Keywords
INTRODUCTION
Diabetes mellitus (DM) is one of the diseases of greatest public health impact in Spain. Its high prevalence and association with cardiovascular complications1,2 makes it a serious burden on the country's public health system; indeed, DM management consumes some 14% of Spain's annual health expenditure.3
Over the last 20 years there has been a spectacular increase in the number of people who are overweight and who suffer DM in Western countries; this has been mainly attributed to changes in lifestyle. It is currently believed that some 10%-19% of the Spanish population is diabetic, among which fraction 90% are believed to have DM type 2 (DM2). The incidence of DM2 is now greater than 10 cases per 1000 inhabitants per year; thus, the number of diabetics is likely to double in the next 25 years.4-8
In the long term, hyperglycemia is associated with microangiopathy, neuropathy, and macrovascular complications, problems that are more prevalent among patients with abnormal glucose metabolism even before the appearance of diabetes.9-12
Cardiovascular diseases are the main cause of morbidity/mortality among diabetics. Compared to members of the normal population of the same age, diabetics are at a 2-4-fold greater risk of ischemic cardiomyopathy (IC),13-17 cerebrovascular disease (CVD),18-21 and death due to these causes. Although peripheral vascular disease (PVD) is uncommon in the early years of suffering diabetes, it is 4-5 times more prevalent in patients with advanced disease than among the non-diabetic population.23 Further, IC accounts for more than 50% of total mortality among diabetics.24
Patients with diabetes who have suffered some cardiovascular complication are at a greater risk of associated morbidity and mortality than those who have suffered no such complication. The clinico-epidemiological research undertaken to date on diabetics with cardiovascular disease has been limited mostly to those with IC25; very little information is available regarding the prognosis of those with CVD or PVD.
Differences have, nonetheless, been described in risk factor profiles depending on the area in which atherothrombotic disease is clinically manifested.26,27
Thus, the risk of new vascular complications may vary in diabetics with IC, CVD, or PVD. However, very little information is available regarding the prognosis of diabetics with different degrees of cardiovascular involvement (expressed as the number of vascular areas with a documented systematic complication); in Spain there is practically no information available at all.
The main aim of this prospective study (the Barbanza Diabetes study) was to quantify and compare the influence of a clinical background of atherothrombotic disease manifested as IC, CVD, or PVD on the risk of new vascular complications in a homogeneous cohort of patients with diabetes. A further aim was to define the pattern of cardiovascular disease in diabetic patients with and without clinical manifestations of such disease.
METHODS
Study Protocol
This prospective, multi-center cohort study (some of the characteristics of which have been described in a previous paper)28 involved 31 primary care doctors belonging to 10 health centers in the southeast of the province of A Coruña, in northwestern Spain. The initial study population was composed of 1423 consecutive eligible patients who came for consultation over a period of 2 months in 2002. The inclusion criteria were: age >18 years, a previous diagnosis of DM,29 and the provision of consent to be included in the study. A prospective follow-up period lasting 4 years was planned, with 3 appointments to monitor risk factors and treatment. A total of 109 patients were lost to follow-up, 83 because of a change of workplace of 2 of the participating doctors, and 26 because of changes in patient address. All data were internally audited after their collection to ensure their quality.
Variables Analyzed
All patients were subjected to anamnesis, a physical examination, and biochemical and electrocardiographic (ECG) tests. Patient demographic, anthropometric, and clinical characteristics were also recorded, as was the treatment each patient was prescribed.
Patients with a body mass index (BMI) of ≥30 were considered to be obese. Blood pressure was measured on the day of inclusion using a checked, calibrated sphygmomanometer. After a 5 min rest period a first reading was taken, followed by a second reading 5 min later. The mean result was then calculated; a value of <130/80 mm Hg was taken to reflect good control of blood pressure. A baseline fasting blood sugar level of <126 mg/dL and a glycohemoglobin level of <7% were considered to represent good control of these variables, as were values of <50 mg/dL for triglycerides, <180 mg/dL for total cholesterol, and <100 mg/dL for low density lipoprotein cholesterol (LDL-C). In women, high density lipoprotein cholesterol (HDL-C) was considered under control when values of >50 mg/dL were recorded; in men, >40 mg/dL was considered satisfactory. The normality value for albuminuria was taken as >30 mg/dL/24 h.
After the 4 years of follow-up, the mortality data collected were analyzed, taking into account the cause of death. Morbidity data were also analyzed, taking into account admissions to hospital and the reason for such admission. The cause of death was obtained from the corresponding death certificate, and the reason for hospitalization from hospital release records; these documents were available in the medical histories of the patients stored at the health centers.
