The arterial switch operation is currently the preferred surgical approach for complete transposition of the great arteries. We sought to determine the mid-term results of this intervention.
MethodsA single-institution retrospective review of clinical records of all consecutive patients who underwent the arterial switch surgery between 1985 and 2010.
ResultsOverall, the operation was performed on 155 patients (68% boys) at a median age of 13 days: 64% with an intact septum, 46% with a ventricular septal defect, and 4.5% with associated aortic arch anomaly. The usual coronary pattern was found in 63%. Palliative surgery was performed prior to arterial switch in 6.5%. In all, 137 perioperative survivors were followed for a median of 6 years. Late mortality was 2.9%, of which 50% was due to coronary complications. Eighteen percent required surgical and/or percutaneous reintervention: 95.6% for right-sided obstruction and 4.3% for aortic regurgitation. At last follow-up, 92% had functional class I symptoms and 95% were free of arrhythmias. The left ventricular ejection fraction was greater than 55% in 95%, 28% had neoaortic regurgitation (78% mild regurgitation), and 31% had right ventricular outflow tract obstruction with a mean gradient according to echocardiography greater than 25mmHg.
ConclusionsMid-term survival of patients after arterial switch operation is excellent and their functional status is good. However, a few patients have residual lesions and a need for further intervention during follow-up, mostly for right-sided obstructions. Late mortality was uncommon and was related to coronary complications. Neoaortic root dilation and regurgitation are not major issues in early adulthood, but the long-term course of these lesions is still unknown.
Keywords
Dextro-transposition of the great arteries (d-TGA) is a common congenital heart defect that represents approximately 5% to 8% of all congenital cardiac anomalies.1 The physiologic correction of the atrium changed the natural history of this heart defect2 and, at the present time, most of the adult survivors of simple d-TGA would have undergone the Mustard or the Senning operation. Nevertheless, these techniques result in long-term complications, such as subaortic right ventricular dysfunction, systemic tricuspid valve regurgitation, symptomatic atrial arrhythmias, obstruction of intra-atrial baffles or residual shunts, and sudden cardiac death3–5; this has led to modifications in the surgical strategy. In fact, today the arterial switch operation is the technique of choice in the majority of hospitals.6 This approach to anatomical correction has the advantage of maintaining the morphologic left ventricle as the systemic ventricle and avoiding atrial incision and suture lines that predispose the patient to atrial arrhythmias. However, short- and mid-term complications, such as obstructive coronary lesions, right ventricular outflow tract obstruction, and neoaortic root dilation and regurgitation, have been identified.7–9 The initial outcomes with this surgical procedure and the management of complications during infancy and early childhood in our series of patients were reported previously.10,11 At the present time, a new population of young adults who underwent arterial switch procedures has begun to come to our adult congenital heart defects unit, and it is necessary to identify the clinical problems that require attention. Our objective is to analyze the mid-term morbidity and mortality in the patients with d-TGA who were treated with this surgical technique in a single center.
METHODSStudy PopulationWe included all the patients diagnosed during the neonatal period as having d-TGA or Taussig-Bing anomaly who underwent the arterial switch operation in the Hospital Infantil Virgen del Rocío in Seville, Spain, between 1985 and 2010, and have continued their follow-up in our health services area to the present day. Only 1 of the patients who survived surgery was excluded because there was no available information on postoperative visits and his current clinical status was unknown. The study was approved by the ethics committee of our center.
The details on anatomy, surgical techniques, and perioperative complications were obtained from surgical records. The patients were classified according to the anatomical type of d-TGA: simple, intact ventricular septum, and complex, with associated anomalies like ventricular septal defect (VSD), subpulmonary left ventricular outflow tract obstruction, and/or aortic arch anomalies (aortic coarctation, interruption or hypoplasia of the aortic arch). Taussig-Bing anomaly (double outlet right ventricle with d-TGA and subpulmonary VSD) was also included as an extreme form of complex d-TGA with VSD. The coronary anatomy was recorded at the time of surgery and the different patterns were grouped according to the classification of Yacoub and Radley-Smith12
Clinical Variables and Follow-upWe reviewed retrospectively the patients’ clinical and demographic data (including mid-term mortality, reinterventions, and complications) and the diagnostic and therapeutic procedures (Doppler echocardiography, cardiac magnetic resonance, myocardial perfusion studies—single photon emission computed tomography [SPECT], computed tomography, diagnostic and therapeutic cardiac catheterization, and surgical protocols).
