This article reviews the updated European Resuscitation Council (ERC) Guidelines for Resuscitation 2015.1 These guidelines do not define the only way to perform resuscitation, but only offer an opinion based on an extensive review of the limited literature in this field.
ORGANIZATIONAL ISSUESFor the first time, emphasis has been placed on the importance of the contribution of the emergency medical dispatcher (112/061) to facilitate the early initiation of basic life support (BLS) maneuvers by bystanders who are trained in dealing with cardiac arrest (CA) (Figure 1 and Figure 2).
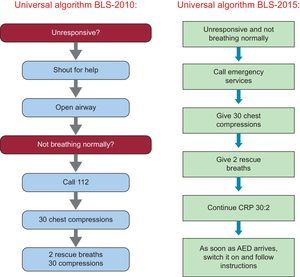
The BLS sequence in adults remains unchanged. The smallest change introduced in the adult BLS algorithm is the removal of the “Asking for help” step, which followed the confirmation of the state of unconsciousness in previous guidelines, and the merging of two questions into one: “Unresponsive and not breathing normally?” (Figure 3). This reflects the trend to simplify the guidelines and the need to minimize as much as possible the time spent on identifying a sudden death situation.2 The guidelines also highlight the need to suspect CA in any patient presenting with seizures.
In the absence of sufficient scientific evidence, they continue to stress the desirability of teaching rescue breaths and performing them in combination with chest compressions, whenever possible.
In addition to the early activation of all the links in the chain of survival, high-quality cardiopulmonary resuscitation (CPR) remains a key objective to improve survival in sudden death. In this regard, the current guidelines establish chest compressions of optimal depth in adults at 5 to 6cm with a rate of 100 to 120 compressions per minute, allowing the chest to rise completely after each compression and minimizing interruptions.
Regarding the implications of these new guidelines for clinical practice in Spain, special attention should be paid to the standardization of regulations in the use of automated external defibrillators (AED) across all the autonomous communities.
ADVANCED LIFE SUPPORTTwo aspects of the 2010 guidelines have been changed: a separate electrical therapies section has been eliminated and a new postresuscitation care section has been added.3
There is also continued emphasis on the prevention of in-hospital CA in all hospitalized patients as well as the need for a structured system to identify seriously ill patients. Measures for the prevention of CA in inpatients and outpatients have been revised. Attention is drawn to the universal termination of resuscitation rule, which recommends termination in the presence of nonshockable rhythm, if there is no return of spontaneous circulation (ROSC), unwitnessed CA, lack of CPR by bystanders, long response times by emergency teams, and patient characteristics.4
The guidelines include the advanced life support algorithm, which is almost identical to that of 2010. A section has been added indicating that the rescuer should consider using ultrasound imaging, mechanical chest compression devices, coronary angiography and percutaneous coronary intervention, and extracorporeal CPR.
The importance of assessing clinical signs and the use of waveform capnography is emphasized when monitoring during advanced life support. The defibrillation section highlights the need for self-adhesive patches for manual defibrillation, the use of an initial energy dose of 150 J to 200 J, preferably using biphasic waveform defibrillators, and the need to escalate the energy dose if successive discharges are required.
Regarding airway management, a stepwise approach based on patient factors and the skill of the rescuer is recommended. The use of adrenaline during CPR is still recommended, although it is noted that there is continuing strong debate regarding its role. Vasopressin is not recommended, and there is no evidence for routinely giving other drugs, such as steroids, magnesium, calcium, and sodium bicarbonate during CA. Fibrinolysis and the use of extracorporeal membrane oxygenators may have a role as a rescue therapy in selected patients. The routine use of mechanical chest compression devices is not recommended, except in selected cases.
Finally, the ERC highlights the importance of the ABCDE approach (A: airway; B: breathing; C: circulation; D: disability; E: exposure) in periarrest situations as an assessment tool.
Regarding the implications of these new guidelines for clinical practice in Spain, we emphasize the prevention of in-hospital CA, the implementation of in-hospital structured communication, the need for the incorporation of ultrasound imaging as a diagnostic tool, and the use of capnography as a monitoring tool.
CARDIAC ARREST IN SPECIAL CIRCUMSTANCESThe guidelines include 3 new sections under this heading: special causes, special environments, and special patients.