The patients were grouped depending on whether or not they suffered cardiovascular disease (divided into IC, CVD or PVD, or atherothrombotic events in more than 1 area) prior to their inclusion in the study. The IC group included patients with a prior diagnosis of angina or myocardial infarction or who had undergone a coronary revascularization procedure (percutaneous or/and surgical). The CVD group included patients with a prior diagnosis of ictus or transitory ischemic attack. The PVD group included patients with a diagnosis of intermittent claudication or aneurysm of the abdominal aorta, or who had undergone a revascularization procedure in the lower limbs (percutaneous or/and surgical) or abdominal aorta surgery.
Statistical Analysis
Qualitative variables were expressed as absolute frequencies and percentages. Quantitative variables were expressed as means (standard deviation). A descriptive analysis of the categorical variables was performed using frequency tables. The Pearson c2 test was used to determine the significance of differences between qualitative variables. Means were compared using the Student t test for independent samples.
The probability of survival during follow-up was determined using the Kaplan-Meier test, employing the logarithmic rank test to compare the curves of different subgroups of patients. Variables found to be significant in univariate analysis were included in Cox multivariate analysis (forward stepwise conditional method). The variables that maintained significance (age, sex, blood pressure, prior cardiovascular disease, and treatment with diuretics, beta-blockers, angiotensin converting enzyme inhibitors [ACEi], nitrates, and angiotensin II receptor antagonists [ARA II]) were those that were finally used to adjust the model. The results are expressed as hazard ratios (HR) and 95% confidence intervals (95% CI). All calculations were performed using SPSS v.14.0. software for Windows. Significance for was set at P<.05 for differences with a probable type I error.
RESULTS
Characteristics of the Patients Studied
Of the 1423 patients initially included, 8% had DM type 1 (DM1). Half of the patients were male; the mean age of the patients was 66 (11) years (age range, 18-97 years). The mean age of the male patients was significantly higher than that of the female patients. Some 47% of the patients studied were obese, 70% showed dyslipidemia, and more than half had some cardiovascular disease or a lesion in another organ. All the risk factors studied, except for smoking, were more common among the female patients, while the males showed a greater actual presence of cardiovascular disease or lesions in other organs (58% compared to 45%; P<.001). Table 1 shows the characteristics of the patients and their treatment depending on whether they had cardiovascular disease or not. Those with cardiovascular disease were older and more frequently showed evidence of kidney damage (albuminuria). The prevalence of high blood pressure was high in all cardiovascular disease subgroups. Some 72.6% of the patients received monotherapy for their diabetes; only 4% took 3 or more medications. Some 19.5% received insulin; 25% of the patients with cardiovascular disease were administered insulin. A strong relationship was seen between high blood pressure and treatment with diuretics; 29.1% of patients who were hypertensive received these drugs compared to only 4.8% of those who were not (P<.001).
Table 2 shows that blood pressure was well controlled in only 14% of hypertensive patients, and baseline glycemia was adequate in only 22%. The patients with IC showed better control of their blood pressure and plasma lipids than did those of the other subgroups. No significant differences were seen with respect to carbohydrate metabolism variables.
Mortality and Morbidity
After a mean follow-up time of 44.6 (10.2) months (median, 48.1 months), total mortality had reached 6.2%. Some 49% of deaths had a cardiovascular cause. The hospitalization rate reached 30%. Table 3 shows the mortality and hospitalization rates plus their associated causes for the subjects as a whole and depending upon whether or not they suffered cardiovascular disease. Mortality was higher in patients with cardiovascular disease, among whom death due to cardiovascular cause was more common. The combination of death + hospitalization for cardiovascular reasons was significantly more common in the subgroups of patients with cardiovascular disease than in the group with no cardiovascular disease. In this latter group, the most common reasons for hospitalization were non-cardiovascular (unlike in the cardiovascular disease subgroups).
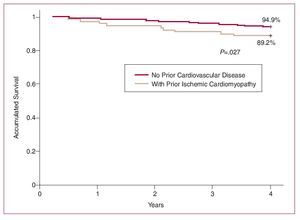
The actuarial probability of survival at 4 years was 93.8%. The Kaplan-Meier curves of Figure 1 show that the probability of survival was significantly lower for those patients with a prior diagnosis of IC than for patients with no cardiovascular disease.
Figure 1. Probability of survival of patients in the Diabetes Barbanza study.
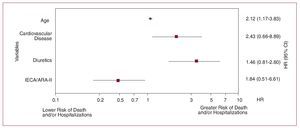
Multivariate analysis showed age, the suffering of cardiovascular disease, and treatment with diuretics to be independent predictors of mortality; treatment with ACEi and/or ARA-II was found to be protective (Figure 2).