Operative mortality was considered to be that occurring prior to hospital discharge or within 30 days of the arterial switch operation and late mortality, that occurring during follow-up after the 30-day postoperative period. For the analysis of mortality during follow-up, the causes of death were classified: a) sudden cardiac death; b) heart failure; c) perioperative, when it occurred within the first 30 days after a cardiac surgical intervention; d) other cardiovascular causes, such as endocarditis, pulmonary or systemic embolism, aortic rupture or dissection, or myocardial infarction, and e) nonvascular cause, such as infections, malignant tumors, or injuries. Reintervention was considered to be any percutaneous or surgical intervention during follow-up after the arterial switch operation, and significant arrhythmia was any sustained supraventricular or ventricular arrhythmia, complete atrioventricular block, or sinus node dysfunction that required treatment. Coronary artery complications were defined as follows: a) nonfatal acute coronary syndrome; b) myocardial ischemia demonstrated by SPECT, and c) obstructive lesions greater than 70% in a coronary artery according to coronary angiography.
In the final follow-up visit, functional status was assessed according to the New York Heart Association classification. We also analyzed the echocardiograms corresponding to this final clinical evaluation, all of them performed in our center in accordance with internal protocols following the current clinical guidelines.13 These studies were complemented by cardiac magnetic resonance and computed tomography angiography when the echocardiogram was not conclusive or to confirm the severity of the lesions that required treatment. Aortic regurgitation (AR) was graded semiquantitatively as mild, moderate, or severe by color Doppler echocardiography, and aortic root dimensions were determined using two-dimensional (2D) and M-mode echocardiography. A diameter greater than 36mm at the level of the sinuses of Valsalva was considered to indicate dilation. Right ventricular outflow tract obstruction was evaluated by means of 2D, color Doppler, and continuous wave Doppler echocardiography. The obstruction was considered to be moderate or severe when the peak gradient obtained with Doppler echocardiography was greater than 36mmHg or greater than 50mmHg, respectively. Depending on the location of the obstruction, it was also classified as subvalvular, valvular, or supravalvular (main pulmonary artery and right and left branches). The assessment of subaortic left ventricular function was based on the M-mode and 2D echocardiographic measurements. In case of conflicting findings, the cardiac magnetic resonance study of ventricular function was used.
Statistical AnalysisThe continuous variables are expressed as the mean (standard deviation) and the categorical variables as percentages. The follow-up time was computed from the date of the operation to the final visit or until the first episode of cardiac death or reintervention. For the purposes of this study, patients older than 14 years were classified as adults. Age and length of follow-up were considered as continuous variables and the remainder of the variables as categorical. Comparisons between groups were performed with Student t test or Mann-Whitney U test in the case of continuous variables as appropriate, depending on whether or not the distributions were normal, and with the chi-squared test for categorical variables. The analysis of survival and intervention- or complication-free survival was carried out using Kaplan-Meier curves, and the log rank test was employed to compare the survival curves. The statistical analysis was performed with the SPSS 15.0 software package for Windows (SPSS, Inc.; Chicago, Illinois, United States). A two-sided P value <.05 was considered statistically significant.
