Controversy surrounds the long-term effects of intracoronary bone marrow stem cell transplantation after ST-elevation acute myocardial infarction (STEAMI). We report on the long-term changes in left ventricular function observed in 29 patients with STEAMI who were treated using this technique. Cardiac magnetic resonance imaging was performed at baseline, 6 months after transplantation, and long-term follow-up (median 27 months, interquartile range 24–35 months). The left ventricular ejection fraction had improved significantly by 6 months (from 47.6±8.9% to 52.7±11.6%; P=.001) and this improvement was maintained long-term, at 52.4±11.8% (P=.01 vs. baseline and P=.999 vs. 6 months). There was no significant change from baseline in end-diastolic or end-systolic ventricular volume. Our findings indicate the improvement in injection fraction occurs soon after stem cell transplantation, within the first 6 months, and remains unchanged at long-term follow-up.
Keywords
The objective of bone marrow stem cell (BMSC) therapy in ST-segment elevation acute coronary syndrome (STEACS) is the recovery of damaged myocardium following an ischemic event. Several studies have investigated this therapy. Initially, they aimed to demonstrate its safety and feasibility1,2; later, the objective was to determine its impact on parameters of ventricular function and remodeling following infarctions.1,3,4,5,6 However, the long-term effects of intracoronary BMSC transplantation on ventricular remodeling following STEACS remain controversial. Our objective is to analyze long-term outcomes for left ventricular function parameters in patients with STEACS who received intracoronary BMSC transplantation and were included in the TECAM (cell therapy applied to the myocardium) pilot study.
MethodsThe TECAM pilot study is a clinical trial to determine the feasibility and safety of an intracoronary BMSC transplantation program in patients with a recent first episode of STEACS and successful reperfusion of the artery causing it. The study took place between 2002 and 2005 and included 64 patients with STEACS with 58 months follow-up [interquartile range (IQR), 48-60]. The enrollment, transplantation and clinical follow-up protocol has been described.2
All patients underwent clinical and imaging follow-up at 6 months. In 29 patients belonging to our healthcare area, we conducted long-term clinical and cardiac magnetic resonance (CMR) imaging follow-up. These 29 patients constitute our study group. The remaining patients did not undergo long-term imaging because the original protocol did not contemplate this; their follow-up was in the hospitals of origin.
Magnetic Resonance ImagingBaseline, 6-month and long-term (27 [24-35] months) CMR imaging was performed with General Electric Signa 4.0 equipment with phased-array surface coils and body coils, and electrocardiogram-gating. We performed echo gradient sequences in apnea in longitudinal horizontal (4 cameras) and longitudinal vertical (2 cameras) planes and a full, short-axis, multi-slice gradient echo sequence of the left ventricle from base to apex.
A CMR imaging expert analyzed results at the cardiac imaging unit of the Hospital Clínico in Valladolid, north central Spain (ICICORELAB). Semiquantitative analysis of segment contractility followed a 16-segment model; quantitative analysis of ventricular volume, cardiac mass and left ventricular ejection fraction (LVEF) used MASS 6.1.2.
Statistical AnalysisContinuous variables are expressed as median [IQR] or mean±standard deviation, and categorical variables as absolute values and percentage. The assumption of normality in quantitative variables was determined with the Shapiro-Wilk test. Continuous variables were compared with the Student's t test and the Mann Whitney U test; categorical variables with chi-squared.
We used repeated measures ANOVA to determine CMR imaging parameter outcomes at baseline, 6 months, and long-term.
A value of P<.05 was considered statistically significant. Statistical analysis was with SPSS 15.0 (Chicago, Illinois, United States).
ResultsTwenty-four (83%) of the 29 patients were men; mean age was 59±11years. We compared our study group's characteristics with those of TECAM pilot study patients without long-term CMR imaging and found no differences in clinical profile, infarction size or therapy regimens (Table 1). Table 2 shows 6-month and long-term (63.5 [58-75] month) follow-up for all TECAM pilot study patients.
