Keywords
INTRODUCTION
Cardiovascular disease is the main cause of premature death in most European populations.1 Total cardiovascular risk estimation is the first step needed to establish primary prevention measures. Cardiovascular risk can be readily calculated in certain subgroups of patients and those with several risk factors.2 Nevertheless, depending on the population studied, there are differences in the susceptibility to established risk factors and, therefore, in the accuracy of cardiovascular risk prediction.3-7
According to some authors, the classic cardiovascular risk factors such as smoking, hypertension, dyslipidemia, diabetes, obesity, sedentary lifestyle, and dietary factors do not completely explain the differences in the prevalence of cardiovascular disease between different populations.8-13 Additional markers such as triglyceride and fasting glucose levels may be of great help in risk stratification and improving treatment directed toward specific populations. Therefore, these may be considered "emerging risk factors."
Adiponectin is an adipocytokine secreted by adipocytes that regulates the body's energy metabolism by stimulating fatty acid oxidation, lowering plasma triglyceride levels, and improving glucose metabolism through an increase in insulin sensitivity.14 In several studies,15,16 hypoadiponectinemia has been observed in patients with obesity, diabetes mellitus, and coronary artery disease. In addition to its antidiabetogenic properties, adiponectin posses an antiatherogenic effect and shows an inverse relationship with other risk factors, such as blood pressure (BP), total cholesterol, and low-density lipoprotein concentrations.17-20 Cross-sectional population studies have shown that low concentrations of adiponectin are associated with an adverse risk profile.21,22 Because of the existing differences related to geographic location, it is important to determine the relationship between adiponectin concentrations and cardiovascular risk factors specifically for the Spanish population. To date, only one cross-sectional study in this regard has been performed in Spain, in the Mediterranean population of Catalonia.
The authors reported a relationship between low adiponectin concentrations and insulin resistance.23 Plasma adiponectin concentrations seem to show interpopulation variations, however, and this should be taken into account in larger studies.24
The aims of this study were to examine the correlation between plasma adiponectin concentrations and abdominal obesity in the Spanish population and investigate the relationship between certain emerging risk factors, such as abdominal obesity, and levels of adiponectin, triglycerides, glycosylated hemoglobin (HbA1c), high-sensitivity C-reactive protein (hsCRP), and fasting glucose, and the probability of experiencing a first cardiovascular event.
METHODS
Procedures
A cross-sectional, case-control study was undertaken in the population attended in the Spanish National Health Service, with the participation of 367 investigators from 170 centers. Subjects were recruited over approximately 4 months and enrolled consecutively; the investigator included the first 2 patients of cases and controls that fulfilled the selection criteria. Among 1160 patients included, 999 who came for outpatient consultation in the internal medicine, cardiology, or endocrinology departments were evaluated. The case group included 523 individuals who had a first cardiovascular event (ischemic heart disease, stroke, congestive heart disease, or peripheral artery disease) within the 3 months prior to inclusion in the study. The investigators classified the cardiovascular events by clinical evaluation. Angina was established on the clinical diagnosis and objective evidence of myocardial ischemia or coronary lesion. The control group included 476 individuals with no history of a cardiovascular event. Cardiovascular risk in cases and controls was estimated using the Systematic Coronary Risk Evaluation (SCORE) algorithm. Each case-control pair, recruited by the same investigator, was matched for sex, age (±5 years), and SCORE risk estimation (±1%).
Patients were excluded if they had a cardiovascular event before the 3 months prior to the study visit, were in treatment with corticoids or oral retinoids, or were receiving antiobesity treatment. All patients gave informed written consent to participate. The study was approved by the Ethics Committee of Hospital Carlos Haya, in Malaga, Spain.
The study data were collected in 2 phases: a retrospective review and a current review of the medical records. During the study visit, personal and demographic data, cardiovascular history, medication, BP, body mass index (BMI), analytical parameters, cardiovascular risk factors, and risk estimation with the SCORE algorithm were recorded. The analytical parameters included total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), adiponectin, hsCRP, HbA1c, serum creatinine, and fasting glucose. The classic cardiovascular risk factors included smoking, a family history of premature cardiovascular disease, diabetes, sedentary lifestyle, and dyslipidemia.
