Keywords
INTRODUCTION
The existence of waiting lists in the public health system (particularly for outpatient care) has led to a search for new health care models. The aim of the "one-stop" outpatient clinic is to perform the examinations needed for diagnosis and treatment at a single visit.1,2 By avoiding delays for testing and the need to return, the number of patient visits is reduced.3,4 Cardiology is an ideal specialty for developing this type of outpatient clinic because the specialists who see the patient carry out most of the examinations.5
In 1996 a one-stop outpatient cardiology clinic was set up at our hospital to visit patients, perform the necessary tests on the same day, and complete a care report within 72 hours. The purpose of our study was to assess the results of 10 years' experience at our hospital, one of the pioneers in this health care model.
METHODS
The population attended was the entire cardiology population in the public health system for the catchment area (Osona, Catalonia, Spain), a region comprising 1191 km2 and a growing population (122 923 inhabitants in 1996 compared with 145 790 in 2006), distributed in 51 municipalities and 10 basic health areas.
To implement the model, a focus group of primary care physicians analyzed the criteria and system for referral, and the characteristics of the cardiologist's response. In order to provide appropriate facilities and staff, frequency ratios were estimated from previous years. An outpatient clinic was set up with 3 cardiologists for a 2.5-hour slot every day with a maximum daily scheduling of 4 visits per cardiologist. All initial visits, interconsultations, and referrals from primary care were scheduled at the clinic. The medical visit, electrocardiogram, and additional examinations ordered by the cardiologist (echocardiogram, exercise test, or Holter monitoring) were immediately performed during the same visit by the same cardiologist who saw the patient. All other cardiologic examinations were given preferential scheduling. Exercise tests were performed at the same visit with no delays, once informed consent had been obtained. If the patient was not wearing adequate footwear, then alternative solutions were used, for instance, undergoing the test while barefoot and wearing leggings.
Check-up or follow-up visits after admissions were handled by the same hospital cardiologists using separate, clearly differentiated appointment books for the one-stop outpatient clinic.
The medical records were integrated with primary care via a computer system that allowed access to the patients' history, reports, and examinations. All data were protected by the medical practitioner's digital signature.
An analysis was performed of the data collected prospectively over a 10-year period: frequency, origin, waiting time, reasons for visit, additional examinations, and destination after discharge. The ratio between one-stop and follow-up visits and hospital admissions was also assessed. Satisfaction surveys were performed among the primary care physicians before the clinic was set up and during follow-up. Statistical analyses were performed with the c2 test for categorical variables and the t test for quantitative variables. The opinion of the cardiologists who handled the activity was assessed by means of self-reported evaluations.
RESULTS
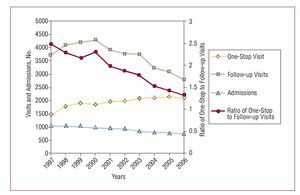
A total of 19 515 visits to the one-stop outpatient clinic were made between January 1997 and December 2006 (Table 1). The number of visits progressively increased, to eventually stabilize at about 2100 per year since 2003 (Figure 1). The mean wait for a visit was 3 days, well below the 60-day wait when the model was first used. The origin of the patients, reasons for the visit, tests performed, and destination after the visit are listed in Table 1.
The one-stop outpatient clinic reduced follow-up visits (from 4116 to 2782 per year) and the ratio of one-stop outpatient clinic/follow-up visits (from 2.49 to 1.33; P<.05).
From the time the one-stop outpatient clinic was opened, the number of hospital admissions in cardiology decreased every year, dropping from 1052 to 771 (Figure 1). In contrast, there were no significant differences in total hospital admissions (9686 vs 9761) or mean cardiology stay (7.59 vs 7.48 days).
Figure 1. Trend in the annual number of one-stop outpatient clinic visits, follow-up visits, and ratio of one-stop outpatient clinic visits/follow-up visits and hospital admissions. A significant decrease was observed in the ratio of one-stop outpatient clinic visits to follow-up visits relative to before implementing the model (P<.05).
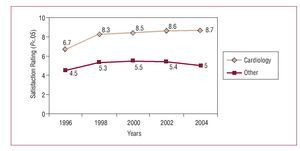
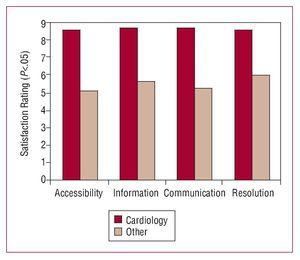
Satisfaction surveys among the primary care physicians (Figure 2) showed an improvement compared with baseline (6.7 [1.8] vs 8.7 [1.7]; P<.05). The aspects assessed (accessibility, information given to patients, communication with primary care physicians, and degree of problem resolution) were rated significantly higher than other specialties without a one-stop outpatient clinic (Figure 3). The opinion of the participating cardiologists is shown in Table 2.
Figure 2. Primary care satisfaction has improved since the one-stop outpatient cardiology clinic was opened (6.7 [1.8] vs 8.7 [1.7]; P<.05) and was higher than among specialties without a one-stop outpatient clinic.
Figure 3. Primary care satisfaction in terms of outpatient clinic accessibility, information received by patients, communication between health care levels, and degree of problem-solving, when the one-stop outpatient clinic is compared with the mean for other specialties without such a clinic. The indexes obtained by cardiology are significantly higher than those obtained by each of the other specialties (P<.05).
DISCUSSION
The development of organization models to decrease waiting time and streamline problem-solving is a health management objective. An ideal model for the various scenarios, which vary according to the organization and characteristics of the site, has not yet been found. The development of an outpatient clinic where examinations and treatment can be provided without any delay enhances health care efficiency1,6 and increases patient satisfaction.7 However, there are questions about its applicability in actual practice. Critics have argued that the system might encourage excessive consultations or referral of trivial medical problems.8
Each group of professionals should adapt the organization to their resources and setting; nevertheless, a close relationship with primary care is essential. Referral criteria should be established by consensus, and the primary care physician should assume long-term follow-up of the patient. By integrating these health care settings, the quality and continuity of the care provided will improve.9-11 In our case, access to the patients' medical records by both primary care and hospital staff provided information on examinations performed in the other setting, thereby enhancing efficiency by avoiding duplicate examinations.12
Cardiology hospitalizations significantly decreased over the 10-year history of the one-stop outpatient clinic, even though there were no changes in the organization of on-duty shifts (part of the internal medicine department) or hospitalizations handled by cardiologists, and no changes in total hospital admissions or mean stay, despite a 15.6% increase in the catchment population. Although a direct relationship between the one-stop outpatient clinic and the decrease in admissions cannot be established, we do feel this is a contributing factor.
Our study showed increased satisfaction among primary care physicians, strategically considered to be the client of specialized care by the one-stop outpatient clinic. Patient satisfaction was not assessed, an aspect that is a limitation of the study.
In our experience, the one-stop outpatient clinic is feasible in actual clinical practice and has been effectively used for 10 years. This model has reduced the waiting time for visits and eliminated the delay for examinations. Moreover, it was satisfactory for primary care physicians, reduced the number of follow-up visits and the need for patients to contact the hospital, and helped reduce hospital admissions.
Correspondence:
Dr. C. Falces.
Unidad de Cardiología. Hospital General de Vic.
Francesc Pla "El Vigatà", 1. 08500 Vic. Barcelona. España.
E-mail: 25364cfs@comb.es
Received July 15, 2007.
Accepted for publication October 4, 2007.