Keywords
INTRODUCTION
Catheter ablation has become the first treatment of choice for most tachycardias, with excellent outcomes and minimal complication rates.1-5 However, use of this therapy is often limited in elderly patients, as it is an invasive procedure with a slightly higher risk of complications due to the more limited resistance of these patients compared to younger ones. In addition, concurrent diseases often encountered in such patients are considered as a factor that could disproportionately increase the risk of the procedure. It is likely that, for these reasons, catheter ablation is less widely indicated in elderly patients. However, the few clinical studies on catheter ablation in elderly patients have shown similar outcomes to those reported for younger patients, both in terms of efficacy and safety.6-9 An example of this is catheter ablation for ventricular tachycardia (VT) in patients with structural heart disease. The efficacy and safety have not been established in elderly patients, given that the series published to date of the general population have included very few elderly people. This treatment would, however, be particularly appropriate in this population, whose concurrent diseases and short life expectancy mean that the use of other much more expensive and invasive therapeutic alternatives, such as implantable cardioverter-defibrillators (ICDs), is questioned.
The objectives of the study were: a) determine the efficacy and complications of catheter ablation of VT in elderly patients (age ≥75 years) with structural heart disease, and b) evaluate medium- and long-term outcomes.
METHODS
Patients
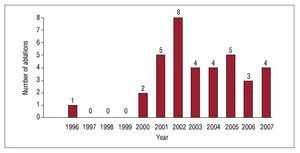
The study included 33 consecutive patients aged over 75 years with structural heart disease who underwent catheter ablation of VT between March 1996 and November 2007. The annual distribution of ablation procedures of the study is shown in Figure 1. The mean age was 79.8 (3.3) years (range, 75.1-88.1 years); 29 patients were men (89.7%) and 4 were women (10.3%). All patients had structural heart disease, which was of ischemic origin in 27 (81.8%) and idiopathic dilated cardiomyopathy in 6 (18.2%). The left ventricular ejection fraction (LVEF) was 35.9% (8.9%) (range, 25%-55%). The baseline characteristics of the patients are shown in the Table.
Figure 1. Annual change in the number of ablations in patients aged over 75 years in our hospital.
Catheterization Study and Ablation
Diagnostic catheterization and initial mapping were done during the same session as the ablation procedure in all patients. For the procedures, patients were in a fasting state and all antiarrhythmic medication had been suspended at least 5 half-lives earlier. Mild sedation was applied with midazolam and morphine hydrochloride. Eighteen patients had received prior treatment with an antiarrhythmic drug (7 with amiodarone, 9 with procainamide, 1 with b-blockers, and 1 with lidocaine) and in 6 patients, 2 antiarrhythmic drugs had been administered before opting for catheter ablation as a therapeutic option.
Two or 3 multipolar catheters were introduced percutaneously via the femoral veins, and placed under fluoroscopic control in the right atrium and para-Hisian region. One or both anterior catheters were then displaced to the apex of the right ventricle and the right ventricular outflow tract when pacing was required at this site. After the initial catheterization study and induction and characterization of the VT, more exact endocardial mapping was undertaken with a guided exploratory catheter. This catheter was introduced into the left ventricle in all patients via a femoral artery. In 2 patients, ablation was done epicardially.
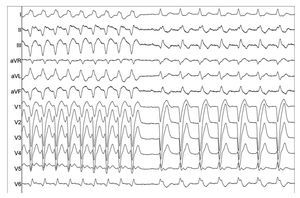
Conventional surface electrocardiographic leads were recorded, as well as 6 to 9 intracardiac bipolar leads filtered between 30 and 500 Hz using a digital polygraph. The site of radiofrequency discharge was controlled by mapping of activation and channeling. Ablation was effected by radiofrequency discharge between the distal electrode of the exploratory catheter and a patch electrode on the back of the patient. For 30 to 60 seconds, a temperature-controlled radiofrequency current was applied, with limits set at 50 W and 70ºC. Ablation of the VT was considered to be successful when this was abolished during radiofrequency application and it was not possible to reinduce it (Figure 2). For the purposes of efficacy of the procedure, only abolition of clinically documented VT was considered, without including persistence of inducibility of other nonclinical VTs.
Figure 2. Suppression of ventricular tachycardia in an elderly patient with ischemic heart disease by radiofrequency application.
Follow-up
After ablation, all patients remained under observation in hospital for at least 24 hours. The patients in whom it had been possible to abolish the clinical VT were discharged without any antiarrhythmic therapy. Patients attended an outpatient follow-up visit 6 months after the procedure. Subsequent follow-up visits depended on the clinical outcome. Attempts were made to obtain a final follow-up with all patients by means of telephone contact at the end of the study.
Statistical Analysis
For the descriptive analysis, quantitative variables were expressed as mean (SD) and compared using the Student t test, after prior study for homogeneity of variance. Those variables that did not follow a normal distribution were expressed as medians [interquartile range] and compared using the Mann-Whitney U test. Qualitative variables were expressed as absolute number and percentage and compared with the Fisher test or c2 test. Statistical significance was established at P<.05.
A Kaplan-Meier survival analysis was subsequently undertaken after discharge from hospital and the quality of life of the patients during follow-up was assessed.
