Patent foramen ovale (PFO) is the most common cause of cryptogenic stroke in patients younger than 55. Transesophageal echocardiography (TEE) has been accepted as the reference diagnostic technique. The purpose of this study was to compare the accuracy of transthoracic echocardiography (TTE), TEE and transcranial Doppler (TCD) in the diagnosis and quantification of patent foramen ovale.
MethodsWe studied 134 patients prospectively. Simultaneous TTE with TCD and TEE with TCD were performed, using agitated saline solution to detect right to left shunt.
ResultsIn 93 patients diagnosed with PFO, the shunt was visualized at baseline by TCD in 69% of cases, by TTE in 74% and by TEE in 58%. The Valsalva maneuver produced a similar improvement in shunt diagnosis with all 3 techniques (26%-28%). TTE and TCD showed higher sensitivity (100% vs 97%; non significant difference) than TEE in the diagnosis of PFO (86%; P<.001). TCD performed during TEE did not diagnose 12 (13%) shunts previously diagnosed during TTE. Similarly, TEE underestimated shunt severity.
ConclusionsTTE enables adequate diagnosis and quantification of PFO. TEE is less sensitive and tends to underestimate the severity of the shunt.
Keywords
Patent foramen ovale (PFO) has been associated with several disease processes such as paradoxical embolism in cryptogenic stroke,1 arterial gas embolism due to decompression,2 or platypnea-orthodeoxia syndrome.3 In recent years, the role of PFO in cryptogenic stroke and migraine and its therapeutic management has generated debate4,5,6,7,8,9,10 and the clinical method of choice for the diagnosis and quantification of right-to-left shunt remains undecided.11,12,13 Agitated saline serum has been used in transthoracic echocardiography (TTE), transesophageal echocardiography (TEE) and transcranial Doppler ultrasound (TCD) in the detection of intracardiac shunts. Although TEE has been considered the reference technique in PFO diagnosis, recent studies have suggested that it leads to false negatives due to the problems involved in performing the Valsalva maneuver.14,15,16,17 On the other hand, its association with atrial septal aneurysm (ASA) and its assessment of the severity of the shunt have been associated with an increased risk of recurrence.18,19 The use of TTE with harmonic imaging has led to the improved assessment of interatrial shunt.14,15,16,17,20 Few studies have analyzed the most suitable strategy for the diagnosis and quantification of PFO. The aim of the present study was to compare the results obtained by the simultaneous performance of TEE with TCD and of TTE with TCD in the diagnosis and quantification of shunt due to PFO and to define the most suitable diagnostic strategy for its assessment in clinical practice.
MethodsWe conducted a prospective study which included 134 patients (75 men and 59 women, mean age 46.4±14.2 [17–75] years) referred to the echocardiography laboratory by the neurology department to rule out PFO after presenting transient stroke (28; 21%), stroke (91; 68%), or migraine episodes (15; 11%). The study was approved by the Vall d’Hebron Hospital Ethics Committee and all the patients had previously given signed informed consent. Previous intracranial or extracranial arterial disease, abnormalities on TCD, or lacunar infarction were ruled out using computed tomography or magnetic resonance imaging. Table 1 shows the characteristics of the study population.
Table 1. Demographic Characteristics of the Population.
| Patients | 134 |
| Age (years) | 46.4±14.2 (17–75) |
| Men | 75 (56) |
| Women | 59 (44) |
| Smoking | 57 (43) |
| Hypertension | 31 (23) |
| Diabetes mellitus | 12 (9) |
| Dyslipidemia | 35 (26) |
Data are expressed as n (%) or mean±standard deviation (range).
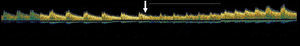
TCD with TTE were performed simultaneously and then, 5minutes later, TCD with TEE, using agitated saline solution to detect right-to-left shunt. The patient was in left lateral decubitus position during both studies. The Valsalva maneuver, which all patients had been taught to perform, was considered effective when there was a peak Doppler flow velocity reduction>25% in the middle cerebral artery21 (Figure 1).
Figure 1. Transcranial Doppler ultrasound recording during Valsalva maneuver. The arrow indicates the beginning of the Valsalva maneuver.
