Keywords
INTRODUCTION
Patients attended for non-ST segment elevation acute coronary syndrome (NSTEACS) constitute a wide-ranging clinical population. If prognostic stratification of these patients were rapid (ideally on admission) and simple, efficacy and efficiency would improve because we could easily identify higher-risk patients who might benefit from more costly, more aggressive medical and interventional therapies. To this extent, several risk scores (RS) for NSTEACS have been described.1,2 However, most of these are limited in that some of the variables on which they are based are not obtained immediately "at the patient's bedside" because they are either analytical or data-based variables that are not always obvious from the patient's clinical record.
In contrast, the electrocardiogram (ECG), given its universal availability, low cost and simplicity, is an essential tool in the diagnosis and prognostic stratification of NSTEACS. In this clinical context, ECG variables like ST-segment depression,3 QRS complex length4or corrected QT interval (QTc) have been investigated.5-7
The objective of the present study is to describe prospectively, in a non-selected population of patients in sinus rhythm attended for NSTEACS, a new RS that is based exclusively on ECG variables obtained on admission.
METHODS
Study Population
We included all patients with a definitive diagnosis of NSTEACS (typical chest pain, dynamic ST-segment changes and/or myocardial damage marker elevation) with the last episode of chest pain in the previous 24 h. We considered myocardial damage markers were elevated when the maximum serum value surpassed our laboratory's upper limit for normal (troponin I, ≥0.1 µg/L; MB fraction of creatine kinase [CK-MB] mass, ≥5 µg/L). We excluded patients with atrial fibrillation, receiving group Ia or III antiarrhythmic drugs, or with hypopotassemia, as these impede or interfere with QTc interval measurement. Diagnosis and treatment were conducted in line with European Cardiology Society Clinical Practice Guidelines.
Electrocardiographic Analysis
We analyzed the first ECG performed following patient arrival at our center. We analyzed the following variables: heart rate ≥85 beats/min, left atrial enlargement (LAE),8 defined by a ≥1 m negative terminal deflection in V1 of the P wave, 2 or more pathologic Q waves in concordant leads, QRS complex length ≥100 ms,4 left ventricular enlargement (Sokolov index >35 mm), Bazett's QTc interval ≥450 ms,5 >0.5 mmST-segment depression,3 and presence of two or more concordant leads with ≥2 mm negative T wave.
Objective
To construct an RS based exclusively on electrocardiographic variables (ECG-RS) with predictive power for the outcome of death or recurrent ischemia (D-RIsch) during hospitalization. We defined recurrent ischemia as the reappearance of anginal chest pain together with any of the following: ST-segment elevation in at least two concordant leads, >0.5 mm ST-segment depression and ≥20% increase in serum troponin I concentration.
Statistical Analysis
Statistical analysis was with SPSS 11.5 for Windows (SPSS Inc., Chicago, Illinois, USA). Continuous variables with a normal distribution are described as mean and SD; categorical variables are expressed as absolute number and percentage. Comparison of categorical variables was with c2. Multivariate analysis was with logistic regression. We considered P<.05 statistically significant.
RESULTS
From January 2002 to December 2004, 523 consecutive patients were attended for NSTEACS in our center. We excluded patients with atrial fibrillation (n=69), receiving group Ia or III antiarrhythmic drugs (n=16), or with hypopotassemia on admission (n=11). Demographic characteristics of the remaining 427 patients are in Table 1.
Incidence of D-RIsch was 155 patients (36%), of whom 25 (5.9%) died. Recurrent ischemia took the form of recurrent angina in 88 patients (59%) and reinfarction in 60 (41%).
Electrocardiographic Variables With Independent Prognostic Value
We conducted logistic regression analysis for D-RIsch during hospitalization. This included the ECG variables under study, those in the TIMI RS,1 gender and Killip class. As Table 2 indicates, only three ECG variables showed independent prognostic power: >0.5 mm ST-segment depression, ≥450 ms QTc, and LAE. These variables constituted the ECG-RS and, as a function of the odds ratio (OR), ≥ 450 ms QTc scored 3 points, >0.5 mm ST scored 2, and presence of LAE scored 1.