Data were analyzed with the SPSS program (version 15.0 for Windows).
RESULTS
Ablation of clinical VT was successful in 28 patients (84.8%); no significant differences in efficacy were found between patients with postinfarction scarring (88.9%) and those with dilated cardiomyopathy (DCM) (66.7%) (P=.17). Twenty-seven patients only required 1 procedure, 5 required a second ablation, and only 1 underwent VT ablation for multiple (4)recurrences. In 2 patients, ablation was done epicardially (successful in a patient with ischemic heart disease but unsuccessful in a patient with DCM).
Ablation-related complications were reported in 3 patients. These were left-bundle-branch block in 1 patient, electromechanical dissociation at the start of mapping that was recovered in 1 patient, and death within 24 hours of the procedure due to cardiac arrest in 1 patient.
After the procedure, an ICD was implanted in 4 patients, all with very severe left ventricular dysfunction. Despite achieving success with ablation of clinical VT, several VTs with different morphologies to the clinical VT were induced.
We managed to contact 20 patients, with a mean follow-up of 38.5 (27.7) months; 9 patients were alive at the time of writing (mean age, 82.2 [4.6] years) and reported a good quality of life, without recurrence of arrhythmia and, 11 patients had died, 4 due to cardiovascular causes (1 sudden death), 3 due to noncardiac causes (neoplastic disease and sepsis), and 4 due to unknown causes (1 of whom had an ICD).
DISCUSSION
Catheter ablation is an accepted alternative for the treatment of VT, with an efficacy of 55% to 70% and a complications rate of between 1.8% and 10% according to the findings of different series.10-13 The Spanish Catheter Ablation Registry for 2007 found an ablation efficacy of 69.9% for VT associated with postinfarction scarring and 65.6% for TV associated with nonischemic structural heart disease.14 These results make the procedure acceptable for the general population. However, often, it is not considered as a therapeutic option in elderly patients, who, as discussed earlier, are classed as high-risk patients. Nevertheless, there are no studies in the literature that assess the efficacy and safety of catheter ablation in this age subgroup. Traditionally, elderly patients have been excluded from clinical trials even though these should strive to faithfully reflect the target population. This would mean including elderly patients in a proportion determined by their prevalence. The results of this study in elderly patients do not differ from those published for younger populations, both in terms of success of the procedure and the rate of complications. This suggests that VT ablation is effective and relatively safe in these patients.
One aspect that should be discussed is the annual distribution of ablation procedures in this study (Figure 1). A progressive increase has been observed over the last decade, with 2002 being the year in which the most number of procedures (8) were carried out. Subsequently, despite the progressive aging of the population and resulting increase in the incidence of patients with VT, the number of patients undergoing ablation in the last 5 years has remained stable. This stable trend could result from optimization of treatment of ischemic heart disease, with early reperfusion strategies and optimum medical treatment, which have contributed to a reduction in the number of patients with postinfarction scarring and ventricular dysfunction. Another determining factor can be found in the greater number of patients with ICD in Spain. According to the Spanish Implantable Cardioverter Defibrillator Registry, in 2007, the number of ICD implants increased for secondary prevention, whereas the number for primary prevention has leveled off.15 The American and European guidelines for the management of ventricular arrhythmias and the prevention of sudden death establish ICD placement as a type I indication with evidence level A in patients with postinfarction SMVT, regardless of LVEF.16,17 However, this recommendation should be treated with caution and elderly patients should be considered on an individual basis, given that the greater number of concurrent diseases and lower life expectancy reduces the cost-effectiveness ratio of this therapy. Catheter ablation might therefore be an appropriate option.
Procedural Complications
Ablation-related procedures occurred in 3 patients (9.1%). In the literature, there are no comparative data for the complication rates in this high-risk population, although as pointed out earlier, it is similar to that described for younger populations according to different series.
Limitations
In this study, data were collected retrospectively using a database, medical records, discharge reports, and telephone contact. In addition, the single-center design of the study makes it difficult to generalize the results, as these depend on the number of ablations per center and the experience of the operators.
Thirteen patients were lost to follow-up, partly because of the long duration of the study and because many patients were referred to our hospital from other provinces in Spain. Likewise, we should remember that the assessment of quality of life by the patients is subjective.
CONCLUSIONS
Due to aging of the population, the number of elderly patients with VT susceptible to radiofrequency ablation is increasing and it increases with the coming years. Catheter ablation of VT in elderly patients with structural heart disease seems to have a similar efficacy to that published for the general population and is relatively safe. It should therefore be considered a reasonable therapeutic option in this selected population, in which therapeutic alternatives are not devoid of complications and whose cost is questioned when there are concurrent diseases or a short life expectancy.
ABBREVIATIONS
DHD: dilated heart disease
ICD: implantable cardioverter-defibrillator
IHD: ischemic heart disease
LVEF: left ventricular ejection fraction
VT: ventricular tachycardia
Correspondence: Dr. J. L. Merino.
Unidad de Investigación de Arritmias y Electrofisiología. Hospital General La Paz.
P.o de la Castellana, 261. 28046 Madrid. Spain.
E-mail: jlmerino@secardiologia.es
Received April 9, 2009.
Accepted for publication October 20, 2009.