Transcranial Doppler UltrasoundThe TCD study was performed using a TCD 100 ML system (Spencer Technology, Seattle, Washington, USA) and MultiDop X4 (DWL Electronic Systems, Sipplingen, Germany). Middle cerebral artery flow was monitored through the temporal bone window using a 2MHz transducer. The TCD transducer was kept in place with an elastic headband fitted with the probe at a depth of 65mm with stable insonation. The study was performed by a neurologist specialized in this technique and blinded to the results of the echocardiographic study.
The middle cerebral artery blood flow velocity value obtained by TCD, simultaneously performed with TTE and with TEE, served as a reference to confirm the effectiveness of the Valsalva maneuver.
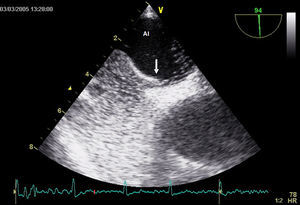
Transthoracic EchocardiographyAll the studies were performed using the Vivid 7 system (General Electric, Milwaukee, Wisconsin, USA) fitted with a 4.3MHz multi-frequency probe with harmonic imaging. The apical 4-chamber view was used to optimize visualization of the atria, ventricles and interatrial septum (Figure 2). In total, 3 patients had a suboptimal acoustic window, but were not excluded from the study. ASA was diagnosed when there was a ≥10-mm midline shift in anatomical M-mode or when total bidirectional shift was >15mm.
Figure 2. Transthoracic echocardiography showing contrast medium passing through the patent foramen ovale.
Transesophageal EchocardiographyTEE with color Doppler was performed using the same system fitted with a 2.9-8MHz multi-frequency probe. To improve tolerance to the test, patients were sedated with intravenously administered midazolam at a starting dose of 2mg followed by 2-mg increments until tolerance was reached and the patient felt comfortable. Blood pressure, heart rate and oxygen saturation were monitored. Baseline values were recorded during TTE and once every minute during TEE. An N-550 pulse oximeter (Nellcor, Boulder, Colorado, USA) and an automatic M4-I Intellisense blood pressure gauge (Omron, Schaumburg, Illinois, USA) were used.
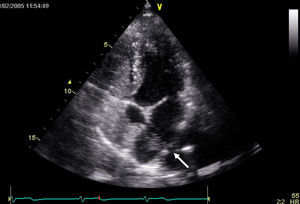
In line with the study aims, the area of the atrial septum in which the foramen ovale was located was visualized in the sagittal plane between 90o and 110o in the caval view (Figure 3). Maximum PFO diameter was measured during the Valsalva maneuver at the distal extreme of the tract formed by the ostium primum and ostium secundum. ASA was diagnosed using the same criteria described for the TTE study.
Figure 3. Transesophageal echocardiography showing contrast medium passing through the patent foramen ovale.
Agitated Saline Contrast TestA mixture of 9mL physiological saline and 1mL air was agitated 10 times in 210-mL syringes connected to a 3-way stopcock to exchange the air-saline mix and achieve good dilution. The bolus of saline solution was injected via an antecubital vein. The study was not begun until adequate filling of the right atrium was achieved. At least 2 injections were administered at baseline and up to 2 injections with the Valsalva maneuver in both the TTE and TEE studies. The Valsalva maneuver was begun when the contrast filled the right atrium and was maintained for >5s; the shunt was assessed during the first 3 heartbeats following the Valsalva maneuver. During TEE, the passage of contrast medium through the PFO was assessed; if its passage was not visualized, additional injections were administered and the openings of the pulmonary veins assessed to rule out intrapulmonary shunt.
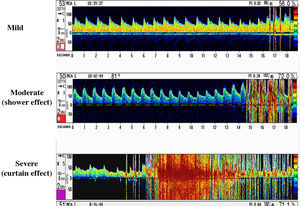
Diagnosis and QuantificationThe TTE or TEE contrast studies were considered positive for PFO when bubbles were observed in the left atrium within the first 3 heartbeats after opacification of the right atrium, whether at baseline or after the Valsalva maneuver. The severity of the shunt was quantified as mild (<10 microbubbles), moderate (10-20 microbubbles), or severe (>20).16 Right-to-left shunt was diagnosed when TCD detected microsignals in the middle cerebral artery, and the degree of severity was quantified according to established criteria22 (Figure 4). A definitive diagnosis of PFO was established when there was concordance between the 2 techniques in their diagnosis.
