All guidelines recommend primary percutaneous coronary intervention as the default strategy for achieving reperfusion in ST-segment elevation myocardial infarction patients. These recommendations are based upon randomized trials which compared primary percutaneous coronary intervention with stand-alone intravenous fibrinolysis. Since the time these trials were performed, however, it has been shown in further trials that use of rescue percutaneous coronary intervention in patients without signs of reperfusion after lysis, and routine coronary angiography within 24h of the administration of lysis for all other patients, substantially improved the results of intravenous fibrinolytic treatment. This has led to proposing the pharmaco-invasive strategy as an alternative to primary percutaneous coronary intervention. Actually, it is not uncommon that circumstances prevent performing primary percutaneous coronary intervention within the recommended time limits set by the guidelines. In such cases, using a pharmaco-invasive strategy may constitute a valid alternative. Both the STREAM randomized trial and real-world experience, in particular the long-term results from the FAST-MI registry, suggest that the pharmaco-invasive strategy, when used in an appropriate population, compares favorably with primary percutaneous coronary intervention. Therefore, implementing a pharmaco-invasive strategy protocol may be an important complement to compensate for potential weaknesses in ST-segment elevation myocardial infarction networks.
Keywords
Following the first randomized trials comparing intravenous fibrinolysis and primary percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI), which unequivocally favored the latter approach in terms of clinical outcomes, the use of primary PCI has grown exponentially in most countries where coronary angiography is available. Together with this increase, mortality of STEMI patients has steadily decreased, and many have suggested a direct causal relationship between these opposing trends, making the increasing use of primary PCI the main if not the only driver of improved clinical outcomes.
It must be recognized, however, that implementing primary PCI in due time remains a difficult task and, in this context, the question of whether alternative strategies should be sought in patients in whom time delays are likely to exceed the guidelines recommendations must be raised. The position of the pharmaco-invasive strategy, combining intravenous fibrinolysis followed by semi-urgent coronary angiography with possible PCI, can be addressed through a series of interrogations:
- •
Is the decrease in mortality observed in STEMI patients solely attributable to the increasing use of primary PCI?
- •
Are time delays really important?
- •
Is the pharmaco-invasive strategy superior to conventional fibrinolysis used as a stand-alone reperfusion method and how does it compare with primary PCI in randomized trials?
- •
How does the pharmaco-invasive strategy compare with primary PCI in real life?
- •
Are there specific situations where the pharmaco-invasive strategy constitutes a credible alternative to primary PCI or where it can be superior?
Many studies have documented a consistent decrease in early mortality in patients admitted for acute myocardial infarction over the past 20 years.1–3 Large administrative databases, however, cannot separate STEMI from non-STEMI. Specific studies in STEMI patients have noted similar trends, with a simultaneous increase in the use of primary PCI.4,5 Hence, many have considered that increased utilization of primary PCI was the main driver of reduced mortality.
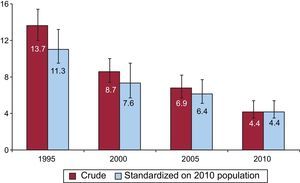
This conclusion, however, is likely to be overly simplistic. Using the French surveys of acute myocardial infarction from 1995 to 2010, we specifically analyzed the factors related to the marked mortality decrease over time (30-day mortality was 13.7% in 1995 and 4.4% in 2010).6 In fact, the overall picture of STEMI evolved considerably during this period (Table). The baseline characteristics of the STEMI population changed, with a progressive reduction in age and a concomitant decrease in associated morbid conditions. Patient behavior changed, with a much shorter time from symptom onset to first call in the more recent surveys; consequently, more patients were transported by the emergency medical system (SAMU [Service d’Aide Médicale Urgente]). Following government decisions, smaller hospitals were closed, with a resulting increase in the average number of STEMI patients treated per site; reperfusion therapy increased from 49% to 75%, mainly related to a major increase in the use of primary PCI (from 12% to 61%), while fibrinolytic therapy decreased (from 38% to 14%). Finally, major changes were also observed in terms of medications administered at the early stage (increased use of antiplatelet agents, changes in anticoagulant regimen, increased prescription of beta-blockers and angiotensin-converting enzyme inhibitors, major increase in the prescription of statins). Thus, changes in reperfusion therapy were far from the only changes observed during a period when mortality dropped by a considerable extent. By itself, the observed change in baseline characteristics of the patients accounted for about one quarter of the decrease in mortality, as evidenced by standardization of the populations in the different surveys on the risk score of the 2010 population (Figure 1). In multivariate analyses, and even after adjusting for use and type of reperfusion therapy, the risk of death at 30 days remained lower in 2010 than in 1995 (odds ratio [OR]=0.39; 95% confidence interval [95%CI], 0.29-0.53), showing that improvement in outcomes resulted from a global change involving both changes in the population's intrinsic risk and in the whole process of care at the acute stage.
