To the Editor,
A previously asymptomatic 78-year-old woman was admitted because of dyspnea and a sense of fainting when moving from the recumbent to the erect position. When supine the patient was not dyspneic and on clinical examination a soft basal diastolic murmur was heard. Arterial blood oxygenation on room air was 95%. On standing up, she became tachypneic and cyanotic, with a blood desaturation to 84%, not responding to supplemental oxygen. The presence of a platypnea-orthodeoxia syndrome (POS) was evident, while signs of orthostatic hypotension were absent. The electrocardiogram was normal. Chest radiography showed an enlarged and tortuous thoracic aorta.
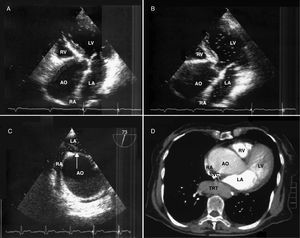
A transthoracic echocardiogram revealed normal ventricles and left atrium. A dilated ascending aorta of 6.0cm was distorting and severely reducing the right atrium (Figure 1A). Slight aortic and tricuspid valve regurgitations were noticed. Systolic pulmonary artery pressure was estimated at 35mmHg. When agitated saline was injected intravenously in a seated position, microbubbles appeared immediately in the left atrium, confirming the existence of a right to left intracardiac shunt (Figure 1B). With the patient in the recumbent position, the quantity of bubbles passing to the left cardiac chambers was dramatically reduced. The location of the shunt was not apparent transthoracically, but transesophageally a patent foramen ovale (PFO) of 5mm was found and the amount of shunt was calculated at 25% (Figure 1C). Although the early appearance of contrast in the left atrium made the existence of an intrapulmonary fistula unlikely, a chest computerized tomography (CT) and magnetic resonance imaging were deemed necessary. In particular, chest CT showed the aortic aneurysm severely deforming the right atrium to a vermiform cavity (Figure 1D). No signs of intrapulmonary arteriovenous malformations were found. The patient was referred for resection and grafting of the ascending aortic aneurysm, with closure of the PFO. Unfortunately, the planned interventions were cancelled 10days later, when the patient sustained a hemorrhagic stroke.
Figure 1. Transthoracic echocardiogram, modified apical view. Right atrium is compressed by ascending aorta (A). Contrast passes through the right atrium to the left (B). Transesophageal echocardiogram. Right atrium deformed by the dilated aorta. Opening of a patent foramen ovale (arrow) permits a right-to-left shunt of contrast (C). Chest computerized tomography. Right atrium reduced by the aortic aneurysm to a vermiform cavity (D). AO, ascending aorta; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; SVC, superior vena cava; TRT, tortuous descending aorta.
A POS consists of dyspnea and arterial oxygen desaturation when assuming the sitting or erect position from the recumbent one.1 A right-to-left interatrial shunt through a PFO is frequently the anatomical substrate that is responsible.2, 3 Persistence of a PFO in adulthood reaches a prevalence of almost 25%, usually remaining clinically silent. If right atrial pressure exceeds the left one, a right-to-left interatrial shunt can manifest paradoxical embolisms or POS, sometimes provoking cryptogenic strokes. Alternatively it can present even in the absence of elevated right atrial pressure. This is a case of a position- and not a pressure-mediated shunt. An enlarged ascending aorta can distort the right atrium, giving a horizontal direction to the atrial septum and a counterclockwise rotation of the heart.4, 5 This distortion favors a caval inflow against a PFO, especially in the sitting and erect position, when the postural changes may exacerbate a right-to-left shunt.6
As life expectancy is increasing, aortic dilatation will become more common. When elderly patients present with otherwise unexplained dyspnea, positional manipulations should be performed. If the suspicion of POS is raised, the possibility of an aneurysmatic ascending aorta distorting a previously silent PFO should not be overlooked.
Corresponding author: sarvanitakis@doctors.net.uk