Figure 4. Quantification of the shunt by transcranial Doppler ultrasound.
Statistical AnalysisSensitivity, specificity and predictive values were determined by the percentage of patients with true positive and true negative results (95% confidence interval). The criteria applied for diagnosing true positives and true negatives was concordance between 2 of the 3 techniques (TTE, TEE and TCD) in the diagnosis of PFO. The diagnostic accuracy of TCD was established during simultaneous TTE study, since in clinical practice TCD is performed without sedation. Continuous values were expressed as mean±standard deviation. The kappa test was used to assess concordance in quantifying the severity of the shunts using different methods. The SPSS 13.0 software package was used for statistical analysis. A P value of <0.05 was used as a cutoff for statistical significance.
ResultsIn total, 93 (69%) of the 134 patients studied were diagnosed with PFO.
Diagnosis of Right-to-Left ShuntThe right-to-left shunt was visualized at baseline by TTE in 69 patients (74%), TCD in 64 (69%), and TEE in just 54 (58%). The Valsalva maneuver was effective in all TTE studies. In 10 patients, the Valsalva maneuver was considered ineffective during TEE, thus external abdominal compression was performed until a reduction >25% in peak blood flow velocity was obtained in the middle cerebral artery. The Valsalva maneuver produced a similar improvement in the diagnosis of right-to-left shunt not visualized at baseline in each of the 3 techniques: TTE 24/93 (26%), TCD 26/93 (28%), and TEE 26/93 (28%). The sensitivity, specificity, and predictive values of the 3 techniques are shown in Table 2.
Table 2. Diagnosis of Patent Foramen Ovale Using Different Imaging Techniques.
| Sensitivity, % | Specificity, % | PPV, % | NPV, % | |
| Transcranial Doppler ultrasound | 97 | 98 | 99 | 93 |
| Transthoracic echocardiography | 100 | 100 | 100 | 100 |
| Transesophageal echocardiography | 86 | 100 | 100 | 76 |
NPV, negative predictive value; PPV, positive predictive value.
During the TTE study, TCD failed to diagnose 3 mild shunts and gave a false positive in 1 patient with a pulmonary arteriovenous fistula, showing the contrast medium reaching the left atrium from a pulmonary vein (Figure 5). TCD performed during the TEE study failed to diagnose 2 mild shunts shown by TEE and gave the same false positive in the patient with pulmonary arteriovenous fistula. In 13 patients, TEE did not diagnose a shunt shown by TTE, which was mild in 11 cases, moderate in 1 and severe in 1 (Table 3). TCD performed simultaneously with TTE diagnosed 12 (13%) shunts more than when TCD was performed simultaneously with TEE; of these, 10 were mild, 1 moderate and 1 severe.
Figure 5. Transthoracic echocardiography in apical 4-chamber view showing contrast-filled right cavities and bubbles arriving from the right inferior pulmonary vein (arrow) in the left atrium.
Table 3. Echocardiographic Characteristics and Sedation Dose in Cases of False Negatives by Transesophageal Echocardiography.
| Patient | Shunt on TCD | Shunt on TTE | ASA | Midazolam (mg) during TEE |
| 1 | No | Mild | No | 8 |
| 2 | No | Mild | Yes | 10 |
| 3 | No | Mild | No | 8 |
| 4 | Mild | Mild | No | 8 |
| 5 | Mild | Mild | No | 6 |
| 6 | Mild | Mild | Yes | 5 |
| 7 | Mild | Mild | No | 12 |
| 8 | Mild | Mild | Yes | 8 |
| 9 | Mild | Mild | No | 10 |
| 10 | Mild | Mild | Yes | 8 |
| 11 | Moderate | Mild | No | 6 |
| 12 | Moderate | Moderate | Yes | 8 |
| 13 | Severe | Severe | No | 9 |
Abbreviations: ASA, atrial septal aneurysm; TCD, transcranial Doppler ultrasound; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
The dose of midazolam was similar in the group of patients in whom the results of TTE and TEE were in concordance and the group in whom results differed (8.1±3.2mg vs 8.2±1.3mg, respectively). During the TEE study, heart rate increased (74±18 bpm vs 94±18 bpm; P<.001), whereas there was a decrease in systolic blood pressure (121±11 mmHg vs 101±32 mmHg; P<.05) and oxygen saturation (98%±2% vs 93%±4%; P<.001). There were no significant differences in diastolic blood pressure (72±8 mmHg vs 72±10 mmHg).