Special CausesThe special causes known as 4H (hypoxia; hypo/hyperkalemia; hypo/hyperthermia; and hypovolemia) and 4T (tension pneumothorax; cardiac tamponade; thrombosis; toxins) have been revised.
The main innovations comprise a new treatment algorithm for life-threatening hyperkalemia, a specific treatment algorithm for anaphylaxis that emphasizes early treatment with intramuscular adrenaline, and a treatment algorithm for traumatic CA with explicit indications for immediate resuscitative thoracotomy (CA caused by blunt trauma that does not respond to CPR within 10minutes or CA caused by penetrating trauma that does not respond to CPR within 15minutes).
The hypo/hyperthermia section recommends noninvasive rewarming techniques in the absence of hemodynamic instability; in the presence of instability, the patient should be treated with extracorporeal life support. The new guidelines on CPR in the case of hypothermia recommend intubation without delay, and echocardiography and ultrasound imaging to verify cardiac activity and blood flow. The use of mechanical chest compression should be considered (given potential chest tightness), as well as the use of low-reading thermometers. Drugs and defibrillation should not be used until a body temperature equal to or more than 30°C has been achieved. If used, adrenaline should be administered at intervals of 6 to 10minutes.
Special EnvironmentsThe special environments section recommends using the universal advanced life support algorithm, with some modifications according to the setting in which CA occurs.
- 1.
In specialized healthcare facilities. The guidelines include a section on CA following cardiac surgery; early thoracotomy should be performed if cardiac tamponade is suspected. When CA occurs in the cardiac catheterization laboratory during percutaneous coronary intervention, 3 shocks should be administered in tandem in the case of ventricular fibrillation and, if needed, a mechanical chest compression device should be used.
- 2.
In transportation vehicles. This section refers to commercial aircraft; it is recommended that an AED is available.5
The guidelines review the special characteristics of patients who are pregnant, elderly, or who have a serious comorbidity, such as asthma, heart failure with a ventricular assist device, acute neurological disease, and obesity.
Regarding the implications of these new guidelines for clinical practice in Spain, we stress the need for the incorporation of ultrasound imaging as a diagnostic tool in the management of CA, the need for the greater availability of AEDs in different environments, and the need for appropriate resuscitation equipment in settings in which there is a risk of CA.
POSTRESUSCITATION CAREInnovationsGreater emphasis is placed on the need for percutaneous coronary intervention following out-of-hospital CA of likely cardiac cause.6
There is now an option to target a temperature of 36°C instead of the previously recommended 32°C to 34°C. The prevention of fever continues to be emphasized.7
A multimodal approach is recommended to assess prognosis. Emphasis has been placed on allowing sufficient time for neurological recovery and for sedatives to be cleared, which can be prolonged in patients with hypothermia.
The systematic organization of follow-up care is recommended, which should include screening for potential cognitive and emotional disturbances.
Contentious IssuesAlthough the guidelines recommend the GRADE approach to assess the quality of evidence and strength of recommendations, most of these were not graded except for targeted temperature management.7,8
Regarding neurological outcomes, the main problem resides in the validation of the recommended biomarkers, because most studies have included few patients. In addition, many of these studies suffered the bias of the self-fulfilling prophecy, because the physician who made the decision to limit treatment (removal of life support) was not blinded to the results of these markers.
The recommendations of these guidelines should lead to the creation of specialized CA care centers. The minimum requirements for these centers would be the capacity for immediate cardiac catheterization and for body temperature control. It would also be useful if they were equipped with the means for accurate prognostic stratification and a specific postdischarge support and rehabilitation system. Ideally, patients in whom resuscitation fails or life support is withdrawn should be included in organ donor programs, including donation after cardiac death. A unit should be available to screen potential donors for hereditary diseases for their prevention in family members. The foregoing innovations should be complemented by the creation of referral networks to optimize outcomes and resources at these centers.
PEDIATRIC LIFE SUPPORTInnovationsBasic life support- •
The duration of delivering a breath should be about 1 second, to coincide with adult practice.
- •
For chest compressions, the lower sternum should be depressed by at least one third of the anterior-posterior diameter of the chest (4cm in infants and 5cm in children).
- •
If there are no signs of septic shock, children with a febrile illness should receive fluids with caution and be reassessed after their administration. In some forms of septic shock, restricting fluids with isotonic crystalloid fluids may be more beneficial than the liberal use of fluids.
