Two-dimensional speckle-tracking echocardiography is a novel tool to assess myocardial function. The purpose of this study was to evaluate left ventricular myocardial strain and rotation parameters by two-dimensional speckle-tracking echocardiography in a large group of healthy adults across a wide age range to establish their reference values and to assess the influence of age, sex, and hemodynamic factors.
MethodsTransthoracic echocardiograms were acquired in 247 healthy volunteers (139 women, 44 years [standard deviation, 16 years old] (range, 18-80 years). We measured longitudinal, circumferential, and radial peak systolic strain values, and left ventricular rotation and twist.
ResultsAverage values of global longitudinal, radial, and circumferential strain were –21.5% (standard deviation, 2.0%), 40.1% (standard deviation, 11.8%) and –22.2% (standard deviation, 3.4%), respectively. Longitudinal strain was significantly more negative in women, whereas radial and circumferential strain and rotational parameters were similar in both sexes. Accordingly, lower limits of normality for the strain components were –16.9% in men and –18.5% in women for longitudinal strain, and –15.4% for circumferential and 24.6% for radial strain, irrespective of sex. Longitudinal strain values were more negative at the base than at apical segments. Mean rotational values were –6.9° (standard deviation, 3.5°) for the base, 13.0° (standard deviation, 6.5°) for apical rotation, and 20.0° (standard deviation, 7.3°) for net twist.
ConclusionsWe report the comprehensive assessment of normal myocardial deformation and rotational mechanics in a large cohort of healthy volunteers. We found that women have more negative longitudinal strain, accounting for their higher left ventricular ejection fraction. Availability of reference values for these parameters may foster their implementation in the clinical routine.
Keywords
Left ventricular (LV) systolic function has been reported to be a powerful predictor of long-term survival in patients affected by a wide spectrum of cardiac diseases.1–3 The most widely used echocardiographic parameter to quantify LV systolic function has been LV ejection fraction (LVEF). While LVEF is a strong predictor of mortality and is used to select patients for device implantation4 surgical procedures5 and pharmacological treatments,6 it is extremely load-dependent, its measurement with echocardiography depends critically on operator expertise, and it is affected by significant intraobserver and interobserver variability.1
Global LV function is the result of the contraction and relaxation of a complex myocardial fiber architecture as a transmural continuum between 2 helical fiber geometries, where right-handed helical geometry in the subendocardial layer of myocardial wall gradually changes into left-handed geometry in the subepicardial layer.7,8 Myocardial fiber contraction determines changes of LV size and shape that are the result of concomitant longitudinal shortening, circumferential rotation, and radial thickening of the myocardium. The LVEF provides a global index of LV chamber function, ignoring the relative role of the different components of myocardial function (deformation in various directions and rotation), which may be affected to a different extent in different cardiac diseases even when LVEF is still in the normal range.9
Two-dimensional speckle-tracking echocardiography has recently emerged as a novel technique for objective and quantitative evaluation of global and regional myocardial function, independent of the angle of myocardial insonation.10–12 The myocardial deformation data (strain, ¿) are obtained by frame-by-frame automatic measurement of the distance between 2 points of each LV segment during the cardiac cycle along 3 dimensions (radial, R¿; circumferential, C¿, and longitudinal, L¿).
In addition, 2-dimensional speckle-tracking echocardiography can be used to assess LV rotational mechanics. LV rotation can be measured on 2-dimensional short-axis views acquired at base and apical levels to allow computation of twist and untwist. Several studies have related the dynamics of cardiac twist to systolic function of the LV.13,14
However, to be clinically useful, all these new parameters of myocardial and LV function need reference values that can be compared with data obtained from patients with suspected myocardial diseases. To date, reference values for deformation and rotational parameters are limited, heterogeneous, and sometimes inconsistent.15–18
Accordingly, we designed this prospective, observational study to use 2-dimensional speckle-tracking echocardiography in healthy volunteers to obtain the reference values for L¿, C¿, and R¿ as well as rotation and twist of the LV and to assess their relationship with sex and age.