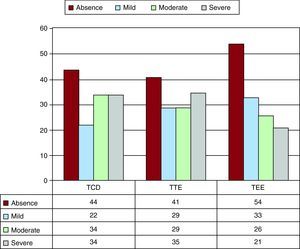
Quantification of the ShuntShunt was quantified as severe by TTE in 69% of the patients (64/93), by TCD in 76% (68/90) and by TEE in 59% (47/80) (Figure 6). In the quantification of shunt, concordance between TTE and TCD was 93% (84/90) (κ=0.83; P<.0001); between TEE and TCD, 74% (59/80) (κ=0.41; P<.0001); and between TTE and TEE, 81% (65/80) (κ=0,59; P<.0001). As visualized by TEE, PFO size during the Valsalva maneuver was 3.81±2.62mm in the patients with shunt and only 0.3±0.8mm in the patients without shunt (P<.001). PFO diameter was greater in the patients with a more severe shunt as determined by TTE; thus, in patients with a mild shunt the diameter was 2.3±1.3mm; with moderate shunt, 3.6±1.6mm; and with severe shunt, 5.6±3.5mm (P<.001).
Figure 6. Quantification of the shunt using the 3 techniques. TCD, transcranial Doppler ultrasound; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
Atrial Septal AneurysmIn 57 patients with right-to-left shunt, TEE study diagnosed ASA (61%), whereas in the patients without PFO ASA was only found in 5/41 patients (12%). TTE study diagnosed ASA in all patients except for one. The patients with PFO and ASA more often presented moderate or severe shunt than the patients with PFO without ASA (71% vs 13%; P<.001).
DiscussionThis study assessed a large series of patients to rule out the presence of right-to-left shunt, and demonstrated that TTE is superior to TEE in the diagnosis of PFO. TEE gave a false negative in more than 10% of the patients and tended to underestimate the severity of right-to-left shunt. TCD performed simultaneously with TTE and with TEE showed that these false negatives were not due to the imaging technique used itself, since TCD performed during TEE also gave a similar number of false negatives. TEE is less sensitive than TTE in the diagnosis of right-to-left shunt at baseline, with a similar number of cases diagnosed with Valsalva maneuver. The results are of clinical importance, since they suggest that TEE does not provide greater accuracy in the diagnosis and quantification of PFO than TTE or TCD. TEE would be indicated only in the presence of poor echocardiographic windows or when assessing the morphological characteristics of PFO before percutaneous closure.
Diagnosis of Patent Foramen Ovale by Different Imaging TechniquesSeveral studies have assessed the usefulness of TCD6,13,23, TTE14,15,16,17,20 and TEE24,25 in the diagnosis of PFO, but differences in the results obtained have led to great controversy. Neurologists have widely used TCD to diagnose PFO. Comparative studies with TEE suggest that its sensitivity is higher than 90%, but that its specificity is 65%-90%.15,26,27 Several studies have suggested that the low specificity of TCD may be due to extracardiac shunts.26 In the present study, there was good concordance between the TCD performed simultaneously with the 2 echocardiographic techniques, with only 1 false positive due to a right-to-left shunt arising from a pulmonary fistula. TCD did not detect 3 mild shunts diagnosed by TTE and 2 mild shunts diagnosed by TEE. These results show that a limitation of TCD is that it cannot be used to visualize the contrast medium entering the right atrium, and thus the Valsalva maneuver may not be performed whenthe right atrium is completely filled with contrast, and consequently mild shunts may be overlooked.
Several previous studies highlighted the low sensitivity of TTE compared to TEE, because interatrial shunt was detected in only 31%-47% of cases.27,28 The suboptimal quality of the images is considered the most limiting factor.29 Nevertheless, with the introduction of harmonic imaging, image quality and the detection of microbubbles in agitated serum have markedly improved. Recent studies have noted that TTE with harmonic imaging and TEE have similar accuracy in the detection of right-to-left atrial shunt14,20,30 and it is accepted that, when image quality is good, TTE can be effective in the detection of PFO.31
In young patients without clinical evidence of heart disease or atrial fibrillation, TTE appears to be effective in the diagnosis and quantification of PFO. Recently, preliminary studies have suggested the possible use of 3-dimensional TTE for this diagnosis.32,33
False Negatives on Transesophageal Echocardiographyin total, 13 of the 93 patients with PFO (14%) were not diagnosed on TEE; 2 had moderate-severe shunt. In some studies, TEE obtained false negatives in the diagnosis of PFO, which wereattributed to a poorly performed Valsalva maneuver.26 In the study conducted by Kúlhet al,14 interatrial shunt was not diagnosed on TEE in 6 of 57 patients with PFO diagnosed by TTE.
