Current postoperative management of adult cardiac surgery often comprises transfer from the intensive care unit (ICU) to a conventional ward. Intermediate care units (IMCU) permit hospital resource optimization. We analyzed the impact of an IMCU on length of stay (both ICU and in-hospital) and outcomes (in-hospital mortality and 30-day readmissions) after adult cardiac surgery (IMCU-CS).
MethodsFrom November 2012 to April 2015, 1324 consecutive patients were admitted to a university hospital for cardiac surgery. In May 2014, an IMCU-CS was established for postoperative care. For the purposes of this study, patients were classified into 2 groups, depending on the admission period: pre-IMCU-CS (November 2012-April 2014, n=674) and post-IMCU-CS (May 2014-April 2015, n=650).
ResultsThere were no statistically significant differences in age, sex, risk factors, comorbidities, EuroSCORE 2, left ventricular ejection fraction, or the types of surgery (valvular in 53%, coronary in 26%, valvular plus coronary in 11.5%, and aorta in 1.8%). The ICU length of stay decreased from 4.9±11 to 2.9±6 days (mean±standard deviation; P<.001); 2 [1-4] to 1 [0-3] (median [Q1-Q3]); in-hospital length of stay decreased from 13.5±15 to 12.7±11 days (mean±standard deviation; P=.01); 9 [7-13] to 9 [7-11] (median [Q1-Q3]), in pre-IMCU-CS to post-IMCU-CS, respectively. There were no statistically significant differences in in-hospital mortality (4.9% vs 3.5%; P=.28) or 30-day readmission rate (4.3% vs 4.2%; P=.89).
ConclusionsAfter the establishment of an IMCU-CS for postoperative cardiac surgery, there was a reduction in ICU and in-hospital mean lengths of stay with no increase in in-hospital mortality or 30-day readmissions.
Keywords
Cardiac surgery is the preferred therapeutic approach for the treatment of many cardiovascular diseases. Because it is invasive, this type of surgery involves a significant amount of health care resources, especially those related to critical care. Strategies are necessary to optimize hospital resources and improve efficiency without negatively affecting clinical outcomes.
In the past decade, likely due to advances in perioperative cardiac care, cardiac surgery-related mortality has decreased significantly.1 By contrast, postoperative morbidity has increased, mainly because patients who undergo cardiac surgery are older, more frail, and have more comorbilities.2 Hence, postoperative cardiac care is critical to overall surgical success and patients’ clinical recovery.
In the field of general intensive care medicine, the establishment of intermediate care units (IMCUs) for patients who do not require full intensive care but who need more services than are available on hospital wards3–5 allows for earlier discharge from intensive care units (ICU), facilitates patient allocation, and helps to reduce costs.6,7 Although many hospitals now have IMCUs, there is little evidence to support their benefit in the context of postoperative cardiac surgery (the IMCU-CS), an area that represents a substantial economic burden to hospitals.8,9 Accordingly, we evaluated whether the introduction of an IMCU-CS to the cardiac surgery postoperative process has an impact on lengths of stay (both ICU and in-hospital) and outcomes (both in-hospital mortality and 30-day readmission).
METHODSThis is a retrospective longitudinal observational study. Between November 2012 and April 2015, 1324 consecutive patients were admitted for cardiac surgery to a university hospital. In May 2014, an IMCU-CS was created for postoperative patient care. For the purposes of the present study, patients were classified into 2 groups, depending on the admission period: pre-IMCU-CS (November 2012-April 2014; n=674) and post-IMCU-CS (May 2014-April 2015; n=650).
Data collection was performed prospectively by members of the cardiology and cardiac surgery departments following the official registry of the Spanish Society of Thoracic and Cardiovascular Surgery with complementary variables since the establishment of the IMCU-CS. Staff members of the cardiology and cardiovascular surgery departments collected data and entered them into the database with a comprehensive check with the official registry of our hospital. We analyzed demographic and clinical data, as well as postoperative complications, in-hospital length of stay (LoS) and outcomes. The main variables analyzed are defined as follows:
- •
ICU stay: cardiac ICU in LoS.
- •
Hospital stay: total hospitalization in LoS in our hospital.
