Multidetector computed tomography (MDCT) has been demonstrated as a feasible alternative to invasive coronary angiography (ICA). However, contradictory results have been reported regarding the effect of coronary artery calcium score (CS) on the diagnostic accuracy of MDCT. Our aim was to assess the agreement of MDCT and ICA and to evaluate the influence of CS on this agreement.
MethodsWe enrolled 266 consecutive patients who underwent evaluation with 64-slice MDCT and ICA. Standard CS software tools were used to calculate the Agatston score. Stenosis was qualitatively classified as mild, moderate, or severe by 1 blinded observer and the results were compared with those of ICA, which was used as the gold standard.
ResultsThe mean age of the patients was 65.4 ± 11.2 years, and 188 patients (70.3%) were men. A total of 484 segments with coronary stenosis ≥ mild were qualitatively evaluated and quantified with MDCT. Noninvasive measurements were concordant with ICA in 402 stenoses (83.05%; Kappa, 0.684), with no significant differences between vessels and with no statistically significant influence of CS on this agreement (OR, 0.93; 95%CI, 0.76-1.09; P = .21). Multidetector computed tomography had high sensitivity, specificity, positive predictive value, and negative predictive value on a per-segment, per-vessel, and per-patient basis.
ConclusionsNon-ICA using MDCT showed good agreement with ICA in the qualitative quantification coronary stenosis and CS had no significant impact on this agreement.
Keywords
Over the past few years, multidetector computed tomography (MDCT) has been demonstrated as a feasible alternative to invasive coronary angiography (ICA), allowing noninvasive evaluation of the coronary arteries.1–4 However, contradictory results have been reported regarding the effect of coronary artery calcium score (CS) on the diagnostic accuracy of MDCT.5,6 With the first generations of MDCT scanners, severe coronary calcifications were recognized as an important factor hampering precise evaluation of coronary artery stenosis, thereby limiting diagnostic accuracy. Calcified plaques produce artifacts (blooming) which may affect the evaluation of luminal obstruction.7 At the same time, more extensive coronary calcification increases the likelihood that the patient has obstructive coronary artery disease,8,9 and ICA is usually required for definitive diagnosis and treatment. Advances in temporal and spatial resolution, especially the introduction of 64-detector rows, and growing experience concerning strategies for optimization of image quality, have allowed high-quality noninvasive angiograms to be conducted in most patients. The purpose of the present study was to evaluate the validity and agreement of MDCT and ICA in patients with coronary artery disease and to evaluate the impact of coronary artery CS on the diagnostic accuracy of MDCT.
METHODSStudy PopulationA total of 271 consecutive patients who were evaluated with 64-slice MDCT and who subsequently underwent ICA were evaluated; 5 patients were excluded because of a lack of image quality (eg, coronary motion, vessel size, breathing artifacts) or technical scan insufficiencies (eg, scan abortion, misplaced scan range, poorly executed contrast media timing, or electrocardiogram [ECG] misregistrations), resulting in a final sample of 266 patients. Demographic and clinical characteristics, including age, sex, cardiovascular risk factors (hypertension, diabetes mellitus, hyperlipidemia, smoking status), kidney failure, and peripheral arterial disease were identified. Kidney failure was defined as a serum creatinine level of more than 1.3mg/dL (115μmol/L). Patients with atrial fibrillation, significant renal insufficiency, or a history of significant iodinated contrast allergy were excluded. In addition, we excluded those with a previously documented history of obstructive coronary artery disease. The decision to perform ICA and MDCT was taken by the patient's physician in all cases based on age, risk factors for coronary artery disease, and the severity or persistence of symptoms. All patients gave written informed consent for ICA and MDCT.