- •
The initial energy dose for cardioversion of a supraventricular tachycardia has been changed to 1 J/Kg.
- •
Many features are common with adult practice.
- •
Prevent fever in children who have ROSC in an out-of-hospital setting.
- •
Targeted temperature management in children post-ROSC should comprise either normothermia or mild hypothermia.
- •
There is no single predictor for when to stop resuscitation.
Changes have been introduced based on scientific evidence. In its absence, the teaching of resuscitation in children has been made easier, either by avoiding changes without sufficient support, or by teaching those who have learned CRP only in adults.
Contentious IssuesRegarding the sequence for maneuvers in BLS the CAB sequence and the ABC sequence were found to be equivalent.9 Given that respiratory arrest is more common than CA in children, and that the ABC sequence has become an established method to teach CPR in Europe, the use of this sequence should be maintained. This position is different outside Europe and will continue to be reviewed on the basis of any forthcoming scientific evidence.
Implications for Clinical Practice in SpainThe presence of a first responder is associated with better neurological outcome in adults and children.10 The crucial role of the first responder could be supported through the mass teaching of CRP, which could be implemented via the school curriculum.
NEONATAL RESUSCITATIONThe concept of resuscitation should be distinguished from the concept of support during the transition period. The term “support of transition” has been introduced to distinguish between situations in which maneuvers are needed to restore vital organ functions and those in which medical help is needed to support transition.
Cord ClampingAccording to the 2015 guidelines of the International Liaison Committee on Resuscitation (ILCOR), it seems reasonable to delay cord clamping for more than 30seconds in full-term and premature neonates requiring resuscitation at birth. There are insufficient data to recommend a clamping time in neonates who need resuscitation at birth. In neonates of less than 29 weeks of gestation, umbilical cord milking continues to be recommended because it can raise the initial blood pressure, improve specific hematological indices, and reduce intracranial hemorrhage; however, no data are available on its favorable long-term effects.
Temperature ControlHypothermia at birth has been associated with various adverse effects; preterm infants are especially vulnerable. The temperature of newly born nonasphyxiated infants should be maintained between 36.5°C and 37.5°C.
Management of MeconiumThe guidelines emphasize the need to initiate ventilation within the first minute of life in nonbreathing infants or ineffectively breathing infants. Tracheal intubation and suctioning should not be routine and should only be performed for suspected tracheal obstruction on an individual basis.
Assessment of Heart RateThe heart rate in the first minute of life is best assessed by using an electrocardiograph and should be recommended vs a pulse oximeter.
Oxygen AdministrationIn term infants, resuscitation should start with air (FiO2 [fraction of inspired oxygen] 21%). Subsequently, if required, a higher concentration of oxygen guided by oximetry can be used to achieve an adequate preductal SaO2 (arterial oxygen saturation) to approximate the percentile of a healthy neonate after vaginal delivery at sea level. Resuscitation of preterm infants less than 35 weeks gestation at birth should be initiated with an FiO2 of 21% to 30%. Oxygen administration should be titrated with monitoring to achieve acceptable preductal SaO2.
Positive Pressure VentilationThe 2015 ILCOR guidelines on the use of positive end expiration pressure are similar to those of 2010. A positive end expiratory pressure of 5 cmH2O should be used when positive pressure ventilation is being administered. Premature neonates of less than 30 weeks gestation with spontaneous breathing and respiratory distress can be treated with continuous positive airway pressure rather than routine intubation.
INITIAL TREATMENT OF ACUTE CORONARY SYNDROMEReperfusion decisions in patients with ROSC following CA of suspected cardiac origin with ST-segment elevation acute myocardial infarction on electrocardiogram are similar to those in patients with ST-segment elevation acute myocardial infarction without CA. However, there is considerable controversy concerning non—ST-segment elevation acute coronary syndromes patients, because the sensitivity and specificity of clinical data, electrocardiogram, and even biomarkers to predict an acute coronary artery occlusion as the cause of CA are unclear. According to the guidelines, it is reasonable to consider emergent cardiac catheterization laboratory evaluation in patients with the highest risk of a coronary cause of CA. This recommendation is based on several observational studies showing that it is often possible to identify an acute thrombotic coronary disease even in patients with CA and without ST-segment elevation on ECG.11 However, there are conflicting data on the potential benefit of performing an emergent or urgent coronary angiography in this setting.