METHODSStudy PopulationA cohort of 260 healthy Caucasian volunteers were prospectively recruited at a single tertiary center among hospital employees, fellows in training, their relatives, and individuals who underwent medical visits for driving or working licenses and met the inclusion criteria. Prospective criteria for recruitment included age >17 years, no history of cardiovascular or lung disease, no symptoms, absence of cardiovascular risk factors (ie, hypertension, smoking, diabetes, dyslipidemia), no cardioactive or vasoactive treatment, and normal results on electrocardiography and physical examination. Exclusion criteria were athletic training, pregnancy, and body mass index > 30kg/m2. Blood pressure (BP) was measured in all participants immediately before the echocardiographic examination. Height and weight were measured using a calibrated stadiometer and scale, and body surface area was calculated according to the Dubois and Dubois formula.19 Body mass index was calculated by dividing weight in kilograms by height in meters squared (kg/m2).
The study was approved by the University of Padova Ethics Committee (protocol number 2380 P, approved on October 6, 2011) and written informed consent was obtained from all volunteers before screening for study eligibility.
EchocardiographyStudy participants underwent a transthoracic echocardiographic examination in the left lateral recumbent position using a commercial ultrasound scanner (Vivid E9, GE Vingmed; Norway) equipped with a 2.5 MHz transducer. Two-dimensional (grayscale) views were obtained from the apical (4-, 2-chamber, and long-axis views) and parasternal (short-axis views at mitral valve, papillary muscle, and apical levels) approaches. Three consecutive cardiac cycles of each view were acquired during a breath hold at end-expiration. Special care was taken to obtain correct apical and short-axis images using standard anatomic landmarks and checking for foreshortening.10 To obtain the apical short-axis view, the transducer was placed on the chest wall at the level of the apical impulse and then moved one intercostal space upward and properly angulated in order to obtain a circular short-axis view of the LV with the smallest right ventricular area.20 All the images were obtained at a frame rate of 50 frames to 80 frames per second. Timing of aortic valve closure was assessed looking at the aortic valve motion in the long-axis apical view. All studies were digitally recorded and transferred to a dedicated workstation for further analysis.
The LV end-systolic and end-diastolic volumes were measured using the biplane disc summation rule and LVEF was calculated.21
Speckle-tracking imaging analysis was performed using a commercially available software (EchoPAC BT 12, GE-Vingmed; Norway). The endocardial border of the LV was manually traced slightly inside the myocardium; a second, larger, concentric circle was then automatically generated near the epicardium in order to include all the LV myocardium. Then, the software automatically divided each LV view into 6 equal segments and performed the speckle-tracking on a frame-to-frame basis.
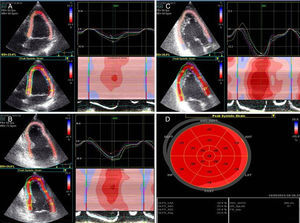
The 3 apical views were used for L¿ measurements. Short-axis views were used for measurement of R¿, C¿, and rotation. In particular, R¿ and C¿ were measured on the short-axis view obtained at the level of the papillary muscle (mid-ventricle), while rotation was measured on the short-axis views obtained at basal and apical levels. The software automatically divided each echocardiographic view into 6 segments, provided an automated tracking confirmation (which must be checked by the operator) and generated the ¿ values, expressed in percentage. If more than 3 of the 16 LV segments were inadequately tracked, the patient was excluded from the final analysis. Thirteen healthy individuals were excluded from analyses because of inadequate tracking. Myocardial L¿ values were displayed as a bull's-eye view (Figure 1).
Strain profiles from three apical views. Speckle-tracking echocardiography analyses in the apical 4- (A), 2-chamber (B) and apical long-axis (C) view with the respective speckle-tracking echocardiography measurements. Average segmental values in each segment are used to generate a “bull's-eye” display of left ventricular myocardial deformation (D).
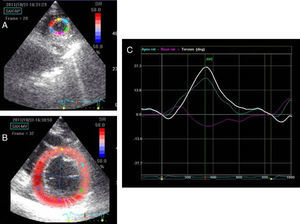
Rotation is an angular displacement of a myocardial segment in short-axis view around the LV longitudinal axis measured in a single plane.11 To measure LV rotation, the software defined the ventricular centroid for the mid-myocardial line on each frame and calculated the time domain rotation for each segment in both basal and apical short-axis views. Averaged LV rotations from 6 segments were used for the measurement of rotation at basal and apical levels. The tracking quality of each segment was indicated by the software and segments with insufficient tracking were excluded. The mean rotation was measured at aortic valve closure. Counterclockwise rotation is expressed with positive values when viewed from the apex, and clockwise rotation with negative values. Twist was calculated as the net difference between apical and basal rotation (Figure 2). Rotation and twist are expressed in degrees.