Waist circumference was determined using a non-elastic metric tape measure placed between the border of the rib cage and the iliac crest. Abdominal obesity was classified according to the following definitions: >94 cm in men and >80 cm in women, according to the criteria of the International Diabetes Federation (IDF),25 and >102 cm in men and >88 cm in women, according to the criteria of the National Cholesterol Education Program-Adult Treatment Panel (NCEP/ATP-III).26 Hypertension was established when systolic BP was ≥140 mm Hg and/or diastolic BP ≥90 mmHg (130 and 80 mmHg respectively, in patients with diabetes) or the patient was currently taking antihypertensive treatment.
Patients were considered to have a sedentary lifestyle if they did not walk, run, or swim for 30 to 45 min 3 or 4 times per week. A family history of premature cardiovascular disease was determined in first-degree relatives aged <55 years for men and <65 years for women. A smoker was a person who smoked at least 10 cigarettes per day.27 Hypercholesterolemia was established by a total cholesterol concentration of ≥240 mg/dL or current treatment with cholesterol-lowering drugs. Dyslipidemia was defined according to NCEP/ATP-III26 recommendations for intermediate risk populations: total cholesterol concentration ≥240 mg/dL, LDL-C >130 mg/dL, HDL-C <40 mg/dL in men and <50 mg/dL in women, triglycerides ≥150 mg/dL, or current treatment with lipid-lowering drugs. Serum creatinine concentrations were considered to be mildly elevated at values of 1.3 to 1.5 mg/dL in men and 1.2 to 1.4 mg/dL in women. Patients were considered to have diabetes if their blood glucose levels were ≥126 mg/dL, they had received a diagnosis of diabetes, or they were taking oral diabetes medication or were under insulin treatment.
Adiponectin was measured at a core laboratory (Laboratorios Echevarne, Spain) using a human adiponectin kit (E09, Mediagnost Co. Ltd), with a sensitivity of <0.06 ng/mL and within-run and between-run coefficients of variation of 7%. The remaining analyses were performed according to the standard practice of each participating center.
Statistical Methods
The 999 patients evaluated met all the inclusion criteria, and 80% of the study variables were available for them. Continuous variables are presented as the mean (SD). Comparisons between the groups of cases and controls were done with the Wilcoxon-Mann-Whitney test for independent data. Categorical variables are represented by frequency counts and percentages of all the responses evaluated. Percentages were compared with the c2 test. We used 95% confidence intervals, and all P values were 2-tailed. A P value less than .05 was considered significant.
Univariate analysis with a nonconditional logistic regression model was used to assess the relationship between each risk factor and the probability of experiencing a cardiovascular event. A multivariate nonconditional logistic regression analysis was also performed. The relationship between adiponectin concentrations and abdominal obesity measurements were examined with linear regression analysis or Pearson/Spearman correlation coefficients. The data were processed with SAS, version 9.1 (SAS Institute, Inc., Cary, North Carolina, USA).
RESULTS
Baseline Characteristics
The anthropometric and metabolic characteristics of the study population are shown in Table 1. The comparisons were performed in 2 categories: immediately after the event and 3 years before the study in both the case and control groups.
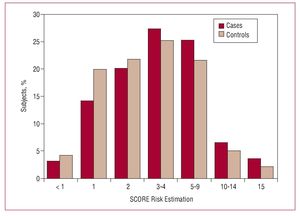
In the cardiovascular risk estimation with the SCORE algorithm, 64.5% of patients in the case group and 71.2% in the control group were classified with a low risk score (<3%) or intermediate risk score (3%-4%). There were no significant differences in cardiovascular risk between cases and controls (P=.09) (Figure 1).
Figure 1. Estimation of cardiovascular risk with the SCORE algorithm.
As to the obesity measurements, there were no differences in the BMI between cases and controls at either 3 years before the study or following the event; however, abdominal obesity (according to the IDF criteria) was greater in the case group than in the controls 3 years before the study (P=.012). There were no differences in the percentage of patients with central obesity in the assessment following the event.
The lipid profile also showed differences between cases and controls. In the analysis following the event, the cases had lower concentrations of total cholesterol, LDL-C, and HDL-C than the controls (P<.0001, P<.001, and P<.001, respectively); moreover, the cases presented lower plasma adiponectin concentrations (P=.0014) and higher hsCRP concentrations (P<.0001). Three years before the study, the cases showed significantly lower HDL-C (P<.0001) and higher triglycerides (P=.0296) than the controls. Adiponectin values from 3 years prior to the study were not available.