FIRST AIDThe 2015 ERC guidelines include a new section on first aid, which begins with a definition of what is meant by first aid and its aims. The new section is divided into 2 parts: first aid for medical emergencies and first aid for trauma emergencies.
There is a lack of robust scientific evidence on first aid, and so many of the suggestions are based on medical expert consensus.
EDUCATION IN RESUSCITATIONThe 2015 ERC guidelines dedicate a specific section to education in basic life support as well as its implementation.
InnovationsThe use of high-fidelity manikins is recommended, but low-fidelity manikins can be used at all levels of ERC life support training. Cardiopulmonary resuscitation feedback devices are useful to improve compression rate, compression depth, decompression, and hand position.
Refresher courses in CPR should consist in short-burst training and their frequency should be adapted to the characteristics of the participants (lay or medical).
Basic life support courses should incorporate training in nontechnical skills (communication, leadership, etc).
Emergency medical dispatchers require specific training in guiding untrained rescuers on how to perform CPR.
The use of all new technology (mobile devices, social media, etc) is considered useful to improve CPR or to access an AED.
Other Aspects of EducationUsing technology and social media: Mobile devices can incorporate informative, educational, and interactive applications (AED geolocation, feedback on the quality of the maneuvers, etc), which can be useful tools to improve education in CRP. In addition, social media are a powerful means of disseminating information and raising awareness on CRP.
Measuring performance of resuscitation systems and debriefing in the clinical setting: Measuring the performance of resuscitation systems and teams is essential to implementing quality improvement initiatives. Critical feedback on performance in real clinical situations is of value to ensure continuous improvement.
Medical emergency teams: Early recognition of the deteriorating patient is the first link in the chain of survival for CA. The establishment and training of rapid-response medical emergency teams is recommended because they have been associated with a reduced incidence of CA. Hospital staff should receive training on signs of patient deterioration, appropriate monitoring, and criteria for activating the teams and how they should be activated.
Emergency medical dispatchers: Dispatchers are part of the first link in the chain of survival and face specific difficulties. They should receive additional training in interpreting signs and symptoms, with a special emphasis on verbal communication.
Contentious Issues to Be ResolvedEvidence has begun to emerge that brief frequent simulation training is useful for maintaining knowledge and skills in resuscitation, but further studies are needed to confirm this.
The use of audiovisual feedback devices to acquire technical skills in chest compressions may be detrimental, because they tend to focus attention on the rate of chest compressions rather than on their quality.
No particular CRP training method can be recommended because of the lack of comparative studies.
No data are available on the retention time of theoretical information and skills acquired following CPR training. It appears that CPR skills begin to decay 3 months after training. Currently, it is recommended that refresher courses should be taken every 1 to 2 years.
THE ETHICS OF RESUSCITATION AND END-OF-LIFE DECISIONSThe main innovation is a shift from the traditional approach of focusing on medical aspects, with an emphasis on the principle of beneficence, to a patient-centered approach with more emphasis on the principle of autonomy. Thus, it is essential that the provision of information and interaction is appropriate between healthcare professionals and surviving patients and their families. The guidelines have adapted the traditional ethical principles (autonomy, beneficence, nonmaleficence, and justice) to this new approach.
One of the most controversial aspects is related to decisions to suspend CRP. The decision to suspend CRP is particularly difficult, since there are no single predictor variables for establishing prognosis, and thus decisions should not be based on a single parameter, such as age.
CONCLUSIONSThese new guidelines represent advances in knowledge over the past 5 years. Their most novel aspect may reside in the emphasis on the need to teach citizens the initial management of CA.
CONFLICTS OF INTERESTI. Fernández Lozano has received payments for consulting and conferences, and grants for attending congresses from Bayer, Boston Scientific, and St. Jude Medical. I. Manrique has received payments for consulting and conferences, and grants for conference attendance from Nestlé laboratories Spain and Ordesa. A. Sionis has received payments for consulting and conferences, and grants for conference attendance from AstraZeneca, Bayer, Boehringer, Daiichi-Sankyo, Ferrer, Maquet, Menarini, Novartis, Orion-Pharma, Pfizer, and Servier.