Statistical AnalysisNormal distribution of data was checked by Kolmogorov-Smirnov test. Data are summarized as mean (standard deviation [SD]). Enrolled participants were stratified according to age (18-35, 36-55, and 56-80 years) and sex. Comparison of strain values between men and women, among different age groups, and among different segments or walls were performed by unpaired 2-tailed Student t test and analysis of variance (ANOVA), as appropriate. The data were analyzed using SPSS for Windows version 17.0 (SPSS Inc.; Chicago, Illinois, United States) and p values <.05 were considered statistically significant.
ReproducibilityInterobserver reproducibility of strain measurements was assessed in 18 randomly selected patients by 2 independent observers who analyzed the data blind to the other observer results. Intraobserver reproducibility was assessed by 1 observer who analyzed the data sets twice, more than 1 month apart. For both intraobserver and interobserver reproducibility, Bland–Altman analyses (bias–limits of agreement) were performed and the intraclass correlation coefficient calculated.
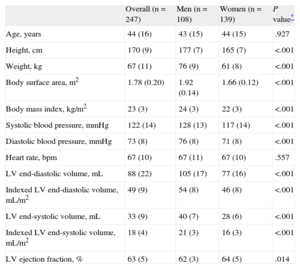
RESULTSA total of 247 healthy volunteers, 139 (56.2%) women, were enrolled in the study. Mean age was 44 (SD, 16 years) (range, 18-80 years). Table 1 shows the demographic characteristics and LV geometry and function of the study population. Men had larger body surface area and body mass index and higher BP values than women (all, P<.001). Men also had larger LV volumes; women had significantly higher LVEF (P=.014) than the men.
Demographics and Left Ventricular Geometry and Function of the Study Population
| Overall (n=247) | Men (n=108) | Women (n=139) | P value* | |
| Age, years | 44 (16) | 43 (15) | 44 (15) | .927 |
| Height, cm | 170 (9) | 177 (7) | 165 (7) | <.001 |
| Weight, kg | 67 (11) | 76 (9) | 61 (8) | <.001 |
| Body surface area, m2 | 1.78 (0.20) | 1.92 (0.14) | 1.66 (0.12) | <.001 |
| Body mass index, kg/m2 | 23 (3) | 24 (3) | 22 (3) | <.001 |
| Systolic blood pressure, mmHg | 122 (14) | 128 (13) | 117 (14) | <.001 |
| Diastolic blood pressure, mmHg | 73 (8) | 76 (8) | 71 (8) | <.001 |
| Heart rate, bpm | 67 (10) | 67 (11) | 67 (10) | .557 |
| LV end-diastolic volume, mL | 88 (22) | 105 (17) | 77 (16) | <.001 |
| Indexed LV end-diastolic volume, mL/m2 | 49 (9) | 54 (8) | 46 (8) | <.001 |
| LV end-systolic volume, mL | 33 (9) | 40 (7) | 28 (6) | <.001 |
| Indexed LV end-systolic volume, mL/m2 | 18 (4) | 21 (3) | 16 (3) | <.001 |
| LV ejection fraction, % | 63 (5) | 62 (3) | 64 (5) | .014 |
LV, left ventricular.
Data are expressed as mean (standard deviation).
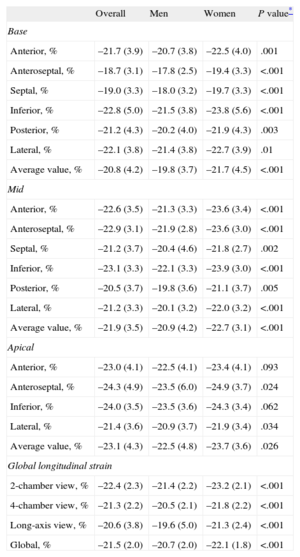
Global L¿ was –21.5 (SD, 2.0%) and it was more negative in women than in men (P<.001, Table 2), accounting for their higher LVEF. Therefore, the lower level of normality (average –2 SD) was –16.9% in men and –18.5% in women. Global L¿ was similar among the 3 age groups (P=.106) (Table 3).
