Delayed diagnosis of hypertension may result in inadequate blood pressure control and increased cardiovascular risk. The aim of this study was to estimate the delay in hypertension diagnosis in patients with type 2 diabetes and the likelihood of a diagnosis within a suitable period (first 6 months), and to analyze the patient and physician characteristics associated with delayed diagnosis.
MethodsRetrospective dynamic cohort study, with a 7-year follow-up in primary care, of 8074 adult patients with diabetes who met the diagnostic criteria for hypertension. Two thresholds were considered: 140/90mmHg and 130/80mmHg. The time elapsed between meeting these criteria and recording the diagnosis was estimated; the time course of the likelihood of a missed diagnosis and the variables associated with correct diagnosis were assessed by Kaplan-Meier survival analysis and logistic regression analysis, respectively.
ResultsThe mean diagnostic delay was 8.9 (15.4) months in patients with blood pressure≥140/90mmHg compared to 15.2 (19.6) months for those with <140/90mmHg (P<.001). The main variables associated with correct diagnosis were baseline blood pressure≥140/90mmHg (odds ratio=2.77; 95% confidence interval, 2.44-3.15), no history of acute myocardial infarction (odds ratio=2.23; 95% confidence interval, 1.67-2.99), obesity (odds ratio=1.70; 95% confidence interval, 1.44-1.99), absence of depression (odds ratio=1.63; 95% confidence interval, 1.27-2.08), female sex (odds ratio=1.29; 95% confidence interval, 1.14-1.46), older age, and taking more intensive antidiabetic therapy. There was an inverse relationship with the age of physicians and a direct relationship with their professional stability.
ConclusionsThe mean diagnostic delay in hypertension among diabetic patients was greater than 6 months and varied according to the diagnostic threshold used. Patients with baseline blood pressure≥140/90mmHg were more likely to receive a timely diagnosis.
Keywords
.
INTRODUCTIONHypertension (HT) is a cardiovascular risk factor that affects 35% of the Spanish adult population.1
The prevalence of HT is between 1.5 and 2.3 times higher in patients with type 2 diabetes mellitus (DM2) than in nondiabetic subjects.2,3 When present it hastens the course of microvascular and macrovascular complications of DM24,5 and increases mortality, to the extent that 75% of deaths of cardiovascular origin in diabetic patients are attributable to HT.2,6
Monitoring HT in diabetics reduces mortality and prevents or delays the incidence of vascular complications.7,8 However, despite the availability of effective drug therapies, blood pressure (BP) control in these patients is poor, which may be partly due to underdiagnosis and delayed diagnosis. To date no reports have estimated the typical delay in diagnosing HT. Knowledge of these factors may enable implementation of procedures that will improve the management of these patients and reduce their cardiovascular risk.
The aims of this study were to estimate the delay in diagnosing HT in adults with DM2 in primary care (PC) according to the diagnostic threshold considered and the probability of these patients receiving a diagnosis with the first 6 months of the onset of HT, as well as to analyze the association between patient and physician characteristics and the likelihood of a delayed diagnosis.
METHODSThis retrospective, analytical, observational, dynamic cohort study was performed in 21 health centers in northeast Madrid. The study population comprised all patients diagnosed with DM2 in their electronic medical record (EMR) who attended at least 2 annual check-up visits in their PC centers. Patients older than 18 years who met the diagnostic criteria for HT between January 1, 2003 and June 30, 2009 and had at least 2 BP readings recorded in the EMR during the study year were included. Patients with a HT diagnosis at the start of the study and those with a follow-up lasting less than 6 months were excluded.
Patient inclusion and follow-up began on January 1, 2003; inclusion ended on June 30, 2009, and follow-up was completed on December 31, 2009.
Data were obtained from personalized secondary data in the patients’ EMR. Diagnoses of HT and DM2 recorded in the EMRs were validated in the same setting where the study was conducted,9 and a positive predictive value for DM of 91.23% and a negative predictive value of 99.98% were obtained. For the HT diagnostic threshold of 140/90mmHg, the positive and negative predictive values were 82.52% and 97.94%, and for the diagnostic threshold of 130/80mmHg, 98.68% and 53.92%, respectively.
A patient was considered diabetic when the EMR contained a diagnosis of DM2 (International Primary Care Classification codes K86 or K87).