Both sedation and esophageal intubation are considered limiting factors when performing an adequate Valsalva maneuver. Nevertheless, in our series, the Valsalva maneuver contributed to a similar number of positive diagnoses on TTE (26%) and on TEE using moderate sedation (33%). Strikingly, without the Valsalva maneuver, TTE diagnosed shunt in 74% of patients and TEE in only 58%. Souteyrand et al15 showed that at baseline TTE diagnosed shunt in 50% of patients, whereas TEE with moderate sedation (midazolam 5mg) only diagnosed shunt in 33%. There is no definitive explanation for these results, but it is possible that the delicate balance between intra-atrial pressures34 can be modified by small hemodynamic changes due to sedation or esophageal intubation itself.
The present study is the first to use TCD simultaneously with TTE and with TEE, showing that, under moderate sedation and with esophageal intubation, TCD has reduced sensitivity to detect right-to-left shunt. On the other hand, continuous monitoring during the procedure demonstrated significant reductions in systemic systolic blood pressure and an increase in heart rate. This hemodynamic response can be explained by the fact that midazolam moderately reduces systolic blood pressure and also the mean pulmonary blood pressure.35,36 On the other hand, low-dose atropine and the difficulties involved in the test itself can explain tachycardia during TEE. It may be that these hemodynamic changes or intubation hinder the reversal of the interatrial right-to-left pressure gradient34 and thus the passage of microbubbles between the atria.
Severity of Right-to-Left Shunt and Assessment of Atrial Septal AneurysmThis study demonstrated that TEE can underestimate the severity of shunt, probably due to the difficulty involved in performing an adequate Valsalva maneuver in sedated patients. PFO size (maximum separation) during the Valsalva maneuver was significantly greater depending on the degree of shunt, and it was observed that all the patients who had a PFO diameter >4mm presented moderate or severe shunt.
ASA is frequently associated with PFO and increases the risk of stroke recurrence.4,37 Although TCD cannot be used to diagnose ASA, both TTE and TEE are of use in its detection. Harmonic imaging facilitates diagnosis by TTE, with accuracy similar toTEE. In the present study, 57 of the patients with PFO presented ASA (61%), whereas among the patients without PFO only 5/41 patients (12%) presented ASA.
LimitationsThe results of the present study are only applicable to the selected population group. The patients received moderate sedation that was slightly higher than that administered in other series. TEE is a semi-invasive test that is poorly tolerated without sedation, especially in the young population. In this regard, we followed the same sedation protocol as for other indications of the technique, since the assumption that the degree of intolerance would be greater for this indication appeared questionable. Although the patients were instructed in the correct performance of the Valsalva maneuver and its effectiveness was verified by a 25% reduction in middle cerebral artery peak flow velocity on TCD, this does not mean that the intensity of the Valsalva maneuver was identical to that performed without sedation and without esophageal intubation. The study did not analyze observer or interobserver variability, given that the greatest variability is generated by administration of the contrast medium and the effectiveness of the Valsalva maneuver, rather than by reviewing the acquired images, and that it was considered unethical to repeat the tests, given the study design.
ConclusionsTTE with harmonic imaging and the administration of agitated physiological saline solution enables adequate assessment and quantification of right-to-left shunt due to PFO. TEE with moderate sedation tends to give false negatives and underestimates the severity of the shunt. However, the TEE technique would be especially indicated in cases of poor image quality or to accurately assess the morphology of the interatrial partition when PFO closure is planned.
Conflicts of interestNone declared.
Acknowledgements
We would like to thank the registered nurses Rosa M. García and Carmen Abad for their invaluable assistance and collaboration in conducting the studies.
Received 14 April 2010
Accepted 12 October 2010
Corresponding author: Pg. Vall d’Hebron, 119-129, 08035 Barcelona, Spain. mtegonzalez@vhebron.net