel studied and the presence of any other abnormal image. Dissection was considered to be present when the image within the stent or adjacent to it showed a flap that was clearly differentiated from the rest of the tissue. Tissue prolapse was defined as the protrusion of tissue through an imaginary arch connecting 2 adjacent struts. Incomplete stent apposition was identified as a clear separation between at least one stent strut and the vessel wall. A thin cap fibroatheroma was defined as a homogeneous area in the arterial wall with a low refractive index, separated from the vessel lumen by a capsule having a high refractive index and a thickness of less than 65 µm.
RESULTS
Six patients were included (5 men; mean age, 59 years): 3 were hypertensive, 2 were diabetics, 4 had dyslipidemia, and 4 were smokers. The PCI was performed to treat acute coronary syndrome in 4 patients and stable angina in 2. The circumflex artery was studied in 3 cases, right coronary artery in 2 and anterior descending coronary artery in 1; 3 patients received a drug eluting stent.
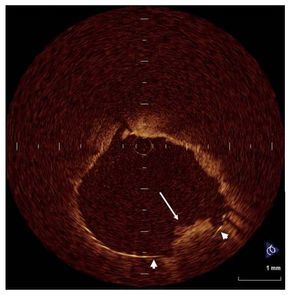
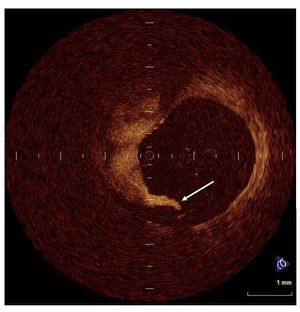
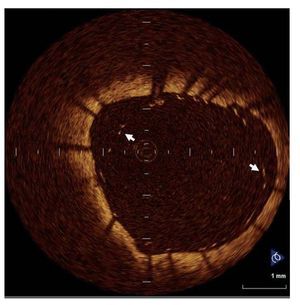
Thin cap fibroatheromas, with a fibrous caps measuring between 0.02 and 0.06 mm, were detected in 3 patients (in the region of the stenosis in the 2 patients who had undergone the study prior to PCI and in a region other than that of the stent in the third), although this circumstance was not related to the indication for PCI. Tissue prolapse through the stent struts was observed in all the patients (Figure 1), minor dissections at the edges of the stent in 4 (Figure 2), and incomplete apposition of the stent in another 4 patients (Figure 3). In incomplete stent apposition, the maximum separation between the stent and the arterial wall ranged between 0.04 and 0.5 mm and it involved up to 180o of the vessel circumference. Given the fact that, at the present time, the prognostic implications of these findings are unknown, balloon overdilation was not performed in any case. The formation of a thrombus around the OCT catheter was observed in 2 patients, despite anticoagulation with 70 to 100 IU of unfractionated heparin per kilogram body weight. None of the patients developed angina, electrocardiographic changes, or complications during the procedure. The OCT study prolonged the duration of the procedure in each patient by less than 5 minutes.
Figure 1. Tissue prolapse tissue (long arrow) into the stent (arrow heads).
Figure 2. Dissection (arrow) observed at the proximal edge of one of the stents.
Figure 3. Incomplete stent apposition along a large portion of the vessel wall (the arrows indicate some of the stent struts).
DISCUSSION
Making use of the high resolution of OCT, this report shows that PCI very frequently leaves zones of suboptimal result, despite a satisfactory angiographic image. Previous studies have demonstrated the superiority of OCT over IVUS for the assessment of the presence of tissue prolapse through the stent struts, minor dissections, and zones of incomplete stent apposition following PCI. In a series of 42 patients, Bouma et al7 detected tissue protrusion in 29 cases, dissections in 8, and incomplete stent apposition in 7 in the OCT studies, whereas, using IVUS, these findings were observed in only 12, 2, and 3 patients, respectively. In our study, despite the smaller number of patients, the percentage of cases in which these entities were identified was much higher, a circumstance that may be due to the difference in the technique employed to obtain OCT images. While we employed automatic pullback at a rate of 1 mm/second along the entire length of the stent, Bouma et al imaged the proximal and distal edges of the stent and the zone where the greatest stenosis was detected prior to implantation of the stent.
There are discrepancies when it comes to establishing the prognostic implication of these findings. While some studies have reported similar rates of adverse events in patients with and without acute incomplete stent apposition or plaque prolapse as assessed by IVUS,10-13 others have demonstrated a high prevalence of abnormal findings in the IVUS study following stent implantation in patients who develop acute stent thrombosis.14 At the present time, the prognostic implication of the detection of sites of suboptimal results following PCI, using OCT in patients with satisfactory angiographic images, is unknown.
In conclusion, given its high resolution, OCT makes it possible to detect zones of suboptimal results following PCI despite an optimal angiographic image. More extensive, long-term studies will be needed to assess the prognostic implications of these findings.
Correspondence: Dr. H. Gutiérrez.
Instituto de Ciencias del Corazón. Hospital Clínico Universitario. Avda. Ramón y Cajal, 3. 47005 Valladolid. España.
E-mail: hggmaire@gmail.com
Received September 7, 2007.
Accepted for publication December 19, 2007.