The patient was considered hypertensive when the measurement of 2 or more systolic blood pressure (SBP) measurements taken on at least 2 consecutive visits was ≥130mmHg or the mean diastolic blood pressure (DBP), ≥80mmHg, according to seventh report of Joint National Committee guidelines.10
Given the lack of agreement among scientific societies on the diagnostic thresholds for HT in patients with DM2, this study considered a second HT threshold when the mean of 2 or more SBP measurements on at least 2 consecutive visits was ≥140mmHg or the mean DBP was ≥90mmHg, according to the NICE (National Institute for Clinical Excellence) standard.11
HT was considered diagnosed when recorded in the EMR, and as undiagnosed when the diagnostic criteria were met but no HT diagnosis was recorded in the EMR. The use of medication with a hypotensive effect but prescribed for indications other than HT was not considered.
We measured the time elapsed between the visit when the patient met the diagnostic criteria and the date when the diagnosis was recorded.
A diagnosis was defined as “correct” when it was recorded in the EMR during the first 6 months after the patient met the diagnostic criteria and as “incorrect” when it was not recorded until more than 6 months later or not at all. Patient-related variables (sociodemographic, comorbidity, anthropometric, biochemical parameters), use of health resources (consultation and treatments) and PC physician-related variables (sex, age, professional stability, work schedule and professional seniority) were analyzed.
Statistical AnalysisA descriptive analysis was prepared of the study population, overall and stratified by the BP measurement when diagnostic criteria were met. The time elapsed between meeting these criteria and recording of the diagnosis, along with the variation over time of the probability of remaining diagnosis-free, was estimated by Kaplan-Meier survival analysis. Log-rank test was used to study differences related to the degree of initial HT.
A univariate analysis was carried out of the factors associated with a correct diagnosis (ie, diagnosis of HT in the EMR during the first 6 months after the diagnostic criteria were met). The chi-square was used for qualitative variables and Student t test for quantitative variables. Variables with a significance<0.25 were included in the logistic regression analysis.
All estimates were calculated with their 95% confidence intervals (95%CI). A P value <.05 was considered statistically significant. Data were analyzed using SPSS 19.0 statistical software package (SPSS Inc.; Chicago, Illinois, United States).
The study was approved by the Carlos III Hospital Ethics Committee (Madrid).
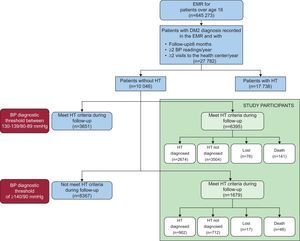
RESULTSFigure 1 shows the flow chart of study participation. Of the 27 782 patients with a diagnosis of DM2 recorded in the EMR in PC centers during the study period, 63.8% ad HT at the time of the DM2 diagnosis and were excluded from the study population. Of the 10 046 patients who did not have HT when DM2 was diagnosed, 80.4% (n=8074) had BP values ≥130/80mmHg during follow-up. Of these, 79.2% (n=6395) had SBP of 130 to 139mmHg or DBP of 80 to 89mmHg and 20.8% (n=1679) had SBP ≥140mmHg or DBP ≥90mmHg.
For the lower diagnostic threshold (130-139/80-89mmHg), 41.8% of patients were diagnosed and the diagnosis was recorded on the EMR and 54.8% remained diagnosis-free after a median follow-up of 3.4 [interquartile range, 1.6-5.2] years. For the diagnostic threshold of BP ≥140/90mmHg, 53.7% were diagnosed and 42.4% remained diagnosis-free after a median follow-up of 3.6 [1.7-5.4] years.
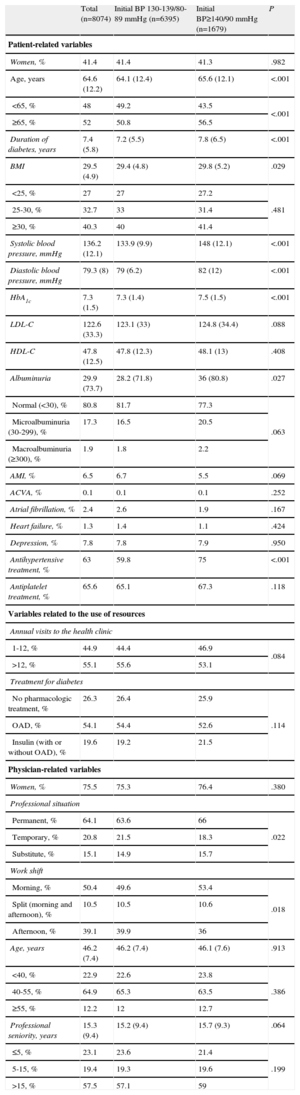
Table 1 summarizes the main characteristics of the study participants and their physicians, in general and stratified by the patients’ baseline BP.
