Keywords
INTRODUCTION
The objective of revascularization surgery is to re-establish blood flow in occluded or stenotic coronary arteries. In many cases, this treatment is not a permanent solution: up to 10% of implanted grafts become occluded immediately or shortly after surgery, and 59% of venous grafts and 27% of arterial grafts are occluded at 10 years.1 At 6 years following surgery, angina reappears in 50% of patients.2,3 These symptoms can be the result of graft failure, but in most patients, the cause is disease progression in native arteries.4
Coronary angiography (CA) is the diagnostic method of choice for assessing the status of coronary grafts. It is, however, an invasive, expensive technique with associated complications, which are uncommon, but sometimes serious.
Noninvasive tests, such as echocardiography and nuclear imaging, are useful for detecting myocardial ischemia, but they are limited for determining the precise location of obstructive disease in a revascularized patient. Because of this limitation, other imaging techniques have been evaluated for noninvasive angiographic assessment of surgical revascularization, such as magnetic resonance imaging,5,6 conventional computed tomography (CT),7 electron beam CT,8 and multi-detector CT (MDCT).9 Specifically, MDCT has shown elevated diagnostic accuracy in the detection of occlusion and stenosis in coronary grafts. Nonetheless, only a small number of studies have investigated its performance in native arteries,10-15 and this has limited its routine clinical application in this setting. Only one previous study in Spain, also performed by our group, has evaluated the diagnostic performance of CT in surgically revascularized patients, although again, only grafts were analyzed, not native vessels, because of the limitations of the earlier, 16-detector CT system used in the study.16
The aim of the present study was to determine the diagnostic accuracy of MDCT for assessing coronary grafts, as well as the vessels distal to the anastomosis and the native coronary vessels, and to compare the results with those of invasive coronary angiography.
METHODS
Population
A prospective study was carried out in 36 patients (30 men) with a mean age of 65.7 (10.1) years (range, 41-81), who had undergone surgical revascularization. All patients had a clinical indication for angiographic evaluation of the grafts to investigate recurrent ischemic symptoms (26 patients, 72.2%) or deteriorated systolic function (10 patients, 27.8%).
All patients except 4 (11.1%) were in sinus rhythm, and the mean heart rate was 61.07 (8.8) bpm (range, 46-72). Patients who had renal failure or allergy to iodinated contrast agents were excluded, as were those who failed to achieve adequate breath-holding (Table 1).
Coronary angiography and MDCT studies were carried out in all patients, with an interval between the studies of 48.63 (40.02) days (range, 2-170). In all patients, MDCT was carried out before CA and the delay in performing CA was decided by the attending physician.
All patients gave informed consent to participate in the study.
Multidetector Computed Tomography Angiography
The study was performed using a 64-detector CT unit with a complete rotation time of 330 ms (LightSpeed VCT, GE; Milwaukee, Wisconsin, United States) that can obtain 64 slices with a thickness of 0.625 mm and coverage of 40 mm per rotation. This enables acquisition of a volume including the entire thorax in a mean breath-hold time of 10.1 (1.9) seconds (range, 7-14).
The volume of contrast agent administered (Iomeron 400; Bracco, Italy) was adapted to the patient's weight, and contrast was injected in an antecubital vein at an infusion speed of 5 mL/s. Image acquisition started when the contrast reached the ascending aorta.
Image acquisition was performed at 120 kV and up to 750 mA and was synchronized with the electrocardiogram (ECG). ECG-pulsed tube current modulation was used to reduce radiation dose. The estimated mean radiation dose was 30 mSv (range, 24-32), applying the conversion coefficient for the chest (´0.017).
Even though most of the patients studied were receiving treatment with beta-blockers, an additional 2.5 to 5-mg dose of intravenous atenolol was given to 7 patients whose heart rate was >60 bpm before the test (Table 1).
Following image acquisition, the phases of the cardiac cycle were retrospectively reconstructed (from 0% to 90%, with successive 10% increases) using a segmental reconstruction algorithm (temporal resolution, 165 ms), in order to obtain reconstructions in the cardiac phase with minimal heart motion artifact, particularly for the study of native coronary vessels.