- •
ICU readmission: cardiac ICU readmission during hospitalization.
- •
Hospital mortality: hospitalization mortality in our hospital, as well as patients transferred to their reference centers.
- •
30-day readmission: hospital readmission related to the cardiac surgery postoperative process or admission for a cardiovascular reason within 30 days after discharge.
The cardiac surgery department of our institution was created in the year 2000 and now consists of 2 cardiac operating rooms, 8 cardiac ICU beds, and 16 beds in the cardiac surgery ward. The ICU team has 4 intensive care physicians and a nurse-to-patient ratio of 1:2.
The IMCU-CS consists of 8 hospital beds (4 double bedrooms) equipped with continuous noninvasive cardiac monitoring. It has a multidisciplinary team consisting of 2 cardiologists with support from cardiac surgery staff10 and a nurse-to-patient ratio of 1:4. The IMCU-CS has a cardiologist on duty 24h/d. A clinical protocol was defined with the creation of the IMCU-CS, for cardiac surgery patients, including admission to the IMCU-CS for all patients discharged from the cardiac ICU before they were admitted to a conventional bed or cardiac ward. The main purpose of the IMCU-CS is to provide cardiac support to allow early discharge from the cardiac ICU for patients who need strict clinical and/or hemodynamic monitoring and require substantial nursing time. It is used for patients who are receiving low-dose inotropes and/or vasoactive agents or undergoing mediastinal/pleural drainage or who have conditions such as heart rhythm disorders and myopathy but who do not need mechanical ventilation or continuous renal replacement therapy.
Statistical AnalysisCategorical data are expressed as number and percentage and quantitative variables as mean±standard deviation (SD) or median [Q1-Q3]. Normal distributions were assessed by normal Q-Q plots. Groups were compared with the chi-square test and the Student t test or nonparametric tests (Mann Whitney U test) when required. For the lineal regression analyses, ICU and in-hospital LoS were log-transformed due to skewed distribution. In theses analyses, the variables with statistical significance in the univariate analysis, as well as those that were considered clinically relevant such as age, sex, kidney failure, diabetes, chronic obstructive pulmonary disease, New York Heart Association class, and left ventricular ejection fraction, were included as covariates. All data analyses were performed with SPSS version 15 (SPSS Inc, Chicago, Illinois, United States). P values of<.05 were considered significant.
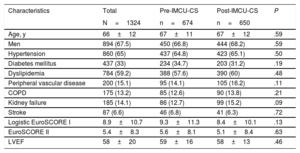
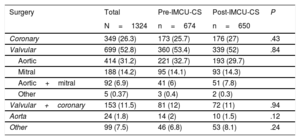
RESULTSWe analyzed 1324 consecutive patients who underwent cardiac surgery between November 2012 and April 2015 and divided them into 2 groups: 674 patients pre-IMCU-CS and 650 patients post-IMCU-CS. Vital status was available in 98.1% of the patients (only 26 patients were lost to follow-up). Demographic and clinical baseline characteristics are shown in Table 1. There were no statistically significant differences in age, sex, risk factors, comorbidities, EuroSCORE 1 and 2, or left ventricular ejection fraction between the 2 groups. Similarly, there were no statistically significant differences between the 2 groups in the type of surgery (Table 2).
Demographic and Clinical Baseline Characteristics
| Characteristics | Total | Pre-IMCU-CS | Post-IMCU-CS | P |
|---|---|---|---|---|
| N=1324 | n=674 | n=650 | ||
| Age, y | 66±12 | 67±11 | 67±12 | .59 |
| Men | 894 (67.5) | 450 (66.8) | 444 (68.2) | .59 |
| Hypertension | 860 (65) | 437 (64.8) | 423 (65.1) | .50 |
| Diabetes mellitus | 437 (33) | 234 (34.7) | 203 (31.2) | .19 |
| Dyslipidemia | 784 (59.2) | 388 (57.6) | 390 (60) | .48 |
| Peripheral vascular disease | 200 (15.1) | 95 (14.1) | 105 (16.2) | .11 |
| COPD | 175 (13.2) | 85 (12.6) | 90 (13.8) | .21 |
| Kidney failure | 185 (14.1) | 86 (12.7) | 99 (15.2) | .09 |
| Stroke | 87 (6.6) | 46 (6.8) | 41 (6.3) | .72 |
| Logistic EuroSCORE I | 8.9±10.7 | 9.3±11.3 | 8.4±10.1 | .13 |
| EuroSCORE II | 5.4±8.3 | 5.6±8.1 | 5.1±8.4 | .63 |
| LVEF | 58±20 | 59±16 | 58±13 | .46 |
COPD, chronic obstructive pulmonary disease; IMCU-CS, intermediate care unit after cardiac surgery; LVEF, left ventricular ejection fraction.