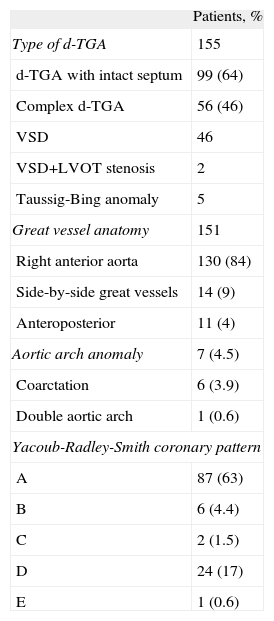
RESULTSPopulation CharacteristicsA total of 155 patients (68% boys) diagnosed as having d-TGA underwent the arterial switch operation between 1985 and 2010, 24% of them (37 patients) prior to 1998. Table 1 summarizes the baseline anatomical features of this group. Prior to this anatomical correction, Rashkind atrial septostomy with a balloon catheter was performed in 83% of the patients, and palliative surgery or surgical treatment of aortic coarctation was required in 9 patients (6%): pulmonary artery banding in 4 patients, pulmonary artery banding and Blalock-Taussig systemic-to-pulmonary artery shunt in 1 patient, aortic arch surgery in 1 patient, and aortic arch surgery and pulmonary artery banding in 3 patients. The arterial switch operation was carried out at a median age of 13 days (range, 4 days to 11 years). In all, 75% of the patients underwent surgery during the first 19 days of life and 13% at ages ranging from 20 days to 2 months.
Baseline Characteristics of the Patients With Complete Transposition of the Great Arteries Who Underwent the Arterial Switch Operation Between 1985 and 2010
| Patients, % | |
| Type of d-TGA | 155 |
| d-TGA with intact septum | 99 (64) |
| Complex d-TGA | 56 (46) |
| VSD | 46 |
| VSD+LVOT stenosis | 2 |
| Taussig-Bing anomaly | 5 |
| Great vessel anatomy | 151 |
| Right anterior aorta | 130 (84) |
| Side-by-side great vessels | 14 (9) |
| Anteroposterior | 11 (4) |
| Aortic arch anomaly | 7 (4.5) |
| Coarctation | 6 (3.9) |
| Double aortic arch | 1 (0.6) |
| Yacoub-Radley-Smith coronary pattern | |
| A | 87 (63) |
| B | 6 (4.4) |
| C | 2 (1.5) |
| D | 24 (17) |
| E | 1 (0.6) |
d-TGA, dextro (complete) transposition of the great arteries; LVOT, subpulmonary left ventricular outflow tract; VSD, ventricular septal defect.
The data are expressed as no. (%).
The overall operative mortality rate was 11.6% over the 25-year period. Although the difference did not reach statistical significance, the mortality was reduced over time, from 19% between 1985 and 1998 to 8% from 1998 to 2010. The only factors that were found to be associated with perioperative mortality were the need for previous aortic arch surgery (50% vs 1.5%; P=.004) and the cardiopulmonary bypass time (4.6% less than or equal to 200min vs 13.8% greater than 200min; P=.09). Although in the majority of cases (93%) perioperative deaths were due to coronary complications, the coronary pattern was not found to be significantly associated with early mortality: a mortality rate of 10% in patients with the favorable coronary patterns (A, D, and E) vs 20% in those with the more unfavorable patterns (B and C) (P=.3).
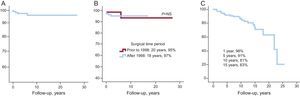
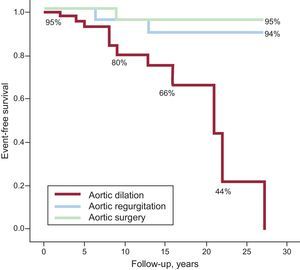
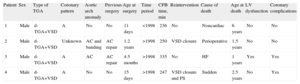
Long-term Survival and Late MortalityOver a median period of 6 years [interquartile range, 3 years to 11 years], there were 4 deaths among 137 perioperative survivors (2.9%), which represents a 20-year survival rate of 96% (Figure 1A). Although the patients operated on prior to 1998, who have now reached the age of transitioning from the pediatric clinic to the adult congenital heart disease unit, had more frequently undergone palliative surgery prior to the anatomical correction (12.5% vs 4%; P=.07), and thus were older when the surgical repair was carried out (528 days vs 22 days; P=.03), the mean mid-term to long-term survival in the two groups is comparable (Figure 1B), with good prospects for surviving surgery in both time periods. Table 2 shows the characteristics of the patients who died during follow-up. All of them had complex d-TGA with the usual coronary pattern and 2 patients (50%) required surgical treatment for severe aortic coarctation prior to the arterial switch operation. Three of the deaths were due to cardiac problems and 50% of them were secondary to coronary complications during follow-up. None of the deaths occurred during adolescence or adulthood.