Figure 2. Cox regression. Determinants of mortality adjusted for age, sex, high blood pressure, prior cardiovascular disease, and treatment with diuretics, beta-blockers, nitrates, ACEi, and ARA-II. ACEi indicates angiotensin converting enzyme inhibitors; ARA-II, angiotensin II receptor antagonists II; HR, hazard ratio.
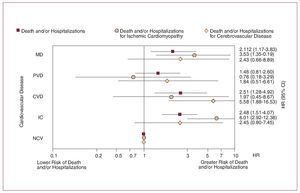
Table 4 and Figure 3 show that patients with a cardiovascular complication were at greater risk of suffering new events or death of cardiovascular cause than those who had no background of cardiovascular disease. The patients with IC were at greater risk of suffering a new cardiovascular event in the same area; similar results were found for patients with CVD.
Figura 3. Risk of events and death for different cardiovascular reasons (cardiovascular disease, ischemic cardiomyopathy, cerebrovascular disease), depending on whether patients suffered prior cardiovascular disease, adjusted for age, sex, high blood pressure, and treatment with diuretics, beta-blockers, nitrates, ACEi, and ARA-II.
DISCUSSION
The risk of suffering a cardiovascular event (death and/or hospitalization for a cardiovascular cause) was found to be similar in the patients with a prior diagnosis of IC, CVD, or PVD, and more than double that for patients with no evident clinical cardiovascular disease.
In the members of the IC subgroup, the most common place for the recurrence of clinical complications (death and/or a new event) was the coronary vascular area; in contrast, for those in the CVD subgroup, recurrences were more likely in the cerebrovascular area. The increased risk of ictus among the IC subgroup patients should also be noted.
To our knowledge, the Barbanza Diabetes study is the first to describe the mid-term (4 years) prognoses of the members of a homogeneous cohort of diabetics with and without clinical cardiovascular disease in Spain. The characteristics of this large group are those expected of a coastal population from Galicia (the region where the study was performed)—high blood pressure, a high salt intake, and a higher incidence of ictus than in Spain's other regions.30 In addition, the present study takes into account the different forms of atherothrombotic disease with which these patients presented.
A number of studies have analyzed the cardiovascular risk of diabetics with and without clinically important IC. Recently, the mid term prognosis (follow-up=3 years) of a group of 776 Dutch diabetics with and without evident cardiovascular disease (n=458 and 318 respectively) was investigated, and it was concluded that, compared to diabetic patients with no such disease, the risk of a new cardiovascular complication (cardiovascular death or non-fatal ischemic stroke or acute myocardial infarction [AMI]) was greater among those with IC, CVD or PVD (4.3, 3.8, and 4.6 times respectively).31 The risk of suffering cardiovascular complications during follow-up was greater among the patients of the present study, both for those with and without prior cardiovascular disease. However, it should be remembered that the Dutch cohort study only included mortality and non-fatal stroke or AMI while the present work included hospitalizations for all cardiovascular causes. It should also be noted that the risk observed for the Dutch cohort was only slightly greater than for the present IC and CVD subgroups, but more than double that recorded for the PVD subgroup. Differences in patient characteristics might account for these differences since the present study involved consecutive diabetic patients receiving assistance from primary care physicians, while the Dutch patients were diabetics referred for consultation to a university hospital. The differences in the recording of hospitalizations may also have led to these differences.
A study that investigated the 10 year prognosis of a group diabetic patients with cardiovascular disease (IC, CVD, or PVD) showed their risk of complications to be 6 times that of persons without diabetes or cardiovascular disease.32
ACEi indicates angiotensin converting enzyme inhibitors; ARA-II, angiotensin II receptor antagonists II; CVD, cerebrovascular disease; HR, hazard ratio; IC, ischemic cardiomyopathy; MD, multiple cardiovascular disease; NCV, no cardiovascular disease; PVD, peripheral vascular disease.