Data are expressed as No. (%) or mean±standard deviation.
Types of Surgery
| Surgery | Total | Pre-IMCU-CS | Post-IMCU-CS | P |
|---|---|---|---|---|
| N=1324 | n=674 | n=650 | ||
| Coronary | 349 (26.3) | 173 (25.7) | 176 (27) | .43 |
| Valvular | 699 (52.8) | 360 (53.4) | 339 (52) | .84 |
| Aortic | 414 (31.2) | 221 (32.7) | 193 (29.7) | |
| Mitral | 188 (14.2) | 95 (14.1) | 93 (14.3) | |
| Aortic+mitral | 92 (6.9) | 41 (6) | 51 (7.8) | |
| Other | 5 (0.37) | 3 (0.4) | 2 (0.3) | |
| Valvular+coronary | 153 (11.5) | 81 (12) | 72 (11) | .94 |
| Aorta | 24 (1.8) | 14 (2) | 10 (1.5) | .12 |
| Other | 99 (7.5) | 46 (6.8) | 53 (8.1) | .24 |
IMCU-CS, intermediate care unit after cardiac surgery.
Data are expressed as No. (%).
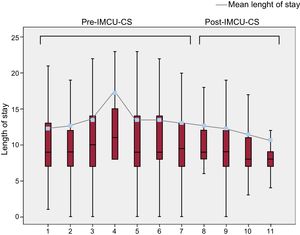
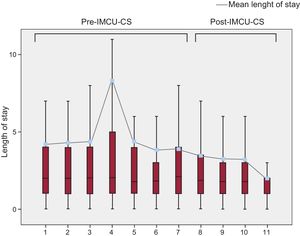
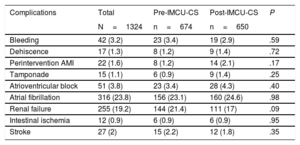
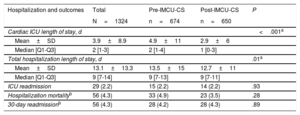
Table 3 summarizes postoperative complications, which were not statistically significant differences between the 2 groups. Table 4 shows ICU and in-hospital LoS for the whole cohort and for the 2 study period cohorts. Both ICU (P<.001) and in-hospital (P=.01) LoS significantly decreased in the post-IMCU-CS period compared with the pre-IMCU-CS period. To calculate in-hospital LoS, we considered the days that patients remained in our center, but 9.7% of patients (12.01% of pre-IMCU-CS patients and 7.38% of post-IMCU-CS; P=.006) were transferred to the reference community hospital to complete recovery. Figure 1 and Figure 2 show the mean and median of ICU and in-hospital LoS, grouping the study period in quarterly intervals.
Postoperative Complications
| Complications | Total | Pre-IMCU-CS | Post-IMCU-CS | P |
|---|---|---|---|---|
| N=1324 | n=674 | n=650 | ||
| Bleeding | 42 (3.2) | 23 (3.4) | 19 (2.9) | .59 |
| Dehiscence | 17 (1.3) | 8 (1.2) | 9 (1.4) | .72 |
| Perintervention AMI | 22 (1.6) | 8 (1.2) | 14 (2.1) | .17 |
| Tamponade | 15 (1.1) | 6 (0.9) | 9 (1.4) | .25 |
| Atrioventricular block | 51 (3.8) | 23 (3.4) | 28 (4.3) | .40 |
| Atrial fibrillation | 316 (23.8) | 156 (23.1) | 160 (24.6) | .98 |
| Renal failure | 255 (19.2) | 144 (21.4) | 111 (17) | .09 |
| Intestinal ischemia | 12 (0.9) | 6 (0.9) | 6 (0.9) | .95 |
| Stroke | 27 (2) | 15 (2.2) | 12 (1.8) | .35 |
AMI, acute myocardial infarction; IMCU-CS, intermediate care unit after cardiac surgery.