Actuarial survival curves corresponding to long-term survival in the overall population of patients with complete transposition of the great arteries who underwent the arterial switch operation (A), comparing the patients treated prior to and after 1998 (B), and Kaplan-Meier curve showing long-term reintervention-free survival (C). NS, not significant.
Characteristics of the Patients Who Died During Follow-up
| Patient | Sex | Type of TGA | Coronary pattern | Aortic arch anomaly | Previous surgery | Age at surgery | Time period | CPB time, min | Reintervention | Cause of death | Age at death | LV dysfunction | Coronary complications |
| 1 | Male | d-TGA+VSD | A | No | No | 11 days | <1998 | 236 | No | Noncardiac | 6 years | No | No |
| 2 | Male | d-TGA+VSD | Unknown | AC and banding | AC repair | 1.2 years | >1998 | 250 | VSD closure | Perioperative | 1.5 years | No | No |
| 3 | Male | d-TGA+VSD | A | AC | AC repair | 4.5 months | >1998 | 335 | No | HF | 1 years | Yes | Yes |
| 4 | Male | d-TGA+VSD | A | No | No | 15 days | >1998 | 247 | VSD closure and PS | Sudden | 2.5 years | No | Yes |
AC, aortic coarctation; CPB, cardiopulmonary bypass; d-TGA, dextro (complete) transposition of the great arteries; HF, heart failure; LV, left ventricular; PS, pulmonary stenosis; TGA, transposition of the great arteries; VSD, ventricular septal defect.
In our series, 93% of the patients were in functional class I at the time of the final office visit and the remaining 7% were in class II. There were no significant arrhythmias except for asymptomatic sinus node dysfunction (1%) and atrioventricular block that required pacemaker implantation in 2% of the patients. The mean left ventricular ejection fraction was 62%, and it was less than 45% in the latest echocardiographic study in only 2.5% of the cases.
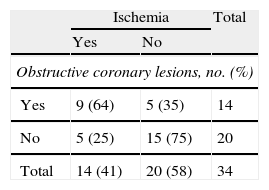
Coronary ComplicationsOnly 3 of the 137 patients developed nonfatal, surgery-related coronary complications that required early reintervention within the first 30 days after d-TGA. Ventricular dysfunction persisted in 1 of these patients. There were no symptoms of obstructive coronary artery disease in any case, nor were there coronary reinterventions during follow-up. In 8.5% of the cases, echocardiography revealed the presence of changes in segmental contractility, and left ventricular dysfunction (left ventricular ejection fraction less than 40%) was observed in only 2%. SPECT was performed in 34 patients, and fixed or reversible perfusion defects were found in 14 (41%). We had access to invasive or noninvasive coronary angiograms of 23% of the patients during follow-up. We should point out that the sensitivity of the ischemia tests (64%) proved to be low (Table 3).
Results of Noninvasive Ischemia Tests in the Detection of Obstructive Coronary Lesions and Percentage of Patients Correctly or Incorrectly Diagnosed According to the Results of Coronary Angiography
| Ischemia | Total | ||
| Yes | No | ||
| Obstructive coronary lesions, no. (%) | |||
| Yes | 9 (64) | 5 (35) | 14 |
| No | 5 (25) | 15 (75) | 20 |
| Total | 14 (41) | 20 (58) | 34 |
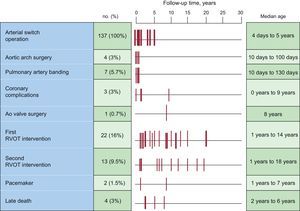
In all, 37 reinterventions were carried out in 24 patients (18%) and over half of them (54%) required more than one reintervention. In fact, reintervention-free survival was only 81% and 63% after 10 years and 15 years, respectively (Figure 1C). In our series, in no case was mortality associated with the reinterventions, and the major indications were right ventricular outflow obstruction (34 patients), AR (1 patient), and VSD closure due to patch dehiscence (2 patients). The reintervention was exclusively percutaneous in 8 patients, surgical in 3, and percutaneous with subsequent surgical treatment in 13. Figure 2 shows the temporal distribution of the interventions.