Prognostic Value of the Risk Score Based Exclusively on Electrocardiographic Variables
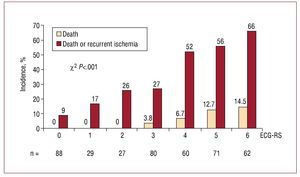
Incidence of D-RIsch showed a linear increase with respect to ECG-RS score. (Figure 1). The validity of our model was endorsed by using the Hosmer-Lemeshow test (c statistic =2.9; P=.3). The area beneath the ROC curve was 0.75 (0.70-0.78), which enabled us to judge that the ECG-RS discriminates adequately between patients at different levels of risk. The area beneath the ROC curve for in-hospital death was 0.78 (0.71-0.84).
Figure 1. Incidence of death and death or recurrent ischemia according to the ECG-RS.
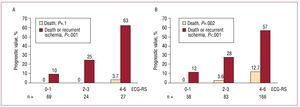
After classifying patients in three groups according to their ECG-RS scores (≤1, 2-3, ≥4), we found stratification for risk of death (0% vs 2.8% vs 11.4%; P<.001) and risk of D-RIsch (11% vs 27% vs 58%; P<.001) was satisfactory. This level of prognostic capability was demonstrated both in unstable angina and non-Q wave infarction (Figure 2). The indices of statistical validity for D-RIsch of the ECG-RS cutoff points are described in Table 3.
Figure 2. Prognostic value of the electrocardiographic variable-based risk score in unstable angina (A) and non-Q wave myocardial infarction (B) ECG-RS.
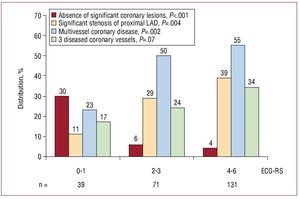
Figure 3 shows the relation between ECG-RS and coronary anatomy, which was less favorable for ECG-RS ≥4. Coronary revascularization was associated with lower mortality in patients with ECG-RS ≥4: 3.5% versus 18% (non-adjusted P=.002), but not with ECG-RS <4: 0% versus 1.8% (non-adjusted P=.2).
Figure 3. Relation between electrocardiographic variable-based risk score and coronary anatomy. ECG-RS indicates rish score based on electrocardiographyc variables obtained on admission; LAD, left anterior descending artery.
DISCUSSION
Our data indicate that an RS derived from the ECG performed on admission facilitates the creation of a classification system that precisely predicts short-term risk of death and ischemic events in NSTEACS. This new ECG-RS includes only ECG variables that in previous studies have shown prognostic capability and that in our series maintain predictive power independently of the TIMI RS variables. We chose the TIMI RS as the benchmark in multivariate analysis because it is widely used and simple, and has a prognostic capability similar to other RSs.9
This new ECG-RS is obtained immediately, without the delay inherent in obtaining analytical results. It is simple to apply, based on quantifiable (and therefore objective) variables, and universally available. Hence, it could be used for the rapid risk stratification of suspected coronary origin chest pain and in decision-making on therapy, beyond simple ST-segment analysis.10
However, despite the fact that our data are a faithful reflection of daily clinical practice, given that the size of our study population is relatively small and that revascularization frequency was low (in our opinion, these are the principle limitations of this work), further research will be needed, based on broader-ranging cohorts, particularly in centers where invasive management is more frequent, to confirm our results and the practical implications derived from them.
Correspondence: Dr. J. Jiménez-Candil. Hospital Universitario de Salamanca.
P.o de San Vicente, 58-182. 37007 Salamanca. Spain.
E-mail: jimenezcandil@secardiologia.es
Received January 7, 2009.
Accepted for publication July 23, 2009.