Data are expressed as No. (%).
Hospitalization and Early Postdischarge Outcomes
| Hospitalization and outcomes | Total | Pre-IMCU-CS | Post-IMCU-CS | P |
|---|---|---|---|---|
| N=1324 | n=674 | n=650 | ||
| Cardiac ICU length of stay, d | <.001a | |||
| Mean±SD | 3.9±8.9 | 4.9±11 | 2.9±6 | |
| Median [Q1-Q3] | 2 [1-3] | 2 [1-4] | 1 [0-3] | |
| Total hospitalization length of stay, d | .01a | |||
| Mean±SD | 13.1±13.3 | 13.5±15 | 12.7±11 | |
| Median [Q1-Q3] | 9 [7-14] | 9 [7-13] | 9 [7-11] | |
| ICU readmission | 29 (2.2) | 15 (2.2) | 14 (2.2) | .93 |
| Hospitalization mortalityb | 56 (4.3) | 33 (4.9) | 23 (3.5) | .28 |
| 30-day readmissionb | 56 (4.3) | 28 (4.2) | 28 (4.3) | .89 |
ICU, intensive care unit; IMCU-CS, intermediate care unit after cardiac surgery; SD, standard deviation.
Unless otherwise indicated, the data are expressed as No. (%).
On multivariable lineal regression analyses, the study period (pre-IMCU-CS/post-IMCU-CS) remained significantly independently associated with a shorter ICU (standardized beta value –0077; 95% confidence interval, –0.259 to –0.038; P=.008) and in-hospital mean LoS (standardized beta value –0.066; 95% confidence interval, –0.135 to –0.016; P=.01). Likewise, the study period (pre-IMCU-CS/post-IMCU-CS) did not remain significantly independently associated with in-hospital mortality or 30-day readmission. The main cause of cardiac ICU readmission during hospitalization was respiratory failure; there was no difference in the incidence of cardiac ICU readmission between the study groups (P=.93, Table 4). The mean LoS in the IMCU-CS was 3.5±2.6 days. An analysis of clinical outcomes showed no significant differences in in-hospital mortality (4.9% vs 3.5%, P=.28) or 30-day readmission rate (4.3% vs 4.2%; P=.89) for pre-IMCU-CS compared with post-IMCU-CS, respectively.
In the pre-IMCU-CS period, only 85% of patients underwent cardiac surgery in less than 90 days. After the creation of the IMCU-CS, 100% of patients underwent cardiac surgery in less than 90 days, according the official management of Health Department in 2014.11
DISCUSSIONThe implementation of an IMCU-CS for postoperative care after cardiac surgery was associated with a reduction in total in-hospital and ICU LoS. We observed no increases in postoperative complications, in-hospital mortality, or 30-day hospital readmission rate. Although our observational studies did not allow us to establish a definitive cause-effect relationship between the reduction in in-hospital LoS and the creation of an IMCU-CS, this reduction was achieved with the same surgical bays, number of ICU beds, and without changes in surgical techniques. This fact suggests that the creation of the IMCU-CS played a major role in this LoS reduction.
In July 2014, the Catalan government (an autonomous region in Spain with 7.5 million inhabitants) issued an official instruction to reduce cardiac surgery waiting lists. The population of Catalonia is now served by 5 cardiac surgery centers, each responsible for the acute and nonacute surgical care of 1.5 million inhabitants.11 The clinical impact of this regulation on our center was a marked increase in open chest surgeries, from 479 in 2013 to 673 in 2015, although there was a shortage of cardiac ICU beds. This prompted the creation of an IMCU-CS to promote earlier ICU patient discharge.12,13 It is known that the main factor limiting the number of cardiac operations is the availability of critical care beds.14 Moreover, it has been demonstrated that prolonged ICU stay is associated with poor patient outcome and increased costs.15–17 The implementation of an IMCU-CS allowed cardiac surgery waiting lists to be reduced to less than 90 days in line with official instruction.