Multidetector Computed Tomography AcquisitionsMDCT data were acquired using Brilliance 64 MDCT (Philips Medical Systems, Best, The Netherlands). Before CS and MDCT examinations, heart rate and blood pressure were monitored. In the absence of contraindications, participants received propranolol (5-15mg intravenously) if the resting heart rate exceeded 65 bpm. All participants were in sinus rhythm. The heart rate of all participants ranged between 45 and 77 bpm (average, 62 ± 6 bpm) with or without premedication. Sublingual nitroglycerin was routinely used 1minute before MDCT to dilate coronary arteries. The participants were imaged in the supine position. The participants were instructed to maintain an inspiratory breathhold during which the MDCT data and ECG trace were acquired. Scanning was performed from the tracheal bifurcation to 1cm below the diaphragmatic portion of the heart. First, an ECG-gated scan without contrast media was performed to determine the CS. After a scout scan, a volume of 80 to 120mL of contrast media (iopamidol 370mg/mL, Bracco) was injected intravenously via an 18-gauge catheter placed in the antecubital vein, at a rate of 5mL/s and controlled with a bolus-tracking technique, followed by a 50-mL bolus of saline. Scanning started automatically with a delay of 5seconds after a predefined threshold of 140 HU was reached in the aortic root. Scanning was performed at 120kV, with an effective tube current of 600 to 1000 mAs, slice collimation of 64 × 0.625mm acquisition, gantry rotation time of 0.4seconds, and pitch of 0.2. Image reconstruction was routinely performed using the retrospective ECG-gating method. A prospective ECG-gated scan using the “step-and-shoot” protocol was only performed in thin patients with a heart rate < 65 bpm. In this study, 67.4% of the MDCT examinations were retrospective and 32.6% were prospective. The effective dose of MDCT was estimated from the dose-length product and an organ weighing factor [k = 0.017 mSv × (mGy × cm)−1] for the chest as the investigated anatomical region.
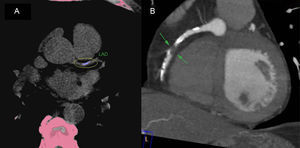
Image Processing and AnalysisPostprocessing of the CS and MDCT examinations was performed on dedicated workstations (Philips Extended Brilliance Workspace). For each study, a CS was determined using the methods of Agatston et al.10 Coronary CS was measured without contrast using semiautomatic software (HeartBeat CS, Philips Medical Systems), which displayed colored spots for calcium to be manually marked by the operator and automatically calculated all spots to a summed CS (Figure). A CS was calculated for each epicardial coronary segment and recorded as a composite (ie, total or summed) score for the entire epicardial coronary system (left main, left anterior descending, left circumflex, and right coronary arteries). Contrast-enhanced multidetector computed tomograms were examined for the presence of obstructive coronary luminal narrowing in all available segments. The MDCT angiograms were examined using axial slices, curved multiplanar reconstructions, and maximum intensity projections (Figure). Coronary arteries were divided into 17 segments based on modified recommendations of the American Heart Association.11 Each vessel was analyzed on at least 2 planes, 1 parallel and 1 perpendicular to the course of the vessel. Semiquantitative assessment was performed on all segments of the coronary artery tree, with an estimate of stenosis severity calculated as the ratio of the minimum contrast lumen over the normal reference lumen of an unaffected distal portion. Severe coronary stenosis was defined as reduction > 70% of the lumen diameter, moderate as a reduction of 50% to 70% of the lumen diameter, and mild as a reduction < 50% of the lumen diameter. Scans were analyzed through consensus of an experienced radiologist and a cardiologist, who were both blinded to the clinical history. Discrepancies were resolved after additional joint review and discussion.
Statistical AnalysisContinuous variables are presented as mean ± standard deviation. Categorical data are presented as absolute frequencies and percentages. The normality of the distribution of variables was examined using the Kolmogorov-Smirnov test. Differences between groups were analyzed using the Student t test for continuous variables or the chi-square test for categorical variables. The sensitivity, specificity, positive predictive value, and negative predictive value of MDCT was analyzed on a per-segment, per-vessel, and per-patient basis. The kappa index was used to assess the agreement between MDCT and ICA. The chi-square test was used to assess differences in the agreement of MDCT and ICA between vessels. Conditional logistic regression analysis was used to analyze the impact of CS (as a quantitative variable) on the agreement between MDCT and ICA (as a qualitative variable: yes or no), including in this analysis the 484 segments with coronary stenosis. The diagnostic accuracy of MDCT compared with that of ICA was determined on a per-segment, per-vessel, and per-patient basis. To assess the effect of observer variability and reproducibility, a second independent observer analyzed 50 randomly selected segments. Intraobserver variability was assessed by comparing the measurements given by the same observer after an interval of more than a week between the 2 measurements. Both readers were blinded to previous measurements. A 2-tailed P < .05 was considered statistically significant. All statistical analyses were performed using SPSS version 17.0 (SPSS Inc, Chicago, Illinois, United States).