Regional and Global Longitudinal Strain Values in the Overall Study Population and Compared Between Men and Women
| Overall | Men | Women | P value* | |
| Base | ||||
| Anterior, % | –21.7 (3.9) | –20.7 (3.8) | –22.5 (4.0) | .001 |
| Anteroseptal, % | –18.7 (3.1) | –17.8 (2.5) | –19.4 (3.3) | <.001 |
| Septal, % | –19.0 (3.3) | –18.0 (3.2) | –19.7 (3.3) | <.001 |
| Inferior, % | –22.8 (5.0) | –21.5 (3.8) | –23.8 (5.6) | <.001 |
| Posterior, % | –21.2 (4.3) | –20.2 (4.0) | –21.9 (4.3) | .003 |
| Lateral, % | –22.1 (3.8) | –21.4 (3.8) | –22.7 (3.9) | .01 |
| Average value, % | –20.8 (4.2) | –19.8 (3.7) | –21.7 (4.5) | <.001 |
| Mid | ||||
| Anterior, % | –22.6 (3.5) | –21.3 (3.3) | –23.6 (3.4) | <.001 |
| Anteroseptal, % | –22.9 (3.1) | –21.9 (2.8) | –23.6 (3.0) | <.001 |
| Septal, % | –21.2 (3.7) | –20.4 (4.6) | –21.8 (2.7) | .002 |
| Inferior, % | –23.1 (3.3) | –22.1 (3.3) | –23.9 (3.0) | <.001 |
| Posterior, % | –20.5 (3.7) | –19.8 (3.6) | –21.1 (3.7) | .005 |
| Lateral, % | –21.2 (3.3) | –20.1 (3.2) | –22.0 (3.2) | <.001 |
| Average value, % | –21.9 (3.5) | –20.9 (4.2) | –22.7 (3.1) | <.001 |
| Apical | ||||
| Anterior, % | –23.0 (4.1) | –22.5 (4.1) | –23.4 (4.1) | .093 |
| Anteroseptal, % | –24.3 (4.9) | –23.5 (6.0) | –24.9 (3.7) | .024 |
| Inferior, % | –24.0 (3.5) | –23.5 (3.6) | –24.3 (3.4) | .062 |
| Lateral, % | –21.4 (3.6) | –20.9 (3.7) | –21.9 (3.4) | .034 |
| Average value, % | –23.1 (4.3) | –22.5 (4.8) | –23.7 (3.6) | .026 |
| Global longitudinal strain | ||||
| 2-chamber view, % | –22.4 (2.3) | –21.4 (2.2) | –23.2 (2.1) | <.001 |
| 4-chamber view, % | –21.3 (2.2) | –20.5 (2.1) | –21.8 (2.2) | <.001 |
| Long-axis view, % | –20.6 (3.8) | –19.6 (5.0) | –21.3 (2.4) | <.001 |
| Global, % | –21.5 (2.0) | –20.7 (2.0) | –22.1 (1.8) | <.001 |
Data are expressed as mean (standard deviation).
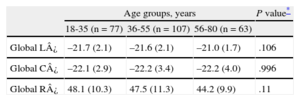
Age-related Changes in Global Longitudinal, Circumferential, and Radial Strain Values
| Age groups, years | P value* | |||
| 18-35 (n=77) | 36-55 (n=107) | 56-80 (n=63) | ||
| Global L¿ | –21.7 (2.1) | –21.6 (2.1) | –21.0 (1.7) | .106 |
| Global C¿ | –22.1 (2.9) | –22.2 (3.4) | –22.2 (4.0) | .996 |
| Global R¿ | 48.1 (10.3) | 47.5 (11.3) | 44.2 (9.9) | .11 |
C¿, circumferential strain; L¿, longitudinal strain; R¿, radial strain.
Base, mid, apical level correspond to the level of the mitral valve, the level of the papillary muscle and to the level of the apex, respectively.
Data are expressed as mean (standard deviaton).
At the segmental level, less-negative L¿ values were measured in basal segments and L¿ became more negative from base to apex (P=.009, Table 2). Among the basal LV segments, septal and anteroseptal segments showed the least negative L¿ and inferior wall showed the most negative L¿. Among LV segments at mid-ventricle, the least negative L¿ was found in the posterior wall and the most negative L¿ in the inferior and anteroseptal walls. Among the apical LV segments, the least negative L¿ was found in the lateral wall and the most negative L¿ in the anteroseptal wall.
Mean averaged L¿ at base, mid-ventricular, and apical levels were more negative in women than in men, accounting for the higher global L¿ measured in women (Table 2).