Changes in Patient Baseline Characteristics, Organization of Care and Initial Management of ST-segment Elevation Myocardial Infarction Patients in the French Surveys 1995-2010
| 1995 | 2010 | |
| Age, mean (SD), y | 66 (14) | 63 (14.5) |
| Median time from onset to first call, min | Collected in 2000: 120 | 74 |
| Use of EMS, % | Collected in 2000 | |
| As first party | 23 | 49 |
| At any time | 55 | 81.5 |
| Number of STEMI patients per month per site, mean (SD) | 5.1 (3.6) | 8.7 (8.0) |
| Reperfusion therapy, % | ||
| Primary PCI | 12 | 61 |
| IV fibrinolysis | 38 | 14 |
| Antiplatelet agents, % | 92.4 | 97.4 |
| Anticoagulants, % | ||
| Unfractionated heparin | 96.4 | 44.8 |
| Low molecular weight heparin | 0 | 62.3 |
| Fondaparinux | 0 | 13.5 |
| Bivalirudine | 0 | 4.4 |
| Beta-blockers | 65.2 | 80.7 |
| ACE-inhibitors | 47.7 | 64.8 |
| Statins | 9.8 | 89.9 |
ACE, angiotensin-converting enzyme; EMS: emergency medical system; IV, intravenous; SD, standard deviation; STEMI, ST-segment elevation myocardial infarction.
Unless otherwise indicated, data are expressed as mean (standard deviation).
Evolution of 30-day mortality in the French ST-segment elevation myocardial infarction registries (1995-2010). Red bars indicate crude death rates, and blue bars indicate mortality rates standardized on the baseline characteristics of the 2010 population (ie, they indicate the mortality that would be expected for the previous years if the population had the same baseline profile as the 2010 population).
The success of reperfusion in STEMI is dependent on the time of its administration. From a practical standpoint, time-to-reperfusion can be considered the sum of time to first medical contact and time from initial medical contact to delivery of reperfusion therapy. Time from symptom onset to first call or medical contact can be influenced by public awareness campaigns. In France, such media campaigns led to a marked decrease in time to first call from 2000 (median: 114min) to 2010 (median: 74min).6 Time from contact to reperfusion will be influenced by organization of care, both on a regional scale (implementation of STEMI networks) and within PCI hospitals. In this respect, registry data show that the 30-min door-to-needle and 90-min door-to-balloon time goals are often difficult to achieve. In particular, door-to-balloon times are often much longer in clinical practice than in randomized controlled trials, as transfer of patients for PCI, local factors (weather conditions, geographic location, staff initially involved, etc.) or poor management strategies can lead to long delays. Data from the GRACE registry have shown that time-to-reperfusion did not decrease from 1999 to 2006.7 More recent data from the CathPCI registry, however, have shown a continued improvement in DB times from 2005 to 2009 (from 83min to 67min).8
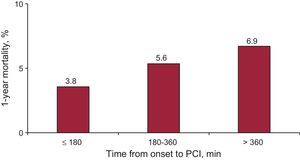
The importance of time delays before administration of reperfusion therapy is not disputed for fibrinolytic-treated patients, and the conclusions of the meta-analysis published by Boersma et al9 in 1996 remain valid: the proportional reduction in mortality was 44% in patients treated within 2h of symptom onset, compared with 20% in those treated beyond 2h. In the contemporary population of the FAST-MI 2010 registry, we still found a strong relationship between increasing time from symptom onset to primary PCI and 30-day mortality (Figure 2).