Image analysis was performed on a workstation (Advantage Work Station 4.3, General Electric Medical System; Milwaukee, Wisconsin, United States) using dedicated software for cardiovascular studies. Curved multiplanar reformatted (MPR), maximum intensity projection (MIP), and 3D volume rendering (3D-VR) reconstructions were performed. All imaging studies were interpreted by a cardiologist with experience in the assessment of cardiovascular studies by CT, blinded to the conventional angiography findings.
Arterial and Venous Grafts
The patency of the grafts and presence of significant stenosis (>50% reduction in graft diameter at any point along its length by visual estimation) were evaluated. A total of 103 coronary grafts were evaluated, which, according to the operative records, included 49 arterial grafts (32 left mammary artery, 2 right mammary, and 15 radial grafts) and 54 venous grafts.
Vessel Distal to the Bypass Anastomosis
All vessel segments distal to the anastomosis were evaluated for the presence of significant stenosis (>50% reduction in lumen diameter) and occlusion.
Native Coronary Arteries
Nonrevascularized coronary arteries and those with incomplete revascularization were assessed by segments, following the 17-segment American College of Cardiology/American Heart Association (ACC/AHA) model.17 The following coronary artery segments were evaluated: proximal, middle, and distal right coronary artery; interventricular/ posterior descending artery and posterolateral branch; left main coronary artery; proximal, middle, and distal left anterior descending artery; first and second diagonal branches; and proximal and distal circumflex artery with 3 obtuse marginal and/or posterolateral branches (as well as the posterior descending branch in cases of left dominance).
Invasive Coronary Angiography
Coronary angiography with standard angiographic views was carried out on a Coroskop Plus/TOP system (Siemens, Munich, Germany) with femoral artery puncture and, whenever possible, selective catheterization of the coronary grafts. The interventional cardiologist in charge of the procedure performed the image analysis, consisting of visual determination of the presence of lesions within the vessels, in the same way as was done with MDCT.
Statistical Analysis
In the descriptive analysis of the sample, the continuous variables are expressed as the mean (standard deviation), whereas the qualitative variables are expressed as percentages.
To determine the diagnostic accuracy of MDCT for noninvasive assessment of significant lesions (>50% stenosis or occlusion) over the entire length of the aortocoronary grafts, distal beds, and native coronary vessels, we calculated the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and diagnostic accuracy of the method. These values were calculated using a 2´2 contingency table, taking conventional CA as the reference standard. The diagnostic values were calculated for the total of aortocoronary grafts, and separately for venous and arterial grafts, for vessels distal to the anastomosis, and for segments of native coronary vessels. In addition, an analysis by patient was carried out for grafts, native vessels, native vessels distal to the anastomosis, and for the combination of grafts and native vessels together. In this analysis, patients with at least 1 stenotic graft or native artery and those who presented nonassessable segments were classified as positive (because the presence of lesions could not be ruled out and the need for coronary angiography persisted). The 95% confidence interval (CI) was determined for the diagnostic variables. Statistical analyses were carried out with SPSS version 12.0 for Windows (SPSS Inc., Chicago, Illinois, United States).
RESULTS
Aortocoronary Grafts
Of the 103 aortocoronary grafts referred to in the surgery report, 96 (93.2%) were visualized by CA, by both selective and indirect injection; 48 were arterial grafts and 48, venous grafts. Twenty-four occlusions were identified (4 in internal mammary artery grafts, 5 in radial artery grafts, and 15 in venous grafts) and 6 cases of stenosis >50% (1 in an internal mammary graft, another in a radial graft, and 4 in saphenous vein grafts).
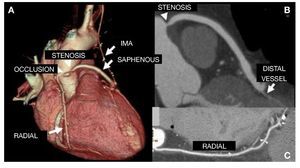
With the use of MDCT, 98 grafts were visualized, 48 arterial and 50 venous grafts. Twenty-six occlusions were detected (4 in internal mammary grafts, 5 in radial grafts, and 17 in saphenous grafts) and 8 significant stenoses (1 in mammary, 3 in radial, and 4 venous) (Figure 1). MDCT enabled detection of 2 saphenous graft occlusions at their origin (stump), that could not be assessed on invasive CA. To determine the diagnostic capability of MDCT for noninvasive evaluation of significant lesions (occlusion or >50% stenosis) in aortocoronary grafts, a comparison was performed in the 96 grafts (48 arterial and 48 venous) visualized on angiography (Table 2).