Table 1. Characteristics of the Study Group (29 patients) and Comparison With the Group of Patients Without Long-Term Cardiac Magnetic Resonance Imaging Follow-up (35 Patients).
| Group with long-term CMR imaging (n=29) | Group without long-term CMR imaging (n=35) | P | |
| CVRF | |||
| Smoking | 19 (66) | 19 (54) | .362 |
| Dyslipidemia | 14 (48) | 11 (31) | .169 |
| High blood pressure | 12 (41) | 12 (34) | .56 |
| Diabetes mellitus | 5 (17) | 4 (11) | .72 |
| Localization of the infarction | .835 | ||
| Anterior | 23 (79) | 27 (77) | |
| Non-anterior | 6 (21) | 8 (23) | |
| Artery causing the infarction | .632 | ||
| Left anterior descending artery | 23 (79) | 27 (77) | |
| Right descending coronary artery | 4 (14) | 7 (20) | |
| Circumflex | 2 (7) | 1 (3) | |
| Type of revascularization | .406 | ||
| Angioplasty following fibrinolysis | 20 (69) | 25 (71) | |
| Primary angioplasty | 6 (21) | 6 (17) | |
| Late angioplasty (>12h) | 3 (10) | 4 (11) | |
| Viability in dobutamine echocardiography | 7 (24) | 8 (23) | .999 |
| Treatment at discharge | |||
| ASA | 28 (97) | 33 (94) | .999 |
| Clopidogrel | 24 (83) | 31 (89) | .72 |
| Anticoagulants | 3 (10) | 5 (14) | .72 |
| Beta blockers | 26 (90) | 34 (97) | .321 |
| Calcium antagonists | 1 (3) | 1 (3) | .999 |
| ACE inhibitors | 23 (79) | 23 (66) | .228 |
| ARA-II | 1 (3) | 1 (3) | .999 |
| Pain-to-reperfusion time (min) | 173 [93-330] | 150 [90-225] | .75 |
| Pain-to-fibrinolysis time | 145 [90-200] | 135 [90-180] | .67 |
| Pain-to-needle time | 480 [300-840] | 720 [240-1320] | .446 |
| Maximum CK (U/L) | 2370 [1281-4450] | 2098 [1331-4221] | .912 |
| Maximum Troponin T (ng/mL) | 6.1 [3.1-11.4] | 6.3 [3.2-10.7] | .871 |
| Days STEACS-to-cell implantation | 11 [8-14] | 9 [7-11] | .012 |
| Number of cells implanted | 75×106 [55-120] | 79×106 [48-90] | .395 |
| CD34+ (%) | 0.92 [0.65-1.45] | 1.1 [0.82-1.7] | .254 |
| CD133+ (%) | 0.66 [0.4-0.98] | 0.76 [0.54-1.2] | .462 |
| CD117+ (%) | 2 [1.2-2.6] | 2.3 [1.6-3] | .144 |
ACE inhibitors, angiotensin converting enzyme inhibitors; ARA-II, angiotensin II receptor antagonists; ASA, acetylsalicylic acid; CK, creatine kinase; CMR imaging, cardiac magnetic resonance imaging; CVRF, cardiovascular risk factors; STEACS, ST-segment elevation acute coronary syndrome.
Data are expressed as n (%) or median [interquartile range].
Table 2. Follow-up of TECAM Pilot Study Patient Total Group at 6 Months and Long-Term.
| 6 months | Long-term | |
| CMR imaging | ||
| LVEDV (ml) | 166±46 | — |
| LVESV (ml) | 84±40 | — |
| RWMI | 1.4±0.38 | — |
| LVEF (%) | 51±12 | — |
| Clinical events during follow-up | 17 (27) | 11 (17%) |
| AMI/angina | 8 (13) | 6 (9) |
| New PTCA | 4 (6) | 4 (6) |
| Cardiovascular death | 0 | 0 |
| Non-cardiovascular death | 0 | 4 (8%) |
| Neoplasia | 0 | 3 |
| Pneumonia | 0 | 1 |
| Other | 6 (9) | 3 (5) |
| Femoral vascular complication | 2 | 0 |
| TIA | 1 | 0 |
| Atrial flutter | 1 | 0 |
| Local infection | 2 | 0 |
| Defibrillator implantation | 0 | 3 |
| NYHA clinical class III or IV | 0 | 0 |
AMI, acute myocardial infarction; CMR imaging, cardiac magnetic resonance imaging; LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction; LVESV, left ventricular end-systolic volume; NYHA, New York Heart Association; PTCA, percutaneous transluminal coronary angioplasty; RWMI, regional wall motion index; TIA, transitory ischemic accident.
Data are expressed as n (%) or mean±standard deviation.