Time delays are therefore crucial to determine the best reperfusion strategy: the superiority of primary PCI over fibrinolysis is likely to exist only as far as the time to reperfusion is not exceedingly increased by opting for PCI rather than the simpler approach of intravenous fibrinolysis. From their review of the National Registry of Myocardial Infarction database, Pinto et al10 found that the equipoise between the 2 reperfusion techniques varied according to time from symptom onset, location of myocardial infarction and age of the patient. Primary PCI yielded better results than fibrinolysis when the excess time delay for delivering reperfusion therapy (PCI-related delay) did not exceed 114min on average; however, the benefit of PCI was lost when the PCI-related delay was >40min for patients <65 years of age with an anterior myocardial infarction presenting within 2h of symptom onset, while a PCI-related delay of 179min still yielded equivalent results for both reperfusion techniques in patients over 65 years of age with non-anterior myocardial infarction who were seen more than 2h of symptom onset. More recently, an analysis of mortality in STEMI patients admitted to non-PCI hospitals comparing on-site fibrinolysis versus immediate transfer for primary PCI showed that the survival advantage of primary PCI was lost when time delays to primary PCI exceeded 120min.11 Consequently, for all recent guidelines, time delays are considered central in the decision-making process.12
With the continuous decline in early mortality of STEMI patients, however, the importance of further decreasing door-to-balloon times has been challenged. Indeed, in the CathPCI registry, mortality remained unchanged from 2005 to 2009, despite a 19% decrease in door-to-balloon times.8 In this study, however, time from symptom onset to hospital admission was not considered. When we analyzed the data from the 2000-2010 French registries,13 we found a strong interaction between time to first call, increased time from call to primary PCI, and early mortality: in patients calling ≤60min from symptom onset, we observed a 2.67-fold increase in 1-year mortality for a call-to-primary PCI time >120min (95%CI, 1.43-4.97; P = .002), but the deleterious effect of delayed delivery of primary PCI gradually decreased with increasing times from onset to first call: hazard ratio (HR)=1.57 (95%CI, 0.56-4.37) for time from onset to call from 61min to 180min and HR=1.22 (95%CI, 0.55-2.57) for time to call >180min. In other words, when the patients were seen early, any time delay in delivering primary PCI resulted in a marked mortality increase; in contrast, when the patients presented late, speed of PCI delivery had little influence on mortality.
In summary, time to administration of reperfusion therapy remains a major determinant of outcomes in STEMI patients, but the impact of early delivery of reperfusion after the initial diagnosis has been made is all the more important when patients are seen early, and becomes less crucial for late presenters.
IS THE PHARMACO-INVASIVE STRATEGY SUPERIOR TO CONVENTIONAL FIBRINOLYSIS USED AS A STAND-ALONE REPERFUSION METHOD AND HOW DOES IT COMPARE WITH PRIMARY PCI IN RANDOMIZED TRIALS?The first trials to compare primary PCI and intravenous fibrinolysis invariably used fibrinolytic therapy as a stand-alone strategy, ie, very few patients treated with fibrinolytics underwent subsequent coronary angiography, potentially combined with PCI. The DANAMI 2 trial14 is a typical example, with only 15 of the 782 patients randomized to fibrinolysis undergoing rescue PCI (2%) and 16% having a PCI later during the initial hospital stay. In addition, most of these trials used in-hospital fibrinolysis, and only the CAPTIM trial compared prehospital lysis with primary PCI.15 Since then, however, several trials have demonstrated that fibrinolysis should not be used as a stand-alone treatment, but should rather be conceived as a pharmaco-invasive strategy, with the initial fibrinolytic treatment permitting early restoration of coronary blood flow in a substantial proportion of the patients, and subsequent PCI used to reopen the infarct-related artery in the case of failed fibrinolysis (rescue angioplasty), or to improve the initial result achieved and avoid subsequent reclosure of the artery.