Figure 1. A: volume-rendering reconstruction.Internal mammary graft to the left anterior descending artery, saphenous graft to the marginal artery, and radial graft to the right coronary, all patent. Significant stenosis in the proximal segment of the saphenous graft to marginal branch and occlusion of the saphenous graft to diagonal artery (arrowheads). B and C: curved multiplanar reconstruction shows proximal stenosis of the saphenous graft to marginal branch, causing a considerably reduced diameter (B); the radial graft to distal right coronary shows no lesions. IMA indicates internal mammary artery.
The diagnostic performance of MDCT in venous grafts showed a sensitivity of 100% (19 significant lesions detected by MDCT of the 19 by conventional angiography), a specificity of 100% (29 lesion-free grafts by MDCT of the 29 grafts by CA), and a PPV and NPV of 100% (Table 3).
With regard to the comparison in arterial grafts, 11 significant lesions were diagnosed by CA and all were detected with MDCT (sensitivity, 100%). There were 2 false positives: two non-significant stenoses in a radial artery graft to the right coronary artery and another to a marginal artery with several metal clips, which were considered significant on MDCT findings (Figure 2). There were no false negatives. The specificity, PPV, and NPV obtained were 94.6% (35/37), 84.6% (11/13), and 100% (35/35), respectively (Table 3).
Figure 2. A: volume-rendering reconstruction. Internal mammary artery graft to left anterior descending artery and a radial artery Y-graft to the posterolateral branch of the circumflex artery with metal artifacts and a reduced diameter, without visualization of the distal anastomosis in the multiplanar reconstruction (B); the radial graft was therefore considered occluded. Conventional angiography of the graft showed that it was patent. IMA indicates internal mammary artery.
The overall sensitivity and specificity of MDCT in the detection of significant coronary graft lesions was 100% (30 lesions correctly diagnosed by MDCT of the 30 visualized on CA study) and 96.9% (64/66; 95% CI, 92.1-100), respectively. The overall PPV was 93.8% (95% CI, 87-100) and the NPV was 100%. The diagnostic accuracy of MDCT for noninvasive assessment of the total of aortocoronary grafts was 97.9% (94 of the 96 grafts compared were correctly evaluated by MDCT; 95% CI, 95-100) (Table 3).
Native Coronary Arteries
A total of 174 nonrevascularized native coronary arteries or incompletely revascularized arteries (the equivalent of 275 segments) were evaluated. Of the 275 segments, 262 (95.3%) were visualized by CA; 46 of them (16.7%) presented significant stenosis/ occlusion and 212 (77.1%), nonsignificant stenosis. Four segments with stents (1.5%) were visualized. The 13 segments that were not visualized included the first and second marginal arteries (2 and 4, respectively), middle right coronary artery, distal right coronary, posterolateral branch, and posterior interventricular artery (4).
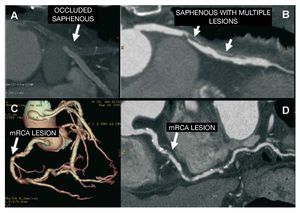
By MDCT, 248 segments were visualized (90.2%). Among them, 43 (15.6%) segments presented occlusion or lesions considered significant (Figure 3), 201 (73.1%) showed nonsignificant stenosis, and 4 (1.5%) had stents. The 3 lesions that were considered significant on conventional coronary angiography but not on CT included 1 lesion that was evaluated as nonsignificant according to CT findings and 2 native vessels that could not be assessed by CT because of motion artifacts. Twenty-seven segments could not be evaluated by MDCT (distal circumflex, 3; first marginal, 2; second marginal, 8; middle right coronary, 1; distal right coronary, 1; posterolateral branch, 3; and posterior interventricular, 9).
Figure 3. A and B: curved multiplanar reconstruction shows completely thrombosed, occluded saphenous graft (A) and another saphenous graft with multiple lesions; the proximal lesion is significant (B). C and D: triple bypass of mammary artery graft to the left anterior descending artery, saphenous to the diagonal, and saphenous to the posterolateral branch of the circumflex. Volume-rendering reconstruction (C) shows patency of the grafts and a lesion in the middle segment of the unrevascularized right coronary artery, seen to be significant in the multiplanar reconstruction (D). mRCA indicates middle right coronary artery.