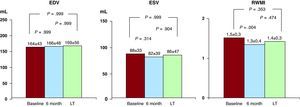
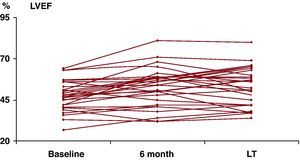
Baseline, 6-month and long-term CMR imaging follow-up results are depicted in Figure 1, Figure 2. We found no significant differences in left ventricular end-diastolic volume (EDV) or end-systolic volume (ESV) between the three studies. We found mean LVEF improved significantly at 6 months (47.6%±8.9% vs. 52.7%±11.6% (P=.001) and this continued long-term (52.4±11.8%; P=.01 vs. baseline, and P=.999 vs. 6 months, Figure 2). We also found significantly improved regional wall motion index at 6 months (1.52±0.32 baseline vs. 1.35±0.36 at 6 months, P=.004), although this was not sustained long-term (1.43±0.34, P=.353 vs. baseline).
Figure 1. Ventricular function parameter outcomes. EDV, end-diastolic volume; ESV, end-systolic volume; LT, long-term; RWMI, regional wall motion index.
Figure 2. Ejection fraction outcomes. LT, long-term; LVEF, left ventricular ejection fraction.
No factor was associated with improved LVEF in our patients. However, the low number of patients in our sample limits the validity of this finding.
DiscussionOur results indicate cell therapy produces early improvement in ventricular function that is maintained long-term, as previous studies had suggested.
Most cell therapy studies have limited follow-up (3-6 months) and BMSC transplantation following infarction usually entails a discrete but significant improvement in ventricular function parameters.1,4,6 Few studies analyze the long-term effects of this therapy and their results are controversial. Using CMR imaging at 6 months, the BOOST1 (BOne marrOw transfer to enhance ST-elevation infarct regeneration) study showed a significant improvement in LVEF in the group with cell therapy. However, at 18-month follow-up,3 differences between groups disappeared due to improvements in the control group, which equaled the cell transplant group. A REPAIR-AMI5 (Reinfusion of Enriched Progenitor cells And Infarct Remodeling in Acute Myocardial Infarction) substudy with 12-month follow-up using CMR imaging found that significant improvement in ventricular function parameters and remodeling was associated with BMSC transplantation, but only in patients with a worse baseline LVEF. The ASTAMI7 (Autologous Stem cell Transplantation in Acute Myocardial Infarction) trial 3-year follow-up found that intracoronary BMSC transplantation was not associated with improved LVEF by comparison with the control group. Cao et al's 4-year follow-up using echocardiography8 found significant improvement at 6-month follow-up in LVEF and in some parameters of remodeling in the intracoronary BMSC transplantation group. This improvement was maintained long-term.
Several explanations have been suggested for the differences between studies: low patient numbers in the sample, different follow-up imaging techniques, infarction-to-cell implantation time, cell processing, or differences in BMSC dosage administered.
The precise mechanism that leads to improved ventricular function following BMSC therapy is debatable and several hypotheses exist. Some studies report significant improvement in remodeling parameters, basically consisting of reduced ESV in the follow-up.4,5,6,8 Others suggest improvement may be explained by the increased regional wall motion index in the peri-infarction zone.1,3 Still other studies show improved LVEF without finding differences in ventricular remodeling parameters.1,4 In our group, we found significant variations in EDV or ESV at baseline, 6 months and long-term, suggesting improved LVEF in our patients is not a product of these parameters. We did find significant improvement in regional wall motion index at 6 months, which could explain the initial increase in LVEF. However, this initial improvement disappeared in long-term follow-up and cannot therefore have produced improved ventricular function in our group. Undoubtedly, the low number of patients in our sample limited our ability to find differences in these parameters.
LimitationsThe main limitation of this study is the lack of a control group. Hence, we cannot conclude that improved LVEF in our patients relates to BMSC transplantation to a greater extent than it associates with standard treatment following infarction. Another limitation is the low number of patients, which may explain why we found no significant long-term variation in ventricular volume or wall motion index. Moreover, not all patients in the original study underwent long-term CMR imaging, which may represent a selection bias even though infarction characteristics and treatment regimens did not differ between the patients who were followed up and those who were not. Obviously, randomized multicenter studies with a long follow-up are needed to confirm our results and determine the true role of BMSC therapy in post-infarction therapy following STEACS.
FundingStudy partially financed by the Spanish Cooperative Cardiovascular Disease Research Network (Red Cooperativa de Enfermedades Cardiovasculares, RECAVA) of the Instituto de Salud Carlos III.
Conflicts of interestNone declared.
Received 23 February 2010
Accepted 2 June 2010
Corresponding author: Servicio de Cardiología, Hospital Clínico Universitario de Valladolid, Avda. Ramón y Cajal 3, 47005 Valladolid, Spain. arevillaorodea@gmail.com