The benefit of rescue PCI has been documented in the REACT trial,16 which tested the usefulness of emergency coronary angiography/PCI in patients in whom reperfusion failed to occur within 90min of fibrinolysis administration. Event-free survival was 85%, compared with 70% in those treated conservatively after lysis. These results supported those of the CAPTIM trial, which, though underpowered, had suggested that prehospital fibrinolytic therapy with the patients brought to PCI-capable centers, and with one third undergoing rescue angioplasty, could do at least as well as primary PCI up to 5 years after the initial episode.17
Beyond rescue PCI, the role of routine PCI within 24h of fibrinolysis was investigated in several trials, such as the GRACIA-1 trial,18 the CAPITAL-AMI trial,19 the SIAM-III20 and in the larger CARESS-in-AMI trial.21 In all instances, a strategy of routine PCI after intravenous fibrinolytic treatment yielded better results than conservative management. The most recent of these trials compared a routine PCI strategy with a postlysis strategy of fibrinolytic treatment followed by rescue PCI in case of failed reperfusion: the CARESS-in-AMI trial21 demonstrated that a strategy of immediate PCI was better than the standard of rescue-only angioplasty after fibrinolysis, with a significant and marked reduction in the primary end point of death, reinfarction, or refractory ischemia at 30 days (10.7% vs 4.4%; P = .005). Likewise, the TRANSFER-AMI trial22 enrolled 1059 patients admitted to non-PCI hospitals < 12h after acute myocardial infarction who received fibrinolytic treatment and were randomly assigned to transfer for angioplasty within 6h or to a strategy limiting emergency angiography to rescue angioplasty, associated with late elective angiography in those not needing rescue angioplasty. The pharmaco-invasive strategy did not improve 30-day mortality in comparison with the conventional strategy (4.5% vs 3.4%; P = .39), but the composite end point of death, reinfarction, recurrent ischemia, new or worsening heart failure, or cardiogenic shock was definitely improved in the pharmaco-invasive arm (17.2% vs 11.0%; relative risk=0.64; 95%CI, 0.47-0.87; P = .004). At 1 year, however, the rate of death or reinfarction was only marginally inferior in the routine angiography arm of the trial.23 Finally, the NORDISTEMI trial24 included 266 patients living in rural areas (transfer time to PCI > 90min) treated with tenecteplase, acetylsalicylic acid, enoxaparin, and clopidogrel and randomized to immediate transfer for routine PCI or PCI indicated for rescue or clinical deterioration. The primary end point of death, reinfarction, stroke, or new ischemia at 12 months was not significantly reduced with the pharmaco-invasive approach (21% vs 27%, HR=0.72; 95%CI, 0.44-1.18). The composite of death, reinfarction, or stroke at 12 months, however, was significantly lower in the pharmaco-invasive arm (6% vs 16%, HR=0.36; 95%CI, 0.16-0.81; P = .01).
A meta-analysis of these 7 trials25 showed a favorable trend for 30-day mortality (OR=0.87; 95%CI, 0.59-1.30), and stroke (OR=0.63; 95%CI, 0.31-1.26), and a significant reduction in reinfarction (OR=0.55; 95%CI, 0.36-0.82), without excess in major bleeding (OR=0.93; 95%CI, 0.67-1.31). Findings at 6-month to 12-month follow-up were similar.
Considering the more favorable results achieved with the pharmaco-invasive strategy, compared with either stand-alone fibrinolysis or fibrinolysis with rescue PCI when needed, a reappraisal of the results of earlier trials comparing primary PCI and intravenous fibrinolysis was needed.26
Two large trials, ASSENT 4-PCI27 and FINESSE28 studied the concept of facilitated PCI (ie, patients treated with emergency primary PCI, with administration of lytics during transportation). ASSENT-4 PCI showed an excess of thrombotic events with fibrinolysis-facilitated PCI (ie, when PCI was performed immediately after the delivery of fibrinolytic treatment), suggesting that, when signs of reperfusion are present, waiting for ≥3h before performing PCI in fibrinolytic-treated patients might be advisable, granting the known prothrombotic effects of fibrinolytic agents and the higher residual thrombus burden observed in lytic-facilitated PCI29. In the FINESSE trial, one-year mortality was numerically but not significantly lower in patients treated with combination therapy (half-dose reteplase and abciximab followed by urgent PCI) compared with primary PCI, suggesting a potential role for potent antiplatelet agents in this setting.30 None of these trials, however, tested the concept of a pharmaco-invasive strategy, where fibrinolytic treatment would be the first and main driver of reperfusion therapy.