To determine the diagnostic performance of MDCT for noninvasive assessment of significant lesions (occlusion or >50% stenosis) in nonrevascularized native vessels, the results for 258 segments of the 262 visualized by CA were compared (the 4 segments with stents were excluded).
The diagnostic values for native vessels showed a sensitivity of 93.5% (43/46), specificity 94.8% (201/212), PPV 79.6% (95% CI, 74.7-84.5), and NPV 98.5% (95% CI, 97-99.9) (Table 3).
The diagnostic accuracy of MDCT for noninvasive evaluation of all native segments was 94.6% (244/258; 95% CI, 91.8-97.3) (Table 3).
Vessels Distal to the Anastomosis
A total of 99 vessels distal to the aortocoronary anastomosis were visualized (35 left anterior descending artery, 14 diagonal, 2 circumflex, 23 marginal, and 25 right coronary).
To determine the diagnostic performance of MDCT for noninvasive assessment of significant lesions (occlusion or >50% stenosis) in vessels distal to the anastomosis, the findings in the 95 vessels out of 99 visualized with CA were compared (4 small-diameter vessels with extensive calcification were not assessed).
The diagnostic values for distal vessels showed a sensitivity of 85.7% (6 vessels with significant stenosis on MDCT of the 7 detected on angiography), a specificity of 96.6% (88 vessels without lesions compared to 85 considered lesion-free by angiography), PPV 66.7%, and NPV 98.8% (Table 3).
The diagnostic accuracy of MDCT for noninvasive assessment of all native distal segments was 95.8% (91 of 95 vessels distal to the anastomosis compared were correctly evaluated by MDCT; 95% CI, 91.7-99.8) (Table 3).
Per-patient analysis
The 20 patients with at least 1 graft with lesions on coronary angiography were correctly classified by MDCT, 3 patients without lesions on angiography were erroneously classified by MDCT, and in 13 patients, MDCT correctly excluded the presence of lesions in the grafts. The diagnostic accuracy to identify or exclude graft disease was 92% (33/36). MDCT also showed high diagnostic precision in the analysis of native coronary vessels and distal vessels, with values of 92% and 94%, respectively. The diagnostic value of the test for correct analysis of lesions in any vessel was high. Following our analysis, the diagnostic accuracy obtained was 91.6% (Table 4).
DISCUSSION
In selected patients, CT and particularly MDCT have shown high diagnostic precision in the evaluation of aortocoronary grafts, with values even higher than those recorded for detection of lesions in native coronary vessels.9-16,18-23 This high performance is mainly attributable to the fact that grafts are less mobile and relatively large (especially true for venous grafts). Nonetheless, there remains some difficulty related to the presence of metal clips in arterial grafts, which are also smaller in size. To determine the utility of MDCT in these patients, however, an evaluation of the native coronary vessels is also needed, and in this case, the task is more difficult due to the poor quality of these vessels in patients with advanced atherosclerosis.
Previous studies using 16-detector scanners have reported high diagnostic accuracy in the assessment of graft patency, with a sensitivity of 100% and a specificity of 98% to 100%, although the reported values are somewhat lower for detection of stenosis (sensitivity, 71%-100%; specificity, 86%-100%).16-19 However, the small number of studies that also assessed native coronary vessels have described a high percentage of nonassessable segments (24%-34%) because of motion artifacts and particularly, the presence of calcifications.10-15
In the existing series examined with 64-detector CT, an increase in the percentage of assessable segments with respect to the earlier studies is reported because of improvements in the quality of the images. Moreover, high diagnostic accuracy is maintained, with values of 100% for detecting occlusion and nearly 100% for stenosis,10,11,13-15,20-23 results that are similar to those obtained in our study (sensitivity and specificity of 100% and 97%, respectively).