The cardiovascular events recorded are shown in Table 2. The most common cardiovascular condition was ischemic heart disease (70%), followed by cerebrovascular disease (20.5%), congestive heart failure (7.8%), and peripheral arterial disease (6.7%).
The pharmacological treatments received following the event for cases and controls are shown in Table 3. In general, the case group had a significantly higher percentage of treated patients.
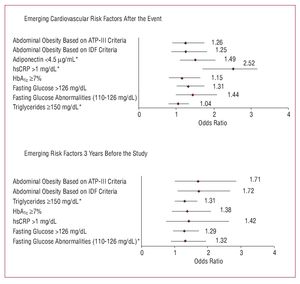
The relationship between emerging risk factors (abdominal obesity and concentrations of adiponectin, triglycerides, HbA1c, hsCRP, and fasting glucose) and the probability that a cardiovascular event would occur was investigated. There were no significant differences between the case-control pairs with regard to cardiovascular risk determined by the SCORE algorithm. The relationship between emerging risk factors and development of a cardiovascular event are shown in Figure 2.
Figure 2. Univariate analysis of emerging risk factors for a cardiovascular event. *Statistically significant.
Adiponectin values £4.5 µg/mL following the episode significantly correlated with occurrence of a cardiovascular event, with an odds ratio (OR) of 1.5 (95% confidence interval [CI], 1.10-2.04; P=.011); hsCRP > 1 mg/dL also showed a significant relationship (OR=2.52; 95% CI, 1.71-3.72; P<.0001). In the analysis of the data obtained in the 3 years before the study, the factors related to the development of a cardiovascular episode were abdominal obesity, according to the criteria of both the IDF (OR=1.70; 95% CI, 1.02-2.85; P=.0443) and NCEP/ATP-III (OR=1.71; 95% CI, 1.10-2.67; P=.0443) and triglycerides ≥150 mg/dL (OR=.31; 95% CI, 1.02-1.70; P=.037).
The classic risk factors associated with a cardiovascular event 3 years before the study were smoking (OR=1.38; 95% CI, 1.07-1.79; P=.013) and HDL-C level (OR=1.25; 95% CI, 1.07-1.39; P=.0002). The associated factors following the event were hypercholesterolemia (OR=1.50; 95% CI, 1.16-1.94; P=.002), smoking more than 20 cigarettes per day (OR=1.75; 95% CI, 1.14-2.70; P=.010), a family history of premature cardiovascular disease (OR=1.70; 95% CI, 1.23-2.38; P=.001), and elevated serum creatinine values (OR=1.28; 95% CI, 0.84-1.97; P=.247).
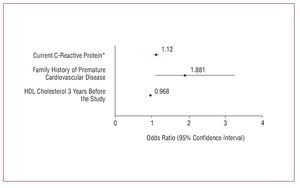
The emerging and classic risk factors that were significant in the univariate analysis were included in a multivariate analysis (Figure 3). The 3 factors that ultimately remained in the model were current hsCRP concentration, family history of premature cardiovascular disease, and HDL-C 3 years before the study. The model presented an accuracy rate of 68.2%. The adjusted OR for HDL-C 3 years before was 0.97 (95% CI, 0.95-0.99). Individuals with HDL-C levels 10 units lower 3 years ago presented a nearly 40% higher probability of experiencing a cardiovascular event than those with levels 10 units higher.
Figure 3. Multivariate analysis of emerging and classic cardiovascular risk factors. *Odds ratio per each 1-unit increase.
Plasma adiponectin concentrations presented an inverse relationship with waist circumference (Spearman rank correlation [r] = -0.012 and P=.0118). Lastly, an inverse correlation was also found between adiponectin and HDL-C concentration in the group of cases (Spearman r = -0.206; P<.0001).
DISCUSSION
Current cardiovascular risk scales present limitations for predicting the probability of experiencing a cardiovascular event. In our series, only 35.5% of patients who had an event showed high-risk status according to the SCORE algorithm. The role of emerging risk factors for improving the predictive power of current risk scales is controversial.28 Because of their pandemic character and their impact on the population, the emerging factors related with obesity are of particular interest. Adiponectin is a cytokine related with obesity. This is the first study that analyzes the relationship between adiponectin and cardiovascular disease in a broad sample of patients distributed over all of Spain.