In our healthy participants, there was no significant correlation between hemodynamic parameters, such as heart rate, systolic and diastolic BP, and global L¿ values (r=0.01, P=.84; r=0.12, P=.05 and r=0.12, P=.06, respectively). However, we found a positive correlation between global L¿ values and both body mass index (r=0.25; P<.001) and body surface area (r=0.24; P<.001).
Circumferential and Radial StrainGlobal C¿ and R¿ were –22.2% (SD, 3.4%) and 46.9% (SD, 10.7%), respectively, and did not differ between men and women (–22.0% [SD, 3.4%] vs –22.3% [SD, 3.4%]; P = .526 for C¿, and 47.4% [SD, 9.2%] vs 46.7% [SD, 11.7%]; P=.655 for R¿, respectively). Accordingly, the lower limit of normality can be set at –15.4% for C¿ and 24.6% for R¿, irrespective of sex.
Similar to L¿, there were no differences in global R¿ and C¿ between the 3 age groups (for all, P=NS) (Table 3).
Left Ventricular Rotation and TwistOf the 247 enrolled participants, 194 (78.5%) had short-axis views of sufficient quality to allow measurement of LV rotation at both apical and basal levels. In each view, a minimum of 4 segments with an excellent tracking score was required to measure rotation. Feasibility (in particular, acquisition of adequate apical views) was similar in women (83%) and in men (73%) (P=.09).
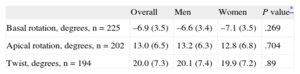
At aortic valve closure, basal rotation was –6.9° (SD, 3.5°) clockwise and apical rotation was 13.0° (SD, 6.5°) counterclockwise. There were no significant differences between men and women either at the basal or apical level (P>.05). Mean apical and basal rotations at the time of aortic valve closure in the study population are shown in Table 4.
Rotational Mechanics of the Left Ventricle and Its Comparison Between Men and Women
| Overall | Men | Women | P value* | |
| Basal rotation, degrees, n=225 | –6.9 (3.5) | –6.6 (3.4) | –7.1 (3.5) | .269 |
| Apical rotation, degrees, n=202 | 13.0 (6.5) | 13.2 (6.3) | 12.8 (6.8) | .704 |
| Twist, degrees, n=194 | 20.0 (7.3) | 20.1 (7.4) | 19.9 (7.2) | .89 |
Positive and negative values of rotation indicate counterclockwise and clockwise rotation, respectively.
Data are expressed as mean (standard deviation).
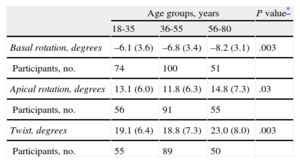
Twist increased with advancing age and was accompanied by a steady increase in basal rotation, whereas apical rotation increased after 55 years of age (Table 5). The twist and apical rotation were comparable between the groups aged 18 to 35 years and 36 years to 55 years (no significant differences), whereas they increased significantly in the group aged 56 years to 80 years (both, P<.05). Basal LV rotation was also correlated with increasing age (r=–0.23; P=.001).
Age-related Changes in Left Ventricular Rotation and Twist
| Age groups, years | P value* | |||
| 18-35 | 36-55 | 56-80 | ||
| Basal rotation, degrees | –6.1 (3.6) | –6.8 (3.4) | –8.2 (3.1) | .003 |
| Participants, no. | 74 | 100 | 51 | |
| Apical rotation, degrees | 13.1 (6.0) | 11.8 (6.3) | 14.8 (7.3) | .03 |
| Participants, no. | 56 | 91 | 55 | |
| Twist, degrees | 19.1 (6.4) | 18.8 (7.3) | 23.0 (8.0) | .003 |
| Participants, no. | 55 | 89 | 50 | |
Positive and negative values indicate counterclockwise and clockwise rotation, respectively.
Data are expressed as mean (standard deviaton).
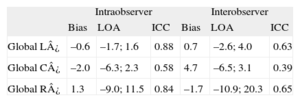
Intraobserver and interobserver reproducibility of 2-dimensional LV strain parameters are shown in Table 6.