There are few studies in which MDCT is used to additionally assess native vessels in the same examination.10-15 In a study by Malagutti et al10 performed with a 64-detector CT unit, the authors reported a sensitivity of 89% and specificity of 93% for the detection of significant stenosis in coronary segments distal to the anastomosis, and a sensitivity of 97% and specificity of 86% in nonrevascularized segments. The study by Ropers et al13 showed a sensitivity and specificity of 86% and 90%, respectively, for assessing coronary segments distal to the anastomosis, and 86% and 76%, respectively, for nonrevascularized segments (coronary segments >1.5 mm), with 7% of nonassessable segments, mainly due to extensive calcification. In another study using 64-detector CT in 749 native segments, Onuma et al11 reported an assessability of 91.4%, with a sensitivity and specificity of 93.3% and 87.6%, respectively. In the evaluation of distal vessels, the observed sensitivity was 70% and specificity 91%.
In our series, 93% of native segments were assessable, and the diagnostic accuracy of the technique (sensitivity, 93.5%; specificity, 100%) was similar to the values reported in previous studies. With regard to distal vessels, we obtained a sensitivity of 85.7% and a specificity of 96.6%, similar to previously described results (Table 5) and lower than those obtained when only native coronary vessels are evaluated in nonrevascularized patients. These results confirm the high diagnostic accuracy of MDCT in the assessment of coronary grafts.
The greatest difficulty for MDCT resides in the evaluation of native vessels, in which progression of coronary disease often leads to reappearance of the symptoms. This difficulty stems from the spatial resolution used in current CT studies, which limits assessment of the native vessels (nonrevascularized and distal to the anastomosis) of patients such as these, with advanced atherosclerosis, small-diameter vessels, extensive calcification, and sometimes, with stents.
Nonetheless, in our series, MDCT enabled complete assessment of the grafts and native coronary vasculature in 25 of the 36 patients, and in 23 of them, at least 1 significant lesion was identified.
It would be desirable that further technological development related to the detectors could elude the limitations in the analysis of native vessels due to insufficient spatial resolution, thereby averting the need for invasive CA in a larger number of patients.
Limitations
Although the same number of arterial and venous grafts was included in our study, less than a third of the arterial grafts were from the radial artery, and these tend to be more difficult to evaluate because of their small size and the more frequent presence of metal clips.
The CT radiation dose was higher than what would have been used if the examination had been limited to assessment of the coronary vasculature because of the larger volume acquired (approximately twice the volume of a conventional cardiac study). Despite the use of radiation dose modulation, doses continued to be high, although with the currently available acquisition protocols and the new CT scanners, a considerable reduction is attained. The risk of developing cancer increases with the radiation dose, but it decreases significantly with age, and in patients older than 65 years, such as those in our series, the risk is small. Nonetheless, it is desirable to expose the patient to less radiation.24
The study was performed in the setting of daily clinical practice and only 1 observer was available for both the CT examinations and catheterization. Thus, the between-observer variability was not determined. In addition, only a semiquantitative (visual) study of the lesions was carried out, because there are currently no precise tools to perform a quantitative evaluation in the specific case of MDCT. For the same reason and in contrast to conventional angiography, it was not possible to reliably establish more precise differences related to the severity of the lesions (<50%, 50%-75%, and >75%), even assuming that the pathophysiological repercussions might differ.
Another known limitation of CT images is that it is not possible to differentiate between partial occlusion and short, complete occlusion in which there is good collateral flow. Although the related therapeutic implications are different, this limitation did not affect the analysis of the study, in which both types of lesions were considered significant stenosis.
CONCLUSIONS
Multidetector CT is useful in the evaluation of grafts in revascularized patients with a repeat onset of symptoms and may be a useful alternative to invasive angiography when there is little or no information on the previous surgery. The assessment of revascularized patients should include an analysis of the native coronary arteries, poses the greatest challenge for this diagnostic imaging technique. Notwithstanding, as our results have shown, the NPV remains high with the use of MDCT; therefore, the technique can be considered useful for excluding significant stenosis in distal vessels and nonrevascularized native vessels. However, the PPV is lower (66.7%), a fact that advises caution in the identification of significant stenosis in vessels having a small diameter or calcifications.
ABBREVIATIONS
CA: coronary angiography
CI: confidence interval
CT: computed tomography
MDCT: multidetector computed tomography
NPV: negative predictive value
PPV: positive predictive value
Correspondence: Dr. F. Ridocci Soriano.
Servicio de Cardiología. Hospital General Universitario de Valencia. Avda. Tres Cruces, 2. 46014 Valencia. Spain.
E-mail: ridocci_fra@gva.es
Received October 17, 2008.
Accepted for publication October 15, 2009.