Although the multiple benefits of IMCUs in terms of efficient health care resource management are well established,18 there are at present few data regarding the use of IMCU-CSs in the field of cardiac surgery. Byrick et al.14 in the 1980s and Mazer et al.19 in the 1990s studied different patterns of critical care services used after cardiac surgery to evaluate whether variations in the process of care influence patient outcome. Intermediate care units facilitate earlier ICU discharge for patients who do not require intensive care, while also avoiding the premature discharge of patients who are not clinically stable enough to be in a conventional ward. In addition, they are a good option for patients on conventional wards who suddenly worsen and need closer clinical monitoring but do not fulfill ICU criteria transfer; transfer to the IMCU probably prevents subsequent ICU readmission.20 Furthermore, IMCUs help to improve ICU efficiency by allowing for optimal selection of appropriate patients for admittance to the ICU.21,22
Our results revealed similar outcomes in terms of ICU readmission, in-hospital mortality, and 30-day readmission between pre-IMCU-CS and post-IMCU-CS groups, suggesting that placing patients in an IMCU-CS is a safe means of achieving earlier ICU discharge. Indeed, we found a cardiac ICU readmission rate of 2.2%; according to previously published studies, the cardiac ICU readmission rate can be as high as 7%.23,24 Cardiac ICU readmission is associated with worse prognosis, longer in-hospital LoS, and increased mortality.25–28 Moreover, in terms of general intensive care medicine, the existence of IMCUs has been associated with lower in-hospital mortality rates because of a reduction in the number of deaths on general wards.23,29,30 In our study, in-hospital mortality was not significantly different between the 2 study groups. Eventually, studies with larger cohorts might be able to shed more light on this issue.
Cost-effectiveness analyses of general intensive care models have yielded controversial results. In general, those that did not confirm a reduction in total hospital costs after the introduction of an IMCU-CS had issues related to study design, such as a wide range of illness severities or inaccurate ICU admission criteria.31–33 Moreover, the fact that patients admitted to IMCU are usually “low-risk patients” may generate lower ICU costs.34,35 Total critical care costs are directly related to LoS, the procedures performed, and complications during admission.9 Currently, to our knowledge, there are no cost-effectiveness data regarding the impact of IMCU-CS in the specific context of postoperative care after cardiac surgery. Our institution, a public center of the National Health Service in Catalonia, is ill-equipped to perform a cost-effectiveness analysis of a cardiac surgery IMCU-CS.
StrengthsDespite its single-center nature, the strengths of the present report include the consecutive inclusion of more than 1300 cardiac surgery patients who were operated on by the same surgical team. Additional reports of experiences with cardiac surgery IMCU-CS, including a full economic analysis,36 are needed to support their implementation.
CONCLUSIONSAfter the creation of an IMCU-CS designed for adult postoperative care after cardiac surgery, the mean ICU and in-hospital LoS were reduced without negatively affecting either in-hospital mortality or 30-day readmission. The establishment of the IMCU-CS allowed us to increase the number of cardiac surgeries performed in a single hospital without making structural changes in the ICU.
CONFLICTS OF INTERESTNone declared.
- –
In the general intensive care medicine scenario, the establishment of IMCU for patients who do not require full intensive care but still need closer monitoring than that available on hospital wards has demonstrated its usefulness. These units allows earlier discharge from the ICU and facilitate patient allocation. Likewise, the benefits of IMCU are well established in terms of efficient health care resource management. However, there is scarce evidence to support their benefit in the setting of postoperative cardiac surgery.
- –
This study provides novel and relevant data on the benefits of the creation of an IMCU-CS. This new management in cardiac surgery patients allows an increase in the number of cardiac surgeries performed in a single hospital without making structural changes in the ICU, achieving a reduction in cardiac surgery waiting lists. This novel system has been able to reduce overall in-hospital and ICU LoS, without negative effects on patient prognosis (in-hospital mortality or 30-day readmission).
.