Reproducibility of Left Ventricular Strain Parameters by Two-dimensional Echocardiography
| Intraobserver | Interobserver | |||||
| Bias | LOA | ICC | Bias | LOA | ICC | |
| Global L¿ | –0.6 | –1.7; 1.6 | 0.88 | 0.7 | –2.6; 4.0 | 0.63 |
| Global C¿ | –2.0 | –6.3; 2.3 | 0.58 | 4.7 | –6.5; 3.1 | 0.39 |
| Global R¿ | 1.3 | –9.0; 11.5 | 0.84 | –1.7 | –10.9; 20.3 | 0.65 |
C¿, circumferential strain; ICC, intraclass correlation coefficient; L¿, longitudinal strain; LOA, limits of agreement; R¿, radial strain.
Studies reporting a comprehensive assessment of LV mechanics in healthy adult participants, including data about both myocardial deformation and rotational mechanics and the impact of age and sex on these parameters, are scarce. The main results of our study can be summarized as follows: a) we provided reference values for all the main deformation components (namely L¿, C¿, and R¿) as well as LV rotational mechanics obtained from a large cohort of healthy volunteers; b) global L¿ values were significantly more negative in women than in men, accounting for the higher LVEF in women. C¿ and R¿ were similar between the sexes; c) age did not significantly affect LV myocardial deformation, and d) LV rotational mechanics is similar in men and women and increases in the later decades of life.
Reference Values for Left Ventricular Myocardial DeformationPrevious studies which have reported reference values of global L¿ included relatively small cohorts and/or enrolled patients referred to echocardiographic studies for clinical indications and subsequently found to have a normal echocardiographic study.16 Despite the recommendation that reference values for echocardiographic variables should be derived from a random sampling of healthy volunteers,22 only one study included completely healthy individuals from the community.23 The enrollment criteria of our study population differentiates the present study from most of the previous studies that have provided reference intervals for myocardial deformation parameters.
There is a lot of uncertainity about the reference values for L¿, C¿, and R¿. Marwick et al17 enrolled 242 healthy individuals without cardiovascular risk factors or a history of cardiovascular disease and found normal global LV L¿ equal to –18.6% (SD, 0.1%). Reference values for C¿ and R¿ were reported by Hurlburt et al.18 Reckefuss et al.16 demonstrated regional reference values for global L¿ and found that L¿ was lower in basal segments and showed a significant increase from base to apex. Finally, they reported a mean global L¿ of –20.6% (SD, 2.6%) in their cohort of normal probands. According to a recent meta-analysis that included 24 studies with a total of 2597 subjects (age 47 years [SD, 11 years], 51% [SD, 24%] men), normal values of global L¿ varied from –15.9% to –22.1% (mean, –19.7%), normal global C¿ varied from –20.9% to –27.8% (mean, –23.3%), and global R¿ ranged from 35.1% to 59.0% (mean, 47.3%). Additionally, they found that all directional components of strain showed heterogeneity and inconsistency between studies.23
We found more negative values of L¿ and less negative values of C¿ than reported in literature. Our R¿ data are similar to those reported in literature but there was a large inconsistency of data, resulting in a wide SD. This may be explained by technical rather than biological factors. The R¿ is a rather inaccurate measure, especially in lateral and basal segments because the distance between endocardium and epicardium is small and the spatial resolution in this tracking direction is reduced.
Effect of Age on Left Ventricular Myocardial DeformationThe effects of age on myocardial deformation remains controversial. While some studies have shown reduced ¿ values with increasing age,24,25 others have reported no change.16,26 In a very recent study, Sun et al27 reported that global L¿ became less negative with aging, while the global C¿ became more negative and the R¿ remained unchanged. Similarly, Zghal and et al28 reported that global L¿ became less negative in elderly patients but there was no significant change in global R¿ and C¿. Another study used three-dimensional magnetic resonance imaging tissue tagging and compared healthy adults by age, and reported less-negative L¿ and C¿ in the elderly, with a change that was larger at the apex than at the base.29
In our study population, which included participants between 18 years and 80 years of age, there was no correlation between age and myocardial deformation. One possible reason may be the relatively low number of elderly participants enrolled (only 34 > 60 years). However, it is not easy to find healthy participants > 60 years using our strict criteria. In addition, our results are in agreement with those of the meta-analysis by Yingchoncharoen et al,23 which failed to document a significant effect of age on global L¿.