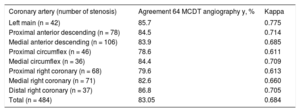
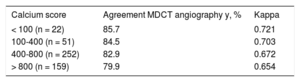
RESULTSThe mean age of the patients was 65.4 ± 11.2 years, and 188 (70.7%) were men. All MDCT examinations were performed without complications. The estimated average effective radiation exposure was 1.3 ± 0.5 mSv for CS and 10.2 ± 4.3 mSv for MDCT coronary angiography. The mean effective dose of prospective ECG-gated scans was 4.5 ± 2.3 mSv. Total CS for the 266 patients ranged from 0 to 1623.1 and the average CS was 916.0 ± 376. A total of 484 segments with coronary stenosis ≥ mild were qualitatively evaluated and quantified with MDCT. Noninvasive measurements were concordant with ICA in 402 stenoses (83.05%, kappa = 0.684), and discordant in 82 stenosis. Of these 82 stenoses, 15 (18%) were due to heavy calcification, preventing proper display of the lumen. No significant differences were found between vessels in the agreement of MDCT and ICA (P = .29 in chi-square test, Table 1). The average CS was 885 ± 312 in cases with agreement of MDCT and ICA and was 1068 ± 396 in cases without agreement, with no significant differences in the Student t test, P = .22). No significant influence of CS (as a quantitative variable) in the agreement of MDCT and ICA (as a qualitative variable: yes or no) was demonstrated in the conditional logistic regression analysis (n = 484, OR, 0.93; 95%CI, 0.76-1.09; P = .21). Table 2 shows the agreement between MCDT and ICA stratified by the CS groups. CS slightly influenced the agreement of MDCT and ICA, but no statistically significant difference was demonstrated in the 4 CS groups (P = .18). On a per-segment basis, the sensitivity, specificity, positive predictive value, and negative predictive value of multislice computed tomography angiography were 96.5%, 77.7%, 90.3%, and 95.3%, respectively; on a per-vessel basis, these values were 97.8%, 75.3%, 89.6%, and 96.4%, respectively; on a per-patient basis, these values were 98.8%, 74.6%, 88.8%, and 97.6%, respectively. Good intra- and interobserver agreement for MDCT were obtained, with intraclass correlation coefficients of 0.95 and 0.91, respectively.
Agreement Between MDCT and ICA Depending on the Vessel. Chi-square Test Showed no Significant Differences Between Vessels in this Agreement (P = .29)
| Coronary artery (number of stenosis) | Agreement 64 MCDT angiography y, % | Kappa |
|---|---|---|
| Left main (n = 42) | 85.7 | 0.775 |
| Proximal anterior descending (n = 78) | 84.5 | 0.714 |
| Medial anterior descending (n = 106) | 83.9 | 0.685 |
| Proximal circumflex (n = 46) | 78.6 | 0.611 |
| Medial circumflex (n = 36) | 84.4 | 0.709 |
| Proximal right coronary (n = 68) | 79.6 | 0.613 |
| Medial right coronary (n = 71) | 82.6 | 0.660 |
| Distal right coronary (n = 37) | 86.8 | 0.705 |
| Total (n = 484) | 83.05 | 0.684 |
ICA, invasive coronary angiography; MDCT, multidetector computed tomography.
Agreement Between MDCT and ICA Depending on the Groups of CS. Chi-square Test Showed no Significant Differences Between Groups of CS in This Agreement (P = .18)
| Calcium score | Agreement MDCT angiography y, % | Kappa |
|---|---|---|
| < 100 (n = 22) | 85.7 | 0.721 |
| 100-400 (n = 51) | 84.5 | 0.703 |
| 400-800 (n = 252) | 82.9 | 0.672 |
| > 800 (n = 159) | 79.9 | 0.654 |
CS, calcium score; ICA, invasive coronary angiography; MDCT, multidetector computed tomography.
The main findings of the present study are that non-ICA using 64-slice MDCT has good agreement with ICA in the qualitative quantification of CS with no significant differences between vessels, and CS has no significant impact on this agreement. This study has important clinical implications, and based on our findings, MDCT could be performed in patients with high CS using current technology.