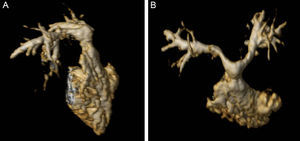
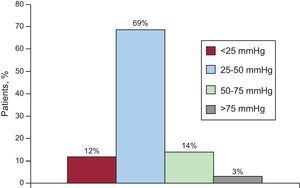
Obstructive Lesions of Right Ventricular Outflow TractIn all, 17% of the patients had lesions in right ventricular outflow tract that required intervention (Figure 3): 17 cases of main pulmonary artery stenosis, 6 cases of pulmonary branch stenosis, and 1 case of neopulmonary valve stenosis. The procedures performed were percutaneous pulmonary valvuloplasty (1 patient), main pulmonary artery angioplasty (15 patients), percutaneous stent placement in pulmonary branch (1 patient), and stent angioplasty of main pulmonary artery and branches (4 patients). Treatment was surgical in 14 patients: 10 cases of main pulmonary artery patch enlargement, 1 case of pulmonary transannular patch, and 3 patients with enlargement of main pulmonary artery and branches. The percutaneous treatment was definitive in only 38% of the cases and 55% (13/24) required a second reintervention. In the last follow-up echocardiogram (Figure 4), 31% of the patients presented some degree of right ventricular outflow tract obstruction and 17% had a peak gradient greater than 50mmHg. The incidence and degree of residual stenosis in the patients who had required reintervention during their childhood were significantly higher than those of the subjects who had not required reintervention.
Figure 5 shows the lengths of the periods of survival free of dilation, AR, and reintervention of the neoaortic root in our series of patients. Although AR was relatively common (28% of the patients), it was mild in the majority of cases (grade I, 78%; grade;grade II, 8%; and grade III, 3%), and reintervention of the valve replacement was required in only 1 case. Up to 16% of the patients had an aortic root size greater than 36mm at the level of the Valsalva sinuses. All the cases of significant AR (grade greater than III) corresponded to patients with dilated aortic root.
DISCUSSIONArterial switch during the neonatal period has become the treatment of choice for d-TGA in most hospitals because of the excellent surgical outcome and the low perioperative mortality reported by experienced surgical teams.7,9 In our referral children's hospital, this procedure has been done since 1985, at first in children with d-TGA and VSD and, at the present time, systematically in newborn infants with d-TGA with intact septum or with VSD. Our results show that the mid-term survival following anatomical correction is good and is associated with a good functional status; residual lesions in the main pulmonary artery and branches represent the most common complication and cause for reintervention.
Possible myocardial ischemia was not extensively evaluated in our retrospective series. Although the lesions are not highly symptomatic, their onset is severe, and, coinciding with the available information,14 the sensitivity of the noninvasive tests we used to detect ischemia proved to be low, coronary angiography was performed in only 21 patients. Nevertheless, coronary complication constituted an important clinical problem during follow-up, 3 patients required coronary surgery during the immediate postoperative period and both the majority of the perioperative deaths and 50% of the late deaths were due to coronary complications, which presented as sudden cardiac death in 1 case. Our data agree with the temporal distribution of risk previously described by Legendre et al.,14 who observed that the high incidence of coronary events during the early postoperative period decreases over the first months of life and slowly increases once again during late childhood and adolescence. While coronary artery arising from a single ostium and an intramural course have been associated with greater technical difficulties in the performance of the arterial switch operation15 and are considered to be the main cause of early coronary complications, a possible distortion, elongation, or extrinsic compression of the coronary arteries in relation to the progressive somatic growth of the patient would explain the development of late coronary obstructions, generally in the proximal segments, even in the presence of favorable coronary patterns.16 In recently published series,17 late death generally occurred during childhood and only exceptionally in adulthood and it was concentrated among symptomatic patients and those with residual complications. In our patient population, late cardiac death was not common and never occurred in adulthood. Nevertheless, not all coronary angiograms were available for all of our patients and only 25% of them were over 14 years of age. The duration of follow-up does not allow us to assume that the problem disappears when childhood is over. In summary, these data support the indication recently established in the guidelines18 that at least one coronary angiogram, invasive or noninvasive, be performed during adolescence and/or adulthood in these patients.