The present study describes the characteristics of recurrences in diabetic patients with different forms of clinical, atherothrombotic disease. While those with IC or CVD were at a greater risk of a recurrence of a clinical complication in the same area, it should be noted that the IC patients had a greater risk of suffering ictus than did the CVD patients of suffering a myocardial ischemic event. Although the small number of patients in each subgroups requires caution be used in the interpretation of these results, no other study has described the pattern of recurrence of cardiovascular disease in diabetics with a prior diagnosis of atherothrombotic disease. In agreement with the recommendations made in clinical guidelines, this indicates the need to look for asymptomatic vascular disease in other areas, especially CVD in patients with IC.33,34
The present results agree, to some extent, with those recorded in a large international registry (the REACH Registry). The latter includes the data of 68 236 patients with clinical IC, CVD, or PVD and of 12 422 patients at high cardiovascular risk (at least 3 risk factors for atherothrombosis) but with no clinical manifestation of disease. After a follow-up period of 1 year, recurrence in CVD and IC subgroup patients was found to be more common in the same vascular area. Some 5.3% of the patients with multiple cardiovascular risk factors, 15.2% of the IC patients, 14.5% of the CVD patients, and 21.1% of the PVD patients died of cardiovascular causes, suffered a non-fatal stroke or AMI, or required hospitalization for an atherothrombotic event.35
In the present study, age, prior cardiovascular disease and treatment with diuretics were independent predictors of mortality. The first 2 of these variables have also been identified as such in nearly all cardiovascular disease registries. The fact that treatment with diuretics should be a predictor probably reflects the influence of heart failure and the need to use more drugs to control more advanced high blood pressure.
It should be noted that treatment with ACEi and/or ARA-II had a protective effect. The same has been seen in a number of clinical trials (MicroHOPE,36 BENEDICT,37 IDNT,38 IRMA-II,39 RENAAL40) involving diabetics. The present data reinforce the recommendations to be found in current practice guidelines, which indicate the blocking of the renin-angiotensin system to be one of the pillars of the therapeutic strategy to be followed.
Limitations of the Study
The present study has the advantage that it involves a registry in which the physicians directly responsible for the patients make and record the diagnosis of DM, record the risk factors for any concomitant cardiovascular disease, record the characteristics of the treatment to be followed, and note the cardiovascular complications that arise during follow-up. However, more than 7% of the subjects were lost to follow-up. This may have had some influence on the results, although it is similar to that described in other population registries for cardiovascular diseases.
For the majority of patients, possible changes in the therapeutic strategy were never recorded. Along with the initial treatment provided, such changes could have influenced the prognosis. However, this is a limitation of nearly all registries on cardiovascular risk and disease.
It is possible that some patients may have suffered cardiovascular complications that did not require hospitalization, leading to the eventual undervaluation of cardiovascular risk.
Concluding a protective action for ACEi and ARA-II suffers from the methodological limitations associated with making clinical observations from registries, although a number of the clinical trials mentioned above vouch for their effect.
Finally, mortality may have been undervalued since patients lost to follow-up may have died.
CONCLUSIONS
This study, which investigates the mid-term prognosis of diabetic patients (from a single geographical area) with clinical cardiovascular disease (IC, CVD, or PVD), shows that cardiovascular mortality and morbidity are similar irrespective of the vascular area affected. The results reveal the recurrence of atherothrombotic disease in each subgroup to be more common in the same vascular area. Treatment with drugs designed to block the reninangiotensin system (ACEi and ARA-II) was found to be an independent predictor of improved prognosis; this should be interpreted with caution, however, since it is a finding associated with a patient registry rather than a clinical trial.
The present results highlight the importance of better implementation of the recommendations made in clinical guidelines, both in terms of diagnostic assessment and therapeutic practice.
Researchers of the Barbanza Group
J.M. Fernández-Villaverde, G. Allut-Vidal, J. Domínguez-López, J.L. Gómez-Vázquez, V. Parga-García, P. de Blas-Abad, C. Pastor-Benavent, A. Fernández-Seoane, R. de la Fuente-Mariño, J. Maestro-Saavedra, A. Ramos-González, M.J. Alvear-García, M.A. Pérez-Llamas, M.J. Eirís-Cambre, R. Besada-Gesto, C. de Frutos-de Marcos, M.C. Caneda-Vi-llar, J.A. Santos-Rodríguez, M. Lado-López, V. Turrado-Turrado, L. Vaamonde-Mosquera, A. Lado-Llerena, and A. Nores-Lorenzo.
ABBREVIATIONS
ACEi: angiotensin converting enzyme inhibitors
ARA-II: angiotensin II receptor antagonists
CVD: cerebrovascular disease
DM: diabetes mellitus
IC: ischemic cardiomyopathy
PVD: peripheral vascular disease
A full list of the participants in the Barbanza study is provided at the end of this article.
Correspondence: Dr. J.R. González-Juanatey.
Servicio de Cardiología. Hospital Clínico.
Travesía Choupana, s/n. 15706 Santiago de Compostela. A Coruña. España.
E-mail: jose.ramon.gonzalez.juanatey@sergas.es
Received January 15, 2008.
Accepted for publication July 15, 2008.