Keywords
INTRODUCTION
Degenerative aortic stenosis is the most common valvulopathy in Europe.1,2 In symptomatic patients with severe aortic stenosis, substitution of the affected valve for a biological or metallic prosthesis significantly improves survival.3 However, advanced age, coronary artery disease, and chronic kidney failure (among other conditions) significantly increase the risk of death during surgery,4 limiting aortic valve surgery using the sternal approach and extracorporeal circulation. Balloon valvuloplasty is inefficient and does not change the natural course of the disease in adults.5 In 2002, Cribier was the first to successfully achieve the transcatheter implantation of an aortic valve for the treatment of severe aortic stenosis.6 Transcatheter aortic valve implantation (TAVI), performed in a minimally invasive fashion either percutaneously or transapically, is a feasible therapeutic option. Irrespective of the approach chosen, the supervision of the procedure using transesophageal echocardiography would appear to be essential. Such monitoring provides important information to both interventional cardiologist and surgeon when selecting the size of the prosthetic valve to be used, as well as in its positioning, and can also positively influence the final results achieved.1,6-8 The literature contains no reports on the possible additional supervisory advantages that might be afforded by real time three dimensional transesophageal echocardiography (3D-TEE), nor on the optimization of the protocol to be followed in the operating room.
METHODS
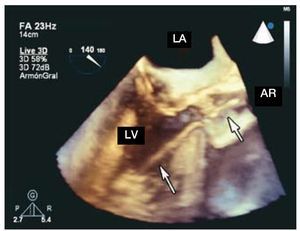
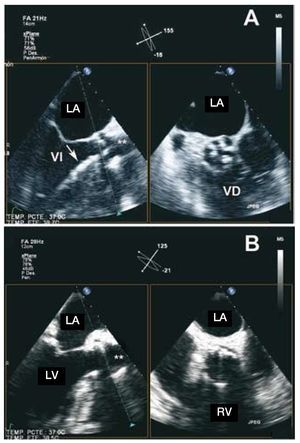
This study describes our initial experience in the intraoperative echocardiographic supervision of high surgical risk patients diagnosed with severe aortic stenosis. All patients were referred to our hospital for inclusion in the transcatheter aortic valve implantation (TAVI) program depending on the criterion of their attending physician.Valvulopathy was diagnosed by a conclusive hemodynamic study prior to intervention using 2-dimensional transthoracic echocardiography and either color Doppler or cardiac catheterization. All patients underwent coronary angiography in order to rule out severe atherosclerotic lesions and to determine the distance between the aortic ring and the coronary ostium. Three dimensional transesophageal echocardiography was performed using an iE33 apparatus and a transesophageal probe model X7-2t Live 3D with a matrix array containing 2500 elements (Philips Electronics, Eindhoven, The Netherlands). This model allows 2-dimensional conventional multiplane transesophageal, color Doppler and spectral Doppler explorations to be made. Its matrix architecture, which involves a panel of crystals, also allows one to obtain and process three dimensional images in real time (Live 3D®) (Figure 1), and in 2 orthogonal planes at 90º simultaneously (the Live xPlane® process or simply X-Plane) (Figure 2). Full volume acquisition was considered inappropriate given the need for postprocessing, which is impossible in an intraoperative setting since immediate access to information is required.
Figure 1. Three dimensional image (Live 3D® processing) of the left ventricular outflow tract, the valve and aortic root, during the positioning of an transcatheter aortic valve prosthesis (arrows). AR indicates aortic root; LA, left atrium; LV, left ventricle.
Figure 2. Three dimensional image obtained during the implantation of a transcatheter aortic valve prosthesis (X-Plane® processing); simultaneous visualization at 135° (left) and 45° (right). A: supervision of positioning of the valvuloplasty balloon (arrow) and of the prosthetic valve; B: final result of implantation. LA indicates left atrium; LV, left ventricle; RV, right ventricle. **: aortic root.
The TAVI procedure using the transapical approach was described by Lichtenstein et al.7 Echocardiographic supervision consisted of marking the position of the apex of the left ventricle (LV) in the thorax using the apical transthoracic 4 and 2 chambers view. During left minithoracotomy at the indicated point and the exteriorization and punction of the LV, 3D-TEE was used to provide data on the hemodynamics of the aortic valve (maximum aortic transvalvular velocity and effective aortic valve area, monitoring the presence and degree of aortic regurgitation) and mitral valve (monitoring presence and degree of aortic regurgitation). In order to choose the size of the prosthesis (Edwards Sapien® 23 or 26 mm transcatheter valve, using the Ascendra® implantation system [Edwards Lifesciences, Horw, Switzerland]) 3D-TEE X-Plane images of the left ventricular outflow tract diameter (LVOTD), the aortic ring, the aortic valve, and the aortic root were examined. The diameter of the aortic ring was taken from the insertion of the non-coronary leaflet to the insertion of the right coronary leaflet with a 135º viewing angle. The 2 orthogonal diameters of the aortic root at the level of the sinus of Valsalva (45º) were also measured in a plane immediately above the outflow of the coronary arteries. Other data of interest gathered included the preferential location of calcification (leaflets and commisures), and the relationship between the coronary ostia and the degree of septal hypertrophy, both of which appear to increase the risk of later complications.8
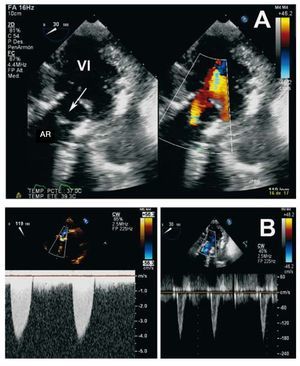
To supervise the undertaking of the aortic valvuloplasty and TAVI, real time 3D-TEE X-Plane and color Doppler (in 2 orthogonal planes at 135° and 45°) images were used (Figure 2A and B). During the anterograde insertion and positioning of the guidewire, the catheter and the 24 French introducer, checks were made for catheter or sheath entrapments and for damage to the mitral valve apparatus and intraventricular septum. The correct positioning of the valvuloplasty balloon and the prosthesis at the aortic ring was ensured. Before inflating, and using 3D-TEE X-Plane and color Doppler images, it was ensured that there was no aortic transvalvular flow during the brief interruption of the circulation controlled by rapid ventricular stimulation via the electrostimulation catheter. After inflating and expanding the prosthesis, its optimum circular expansion was qualitatively checked, along with the eccentric positing of the native leaflets, and the correct movement of the aortic leaflets. Careful checks were made to rule out periprosthetic and transprosthetic regurgitation, as well as aortic wall damage or occlusion of the coronary ostium. The introducer and guidewire were then withdrawn for final assessment using 2D X-Plane and color Doppler images, along with conventional 2D images and spectral Doppler data (deep transgastric view) (Figure 3A and B).