In our series, as in others published previously,7–9,17 the rate of interventions during long-term follow-up was high. The main reasons for reintervention were obstructive lesions of the right ventricular outflow tract, with a frequency of 17%, similar to that reported in the literature,19 which ranges between 7% and 28%. Supravalvular pulmonary stenosis is the most common technique-related complication. It is usually localized as a circumferential stenosis at the level of the surgical suture of the main pulmonary artery, although it also affects the bifurcation of the pulmonary artery branches, which are subjected to stretching or tension following the Lecompte maneuver. The percutaneous treatment of these lesions only proved effective in 38% of our patients, but always when performed at an early age with the shortest possible delay after the arterial switch operation.11 Even though the majority of these lesions were diagnosed and treated during childhood, right ventricular outflow tract stenosis persisted at the last follow-up visit in nearly a third of our patients, with obstruction being more frequent and more severe in the patients who had undergone reintervention during childhood.20 Residual obstruction of right ventricular outflow tract can be progressive and, moreover, it has been demonstrated to be the major determinant of exercise capacity in this population,21 which justifies the need for regular follow-up and possible future reinterventions in adulthood.
Dilation of the neoaortic root with secondary AR is the second most common vascular lesion following the arterial switch operation. The cause of these lesions is clearly multifactorial22–24 and includes anatomical factors related to the congenital defect and surgical lesions that produce hemodynamic overload in a vulnerable histological substrate, with damage to the arterial media. Previously published data show that AR has a bimodal pattern23 and that, excluding those patients who develop AR in the immediate postoperative period, there is an increase in the number of cases and the need for reintervention around the age of 15 years. Moreover, aortic dilation has been seen to be progressive during the first decades of life after surgery.22 As we observed in our distribution of the complications (Figure 2), the early development of AR and aortic dilation is rare and these lesions generally occur after a postoperative follow-up period that is nearly twice that necessary for the development of supravalvular pulmonary stenosis. Although only 2 of our patients required intervention or close monitoring, given that these lesions are progressive this may be the expression of what is still a relatively short follow-up period.
Finally, ventricular dysfunction was uncommon in our patient population and was secondary to coronary complications, generally perioperative. Some studies indicate that, even in the absence of coronary lesions, these patients develop perfusion changes due to a reduction in the coronary flow reserve because of sympathetic denervation secondary to the arterial switch operation.25 In this context, it may be that the left ventricular ejection fraction is less sensitive than long-axis function as a parameter of systolic function.
LimitationsThere are inherent limitations in the retrospective nature of the study, among them the fact that the data are obtained from follow-up and complementary examinations that were not performed in a uniform manner, particularly in the assessment of coronary complications. In our center, at present the evaluation of the coronary anatomy is carried out in accordance with a protocol; however, ischemia studies and coronary angiograms were not performed systematically in all the patients, and the results of SPECT and of coronary angiography, invasive and noninvasive, are available in very few cases. Thus, we have defined a coronary complication as an event combining clinical findings, noninvasive ischemia tests, and coronary angiography. In this context, the results concerning the prevalence of complications should be interpreted with caution to avoid reaching conclusions that cannot be deduced from the observations of this study. Likewise, we cannot provide an objective assessment of the functional capacity. Finally, the small number of complications and the relatively short follow-up period are insufficient for the identification of groups at risk for long-term complications.
CONCLUSIONSThe mid-term survival and functional status of patients who have undergone the arterial switch operation are good. Late cardiac death is not a common occurrence, but it appears to be related to coronary complications. Residual lesions of the main pulmonary artery and its branches are the most common complications and causes of reintervention. Although there are cases of early AR, the dilation of neoaortic root and significant AR develop later and their long-term course during adulthood has yet to be determined.
CONFLICTS OF INTERESTNone declared.