Sex-related Differences in Left Ventricular Myocardial DeformationThe effect of sex on LV myocardial deformation remains controversial. Several studies found no difference in ¿ measurements between men and women.17,23,26,30 However, Kuznetsova et al24 reported higher R¿ in women than in men. Recently, Cheng et al31 found that, on average, L¿ was 1.7% more negative in women than in men. Hurlburt et al18 found that global L¿ and C¿ were significantly more negative in women than in men. These findings were confirmed by Reckefuss et al,16 who reported more negative L¿ in women. Finally, the HUNT-study showed that myocardial deformation was consistently higher in women, except in the group of participants > 60 years.25
In our study, we observed that women have more negative L¿ measurements, while global C¿, R¿ values and LV rotational were similar between men and women. This may account for the higher LVEF that we and others consistently found in normal women compared to normal men.32,33
Effect of Hemodynamic Factors and Body Size on Strain MeasurementsRecently published meta-analysis of 2597 subjects showed that systolic BP was associated with variation in normal global L¿ values.23 Besides systolic BP, differences in vendor and other variables such as age, sex, and body mass index were not significantly associated with the mean value of global L¿ in normal patients.23 Although this meta-analysis showed systolic BP to be an important determinant of strain, we did not confirm this finding in our study. Additionally, height, systolic BP, and heart rate did not correlate with global L¿ in a large study of healthy volunteers.17 Our study showed that body size parameters were correlated with global L¿. This finding is rather controversial in literature: a previously published report confirms this finding,34 but the recently published meta-analysis showed that body mass index was not a significant determinant for normal ranges of global L¿.23
Rotational Mechanics of the Left VentricleBoth LV rotation and torsion have been demonstrated to be important determinants of LV function.32 Apical rotation is usually greater than basal rotation and more strictly correlated with global LV function.35 Takahashi and et al15 reported normal values in different age groups. They found that basal and apical rotation were 4.9° (SD, 2.0°) and 10.1° (SD, 1.9°), respectively in 20 normal individuals between 33 years and 40 years old. Our data show higher values of LV rotation, particularly at the apex. The reasons for these differences are difficult to explain. Although we cannot exclude an ethnic factor, we think that the most likely explanation is due to the level of the LV apical short-axis view. Van Dalen et al20 have clearly shown how critical this factor is and how much the measurements can change if the view is taken just few millimeters more towards the apical or more caudal level. Unfortunately, there is no clear anatomical landmark that allows us to standardize this view. We have taken great care to obtain the most apical (just before right ventricular apex disappears) and circular view. However, the large SD in our rotational data should raise caution about the overall accuracy of our reference values. In the present study, the twist and apical rotation were comparable between the groups aged 18 years to 35 years and 36 years to 55 years. However, both of them showed significant increase in the group aged 56 years to 80 years. Likewise, Maharaj and et al36 reported that twist changed substantially after 40 years of age.
Zhang et al37 found a significantly larger apical rotation in participants aged 55 years to 65 years (9.65° [SD, 1.56°]) than in those aged 45 years to 55 years (7.94° [SD, 1.20°]). Maharaj et al36 demonstrated that apical and basal rotations and net twist increased with age. Our data are consistent with these findings. LV twisting increased with age, mostly related to the increase of LV rotation at the apex.38 This increase is most likely related to an imbalance between the subendocardial and subepicardial layers, with a greater dominance from the epicardial fibers with advancing age.38
LimitationsThere are some limitations in this study. Deformation values depend on the equipment used, suggesting that reference values may change depending on the echo machine used to acquire images and the software used to analyze them.33,39 Our data can be applied only to patients examined with the equipment employed in this study. For the future, there is hope that a standardization of strain values across different vendors will be reached.40
All participants were of European Caucasian descent. Therefore, the results of this study cannot be extended to other ethnic groups.
CONCLUSIONSWe report the comprehensive assessment of normal myocardial deformation and LV rotational mechanics in a large cohort of healthy volunteers with a wide age range. We found that women have more negative L¿ than men, which accounts for the higher LVEF in women. Moreover, age is a major determinant of rotation values in healthy participants, with an increase in apical rotation and LV twist in the elderly.
The availability of reference values for these parameters may foster their implementation in the clinical routine. According to our results, sex should be taken into consideration when evaluating the pathologic changes in myocardial function, whereas age is a significant determinant of rotational mechanics.
FUNDINGGonenc Kocabay and Sorina Mihaila are recipients of a reasearch grant funded by the European Association of Cardiovascular Imaging.
CONFLICTS OF INTERESTDenisa Muraru and Luigi P. Badano have received equipment grants and speakers’ honoraria from GE Vingmed. Luigi P. Badano is on the speakers bureau of this company.