In the population studied, an adiponectin concentration £4.5 µg/mL was associated with a risk of experiencing a first cardiovascular event. These results are consistent with those of other authors22,29 who have related hypoadiponectinemia with coronary disease. Although the cardiovascular event might have occurred up to 3 months before inclusion in this study, the adiponectin concentrations obtained after the event can be considered reliable. It has been shown that adiponectin values are a good predictor of secondary cardiovascular events over 7 years of follow-up.30
This study also showed that plasma adiponectin concentrations are inversely related to waist circumference and abdominal obesity. The results concur with those of other studies that show a relationship between plasma adiponectin concentrations and obesity, insulin resistance, and coronary disease.15,22,30,31 Moreover, a correlation was found between adiponectin and lipoprotein levels, in particular HDL-C. Other authors have indicated that the risk of experiencing a cardiovascular event is substantially correlated to abdominal obesity measurements and lipid metabolism.29,32 Our results support the idea that there is a relationship between adiponectin and lipid metabolism.
In addition to plasma adiponectin, a relationship was found between hsCRP concentrations following the event and the cardiovascular event (Figure 2). Although circulating hsCRP is a marker of inflammation, it is not clear whether it is a true predictor of a cardiovascular event, and there are controversial proposals in this regard.33,34 Assessment of emerging factors measured at 3 years before the study showed a relationship between abdominal obesity and triglyceride concentrations, and development of a cardiovascular event. These risk factors lost significance following the episode, and low adiponectin concentrations and high hsCRP concentrations remained as the only significant emerging factors. Nonetheless, the multivariate analysis showed that hsCRP was the only emerging factor significantly associated with a cardiovascular event. Adiponectin may have lost a significant relationship because of the limitations of the study.
The data from the present study show an improvement in abdominal obesity and BP in the group of cases with respect to the controls, in the interval from 3 years before the start of the study to the measurements taken after the event. These differences may be due to the implementation of lifestyle changes and to the pharmacological treatment given after a cardiovascular event. Likewise, secondary prevention measures may have contributed to improvements in the lipid profile, which showed decreases in serum concentrations of total cholesterol, LDL-C and triglycerides. It is interesting to note, however, that HDL-C concentrations measured after the event persisted at levels lower than the controls, which indicates that the drugs used, such as statins and other lipid-lowering agents, did not produce significant changes in HDL-C concentrations.
The present study has several limitations that should be specified. First, some of the measurements at 3 years before the study (waist circumference, HbA1c, and hsCRP) were not available for all the participants and this may have had an effect on the estimations of total risk. In addition, selection of patients who had a recent cardiovascular event and the size of the sample may have introduced bias in the study, with overestimation of risk. The fact that neurologists were not included may also have resulted in underestimation of the number of patients with cardiovascular disease and the relationship of this condition with adiponectin; nonetheless, internal medicine specialists attend a large part of these cases, and this is reflected in the percentage of stroke patients in our study population (20%).
Adiponectin was measured following the event and it cannot be concluded that this factor was unequivocally associated with the disease because it lost significance in the multivariate analysis and was not included in the secondary prevention measures.
CONCLUSIONS
Emerging risk factors may provide a new opportunity to improve the currently available risk estimations. This study shows that adiponectin is related to central obesity and cardiovascular disease in the Spanish population. Notwithstanding, a cohort study is needed to determine whether this factor will improve the predictive capacity of the SCORE algorithm. Moreover, because of the high prevalence of obesity in the Spanish population, the risk factors related to this condition (such as adiponectin) may be more useful for improving risk prediction in our population. However, additional studies should be performed to better evaluate the contribution of the emerging risk factors. The task of adding new data that will help to estimate patient risk, perhaps even better than the classic risk factors, has considerable, positive clinical relevance.
ACKNOWLEDGMENTS
The authors would like to express their thanks to the medical writing Department of Infociencia S.L.
ABBREVIATIONSBP: blood pressure
HbA1c: glycosylated hemoglobin
HDL-C: high density lipoprotein cholesterol
hsCRP: high-sensitivity C-reactive protein
LDL-C: low density lipoprotein cholesterol
The researchers and hospitals participating in the REFERENCE study are listed in the Appendix.
Correspondence: Dr. V. Barrios Alonso.
Departamento de Cardiología. Hospital Ramón y Cajal.
Ctra. de Colmenar, km 9.100. 28034 Madrid. España.
E-mail: vbarriosa@meditex.es; vbarrios.hrc@salud.madrid.org
Received February 27, 2008.
Accepted for publication June 25, 2008.