The WEST study31 included 304 STEMI patients within 6h of symptom onset, randomized to 3 arms: fibrinolysis alone, pharmaco-invasive strategy, or primary PCI. There was no difference in the primary end point of the trial (a combination of death, reinfarction, refractory ischemia, congestive heart failure, cardiogenic shock, and major ventricular arrhythmia), but death or reinfarction was higher in the fibrinolysis-alone arm (13.0%) than in the primary PCI arm (4.0%), while the pharmaco-invasive arm was not statistically different from primary PCI (6.7%), suggesting that early pharmacological reperfusion with follow-up (rescue and routine) PCI within 24h yields results that might compare with those of primary PCI.
Recently, the STREAM trial assessed the results of fibrinolysis followed by early coronary angiography (3-24h) in STEMI patients presenting within 3h of symptom onset and unable to undergo primary PCI within 1 hour, compared with those of primary PCI performed beyond 1 hour (median time from randomization to arterial sheath insertion: 77min). Of the 1892 patients included in the trial, 12.4% in the pharmaco-invasive arm vs 14.3% in the primary PCI arm met the primary end point (death, reinfarction, congestive heart failure, or shock at 30 days), relative risk=0.86; 95%CI, 0.68-1.09. All-cause death was similar in both arms (4.6% vs 4.4%), but intracranial bleeding was more frequent in the fibrinolysis arm (1.0% vs 0.2%). Because of the initial excess in intracranial bleeding in elderly patients, the protocol was amended after about one quarter of the patients had been randomized, and the dose of tenecteplase was reduced by half in elderly patients (≥75 years of age); the difference in intracranial bleeding between the 2 groups was no longer significant after the protocol had been amended: 0.5% vs 0.3%). The 1-year results of the trial have been presented during the 2013 scientific sessions of the American Heart Association; they showed a similar cardiac mortality in both arms.
Overall, 2 conclusions can be drawn:
- •
The results of randomized trials comparing primary PCI with stand-alone fibrinolysis should no longer be considered a valid reference in the contemporary era, because of the way fibrinolytic treatment should be used, but also because of increased operator/center experience in primary PCI (including its pharmacological environment).
- •
A pharmaco-invasive strategy, such as used in the contemporary period, is likely to give clinical results up to 1 year equivalent to those of primary PCI, at least when PCI cannot be performed within 1h of the qualifying electrocardiogram, in patients seen early after symptoms onset.
Only limited information is available regarding the compared results of a pharmaco-invasive strategy or primary PCI, such as used in the real world. Probably the most comprehensive data come from the French registries, in particular, the FAST-MI 2005 registry.32
The French organization of care for STEMI patients largely relies on a widely deployed network of emergency medical system ambulances, with emergency physicians on board (SAMU). The SAMU system is based upon a unique, nationwide, call number. There is one SAMU medical call center for each French administrative region (département), which decides whether or not to dispatch one of several mobile intensive care units that can provide critical care in the field and during transport. By French law, each mobile intensive care unit team must include a physician, usually an anesthesiologist or emergency physician, a nurse, and a driver trained as an emergency medical technician. Management on scene by the mobile intensive care unit team and precise notification of the patient status to the “receiving” medical center allow direct admission to the most appropriate setting, and in particular direct admission to the catheterization laboratory. Emergency physicians can also deliver intravenous fibrinolysis on site. In spite of this organization, only about half of the STEMI patients actually use the SAMU directly, and median time from first call to primary PCI (including an average 20-min time delay for the mobile intensive care units to get to the site) was still 150min in 2005. This explains why fibrinolysis is still used in France, and is usually delivered in the prehospital setting.