Coronary artery calcium is closely correlated with atherosclerotic plaque formation and is thus a sensitive marker of existing atherosclerosis.12–15 A number of studies have confirmed that CS is a highly sensitive test for coronary atherosclerotic plaque and for “significant” coronary lumen disease with a high negative predictive value.16–19 CS has been shown to be predictive of major cardiovascular events and to modify the cardiovascular risk predicted by the Framingham risk score, especially in the intermediate risk group.20–23 CS may be useful in helping to determine which patients would benefit most from pharmacologic therapy, such as cholesterol-lowering medication. In our study, traditional cardiovascular risk factors were not predictors of calcium scores. This finding could explain the finding that the predictive value of CS for major cardiovascular events was superior to traditional cardiovascular risk factors. CS has some additional advantages; it takes approximately 5minutes to perform and interpret, is measured without contrast, and is a low radiation scan.24,25
The presence of calcium causes problems in the correct interpretation of MDCT coronary angiography. Calcium creates blooming artifacts, which obscure the visualization of the underlying noncalcified plaque or lumen. Calcium tends to overestimate the severity of adjacent lesions, either because of the blooming effect itself or because, if there is doubt or fear of “missing” a significant stenosis, “defensive” scoring is performed. With the first generation of MDCT scanners, severe coronary calcifications have been recognized as an important factor hampering precise evaluation of coronary artery stenoses, thereby limiting diagnostic accuracy.26,27 At the same time, more extensive coronary calcification increases the likelihood that the patient has obstructive coronary artery disease.8,9 Advances in temporal and spatial resolution, especially the introduction of 64-slice MDCT, have enabled high-quality non-ICA. The newer scanners allow rapid scanning of the cardiac anatomy, require minimal patient cooperation (short breath hold), and have improved image quality (better spatial and temporal resolutions) and high diagnostic accuracy.28–32 However, the main objective of MDCT is not to replace ICA, and these diagnostic tools are complementary. Innovations in the scanning process may reduce the importance of calcium in the future. At present, there is no firm consensus on the extent of coronary calcification that precludes a technically adequate coronary MDCT angiogram. In addition, total CS is somewhat misleading, because calcium distributed along the entire coronary tree would make the interpretation of an MDCT examination relatively easy, whereas a single heavily calcified plaque would make interpretation doubtful. Coronary MDCT may yield useful information despite extensive coronary calcification, particularly in patients with low heart rates and a low-to-moderate body weight. Thus, the decision to proceed with coronary MDCT in the presence of a high coronary CS is taken by the attending physician.
LimitationsThe present study has certain limitations. First, it is a descriptive, retrospective study performed in a single center. Second, MDCT is limited to the anatomic visualization of stenosis and does not provide information as to the functional relevance of a lesion. Third, no quantitative coronary angiography was performed and the stenoses were semiquantitatively assessed with both ICA and MDCT. Furthermore, ICA was not performed systematically, but was based on the result of the MDCT, producing a bias. Thus, these results can only be taken into account in similar contexts to the present study. Conditional simple logistic regression analysis (used to analyze the impact of CS on the agreement between MDCT and ICA) does not rule out the possibility that the results are due to chance. In addition, there may be a lack of statistical power that may influence the results of the present study. The lack of ischemic correlates on stress testing limited the clinical relevance of the findings. We did not assess the pattern of calcium deposits in this study. Extensive arterial wall calcifications still impair vessel assessment, but no segment had to be excluded from the analysis. A general limitation for all scoring methods is that the overall calcium burden poorly reflects the distribution of calcifications within the coronary tree. A single large calcified plaque in a proximal vessel segment may be more deleterious for image interpretation than multiple small speckles widely distributed. Further studies are warranted to determine the evaluability of MDCT examinations with respect to distribution patterns and plaque morphology.
CONCLUSIONSThe present study demonstrates that non-ICA using 64-slice MDCT has good agreement with ICA in the qualitative quantification of coronary stenosis, with no significant impact of CS on this agreement. This study has important clinical implications and, based on our findings, MDCT could be performed in patients with high CS using current technology.
CONFLICTS OF INTERESTNone declared.
- –
With the first generations of MDCT scanners, severe coronary calcifications were recognized as an important factor hampering precise evaluation of coronary artery stenosis, thereby limiting diagnostic accuracy.
- –
Calcified plaques produce artifacts (blooming) that may affect the evaluation of luminal obstruction.
- –
The main findings of the present study are that non-ICA using 64-slice MDCT has good agreement with ICA in the qualitative quantification of coronary stenosis, and CS has no significant impact on this agreement.
- –
This study has important clinical implications and, based on our findings, MDCT could be performed in patients with high CS using current technology.
.