Figure 3. Aortic valve hemodynamic assessment before and after transthoracic implantation of the aortic valve prosthesis. A: two dimensional deep transgastric transesophageal view (left) and color Doppler (right); the prosthesis is well positioned, the leaflets show coaptation, and there is mild central regurgitation. B: spectral Doppler data obtained continuously during intraoperative transesophageal echocardiography before (left) and after (right) transthoracic implantation of the aortic valve prosthesis; note the normalization of the transvalvular flow velocity. AR indicates aortic root; LV, left ventricle.
RESULTS
Between June 2008 and March 2009, 21 patients underwent TAVI. The median age of these patients was 81 [74-84] years; 11 (52%) patients were men. The median logistic EuroSCORE value was 11 (range, 6-15). Four patients had a logistic EuroSCORE of ≤5; TAVI was deemed particularly indicated in these patients, among whom 1 had a porcelain aorta, 1 had a metallic mitral prostheses, 1 had end-stage kidney disease, and 2 had chronic obstructive pulmonary disease. In 6 patients (29%) the transapical approach was followed owing to severe aortoiliac involvement. In all cases intraoperative 3D-TEE X-Plane, color Doppler and real time sectorial 3D imaging was performed without problems, providing adequate visualization during the implantation and expansion of the prosthesis. Table shows the main echocardiographic findings. In all patients a significant reduction was seen in the maximum aortic transvalvular velocity and mean aortic pressure gradient, resulting in an increase in the effective aortic valve area.
No fatal intraoperative complications were encountered. 3D-TEE detected 4 complications. In 2 patients this involved rocking of the prosthesis and in 1 patient anterograde displacement, with migration to the LVOTD and a rotation of 90°. The appearance of severe aortic regurgitation in 2 of these 3 patients required the use of a conventional biological prosthesis. Finally, in 1 patient with marked septal hypertrophy (20 mm), 3D-TEE detected a small erosion and lifting of the endocardium due to trauma caused by the 24 French introducer; no alteration of the flow was seen after repositioning the introducer.
DISCUSSION
The present results highlight the importance of intraoperative TEE in the monitoring of TAVI when using the transapical approach. Since the introduction of TEE in the operating room its effectiveness as a monitoring system during hemodynamic management and the assessment of myocardial and valve function in patients with cardiovascular disease has become well established. Indeed, it has had an undeniable impact on surgery and the results achieved.9 Vahanian et al1 indicate the usefulness of TEE during the transcatheter implantation of prostheses, as a means of guaranteeing correct positioning and diagnosing complications. The greatest experience in TAVI has been gained employing the retrograde iliac route; the transapical route has been used much less often. Precise measurements made using TEE is vital in the selection of the size of the prosthesis, only then can the migration of the latter be avoided, optimum hemodynamics be guaranteed, and perivalvular regurgitations minimized. The use of this system also ensures the correct positioning of the prosthesis, helps avoid complications, and, following implantation, allows the checking of adequate functioning via the determination of the transprosthetic pressure gradient the valve area, and absence of regurgitation. Assessment using a 3D probe in real time, employing the X-Plane process, allows for better viewing of the prosthesis in 2 orthogonal planes simultaneously (longitudinal axis at 135° and short axis at 45° to the aortic valve); this is of great importance in the delicate positioning of the advancing device system during the implantation of the prosthesis at the aortic ring.
This paper describes a small, single center study; the findings, although promising, are therefore preliminary and the same clinical results cannot be guaranteed everywhere. However, they would appear to show that intraoperative TEE, when used as part of an optimum protocol, can provide 3D images in real time of great use in the monitoring of TAVI in patients with severe aortic stenosis.
Correspondence: Dr. P. Marcos-Alberca.
Unidad de Imagen Cardiovascular. Servicio de Cardiología. Instituto Cardiovascular. Hospital Clínico San Carlos. Universidad Complutense. Prof. Martín Lagos, s/n. 28040 Madrid. Spain.
E-mail: pmarcosa.hcsc@salud.madrid.org
Received August 28, 2008.
Accepted for publication June 18, 2009.