From a historical perspective, the concept of a pharmaco-invasive strategy has been preceded by repeated assessments of the results of prehospital fibrinolysis. In 2000 in France, fibrinolytic treatment was administered in the ambulance in two thirds of the patients, 24% had rescue PCI after lysis, and 60% had a PCI procedure during the initial hospital admission. Compared with patients treated with primary PCI, those receiving prehospital fibrinolysis showed a strong trend to decreased 1-year mortality (HR=0.52; 95%CI, 0.25-1.08; P = .08).33,34 The satisfactory results of prehospital fibrinolysis when used in a timely fashion in physician-staffed ambulances are confirmed by the German data from the PREMIR registry,35 showing that in-hospital mortality was not different from that of primary PCI. Similar findings have been reported from the Polish Wielkopolska registry, in which thrombolytic treatment with tissue plasminogen activator followed by PCI in 26% of the patients provided results that compared with those of primary PCI in patients with onset of chest pain within <4h.36
Although not strictly speaking “pre-hospital” fibrinolysis, intravenous fibrinolytic treatment has been used at primary care centers, before transferring the patients to tertiary hospitals. This organization of care has been used in several areas in the United States of America to overcome the difficulty related to the long distances that separate many patients from PCI centers capable of providing emergency interventions during 24 h per day and 7 days per week (24/7). Very encouraging results have been reported from a regional set-up to provide optimal care for STEMI patients, wherever the myocardial infarction occurs. The Minnesota regional system of care37 designed specific therapeutic protocols for patients with STEMI presenting to hospitals far from the main PCI center; patients presenting at hospitals 60 miles from the tertiary center (zone 1) were directly transferred to the catheterization laboratory of the tertiary center; patients presenting at hospitals 60 to 210 miles from the tertiary center (zone 2) received half-dose tenecteplase en route to the PCI center. Personnel at the primary care hospitals had specific training for managing patients with acute chest pain, and electrocardiograms were faxed to the PCI center before transfer. In the case of inclement weather or other anticipated delays, patients from zone 1 could receive half-dose tenecteplase, and those from zone 2 received full-dose lytics. Thirty-day mortality was similar in patients presenting directly at the tertiary center (4.4%) and in those from zone 1 (4.7%) and zone 2 (5.2%). A similar experience was reported with the Mayo Clinic STEMI protocol.38 A network was organized between a tertiary hospital with 24/7 PCI capability and primary care institutions located in a radius within which the maximum transfer time did not exceed 90min. The primary reperfusion strategy at local hospitals was full-dose fibrinolysis in patients presenting within 3h of symptom onset and primary PCI in those presenting beyond 3h. For primary PCI, the emergency department at the tertiary hospital was bypassed in order to avoid losing time. Patients with fibrinolysis were evaluated by a cardiologist upon arrival, those without signs of reperfusion underwent immediate rescue PCI, and coronary angiography was performed on a routine basis in all other patients 24-48h later. In-hospital mortality was 6.6% in patients admitted directly to the tertiary center, 5.7% in those admitted to regional centers and treated with primary PCI, and 3.1% in those admitted to regional centers and treated with fibrinolysis. Similar efforts have been made in North Carolina and have led to marked reductions in times-to-reperfusion in patients initially admitted to primary care hospitals; in spite of these improvements, however, no further reduction in early mortality, compared with historic controls, was observed.39
From prehospital fibrinolysis, practice evolved towards an integrated pharmaco-invasive approach. Perhaps the first reported example is the Israeli experience from the city of Haifa, which documented very favorable results with wide use of intravenous fibrinolysis followed by an aggressive policy of rescue PCI and early intervention.40 In this registry, 25% of the patients treated with fibrinolysis had rescue PCI, 92% underwent coronary angiography during the same hospitalization, with 79% undergoing PCI. Thirty-day mortality was 4.7% and 1-year mortality was 6.7%. Of note, mortality was lower in the patients receiving fibrinolysis within 150min of symptom onset, and in those undergoing subsequent PCI. Likewise, in 2005, common practice for fibrinolytic-treated patients in France had evolved towards an integrated pharmaco-invasive strategy.32 Of the patients treated with intravenous fibrinolysis, 96% underwent coronary angiography and 84% underwent a PCI procedure (within 24h of lytic administration in 57%). In-hospital mortality was 4.3% for fibrinolysis and 5.0% for primary PCI. In patients receiving fibrinolysis, 30-day mortality was 9.2% when PCI was not used and 3.9% when PCI was subsequently performed. One-year survival was 94% for fibrinolysis and 92% for primary PCI (P = .31); after propensity score matching, 1-year survival was 94% and 93%, respectively.
Overall, all of these data suggest that, as used in routine clinical practice, a pharmaco-invasive strategy is likely to give results that compare favorably with those of primary PCI.
ARE THERE SPECIFIC SITUATIONS WHERE THE PHARMACO-INVASIVE STRATEGY CONSTITUTES A CREDIBLE ALTERNATIVE TO PRIMARY PCI OR WHERE IT CAN BE SUPERIOR?There is little question that primary PCI, performed within the recommended timelines, should constitute the default strategy for STEMI patients, as it offers the best chance to reopen the culprit vessel, without increasing the risk of hemorrhagic stroke. The pharmaco-invasive strategy, however, can constitute a valid alternative when patients are seen early after the onset of symptoms and when the time to primary PCI is likely to exceed the limits suggested in the guidelines. Both conditions are necessary to give a fibrinolytic strategy the best opportunity to achieve superior results. A short delay from symptom onset will increase the efficacy of fibrinolytic treatment and its capacity to reopen the culprit artery. Also, as we have observed in the FAST-MI registry, the impact of a longer first contact-to-balloon time is inversely related with the time from symptom onset: the shorter the time from onset of symptoms, the greater is the necessity to shorten the time delay to primary PCI. Therefore, the pharmaco-invasive strategy is likely to be a winner (in the absence of specific contraindications) when patients present within 2h of symptom onset, and when the time from the qualifying electrocardiogram to primary PCI is likely to be > 90min. These theoretical consideations are supported by a recent analysis of the 5-year follow-up results from FAST-MI 2005, comparing the pharmaco-invasive strategy with primary PCI in patients having called within the first 12h from symptom onset. Crude 5-year survival was 88% for the fibrinolytic-based strategy, and 83% for primary PCI, compared with 59% for patients who got no reperfusion therapy. Adjusted HRs (95%CI) for 5-year death were: HR=0.73 (IC95%, 0.50-1.06) for fibrinolysis vs primary PCI, HR=0.57 (IC95%, 0.36-0.88) for prehospital fibrinolysis vs primary PCI, and HR=0.63 (IC95%, 0.34-0.91) for fibrinolysis vs primary PCI performed beyond 90min of the call in early presenters having called within the first 180min from symptom onset. In propensity-score-matched populations, however, survival rates were not significantly different for fibrinolysis and primary PCI, both in the whole population (88% for fibrinolysis, 85% for primary PCI), and in the population seen early (87% for fibrinolysis, 85% for primary PCI beyond 90min of call).41 Left ventricular ejection fraction was also significantly (although modestly) higher in the patients receiving a pharmaco-invasive approach.
CONCLUSIONSIn summary, on a worldwide scale, implementation of a tight network of highly experienced, 24/7 PCI-capable STEMI centers is not realistic. In many places, an experienced PCI center is too far away to offer primary PCI within the recommended time limits. In such circumstances, and particularly when patients present early after the onset of symptoms, a pharmaco-invasive strategy represents a valid alternative to delayed primary PCI. From a public health standpoint, one of the most rewarding strategies would be to implement public information campaigns designed to make the public aware of the importance of calling early in cases of persistent chest pain potentially suggestive of myocardial infarction. With an increasing proportion of early presenters, the pharmaco-invasive strategy could be an alternative to primary PCI in a substantial number of patients.
CONFLICTS OF INTERESTN. Danchin has received speaking fees from Boehringer-Ingelheim.
Section sponsored by Laboratory AstraZeneca