Baseline Characteristics of the Sample
| Total (n=8074) | Initial BP 130-139/80-89 mmHg (n=6395) | Initial BP≥140/90 mmHg (n=1679) | P | |
| Patient-related variables | ||||
| Women, % | 41.4 | 41.4 | 41.3 | .982 |
| Age, years | 64.6 (12.2) | 64.1 (12.4) | 65.6 (12.1) | <.001 |
| <65, % | 48 | 49.2 | 43.5 | <.001 |
| ≥65, % | 52 | 50.8 | 56.5 | |
| Duration of diabetes, years | 7.4 (5.8) | 7.2 (5.5) | 7.8 (6.5) | <.001 |
| BMI | 29.5 (4.9) | 29.4 (4.8) | 29.8 (5.2) | .029 |
| <25, % | 27 | 27 | 27.2 | .481 |
| 25-30, % | 32.7 | 33 | 31.4 | |
| ≥30, % | 40.3 | 40 | 41.4 | |
| Systolic blood pressure, mmHg | 136.2 (12.1) | 133.9 (9.9) | 148 (12.1) | <.001 |
| Diastolic blood pressure, mmHg | 79.3 (8) | 79 (6.2) | 82 (12) | <.001 |
| HbA1c | 7.3 (1.5) | 7.3 (1.4) | 7.5 (1.5) | <.001 |
| LDL-C | 122.6 (33.3) | 123.1 (33) | 124.8 (34.4) | .088 |
| HDL-C | 47.8 (12.5) | 47.8 (12.3) | 48.1 (13) | .408 |
| Albuminuria | 29.9 (73.7) | 28.2 (71.8) | 36 (80.8) | .027 |
| Normal (<30), % | 80.8 | 81.7 | 77.3 | .063 |
| Microalbuminuria (30-299), % | 17.3 | 16.5 | 20.5 | |
| Macroalbuminuria (≥300), % | 1.9 | 1.8 | 2.2 | |
| AMI, % | 6.5 | 6.7 | 5.5 | .069 |
| ACVA, % | 0.1 | 0.1 | 0.1 | .252 |
| Atrial fibrillation, % | 2.4 | 2.6 | 1.9 | .167 |
| Heart failure, % | 1.3 | 1.4 | 1.1 | .424 |
| Depression, % | 7.8 | 7.8 | 7.9 | .950 |
| Antihypertensive treatment, % | 63 | 59.8 | 75 | <.001 |
| Antiplatelet treatment, % | 65.6 | 65.1 | 67.3 | .118 |
| Variables related to the use of resources | ||||
| Annual visits to the health clinic | ||||
| 1-12, % | 44.9 | 44.4 | 46.9 | .084 |
| >12, % | 55.1 | 55.6 | 53.1 | |
| Treatment for diabetes | ||||
| No pharmacologic treatment, % | 26.3 | 26.4 | 25.9 | .114 |
| OAD, % | 54.1 | 54.4 | 52.6 | |
| Insulin (with or without OAD), % | 19.6 | 19.2 | 21.5 | |
| Physician-related variables | ||||
| Women, % | 75.5 | 75.3 | 76.4 | .380 |
| Professional situation | ||||
| Permanent, % | 64.1 | 63.6 | 66 | .022 |
| Temporary, % | 20.8 | 21.5 | 18.3 | |
| Substitute, % | 15.1 | 14.9 | 15.7 | |
| Work shift | ||||
| Morning, % | 50.4 | 49.6 | 53.4 | .018 |
| Split (morning and afternoon), % | 10.5 | 10.5 | 10.6 | |
| Afternoon, % | 39.1 | 39.9 | 36 | |
| Age, years | 46.2 (7.4) | 46.2 (7.4) | 46.1 (7.6) | .913 |
| <40, % | 22.9 | 22.6 | 23.8 | .386 |
| 40-55, % | 64.9 | 65.3 | 63.5 | |
| ≥55, % | 12.2 | 12 | 12.7 | |
| Professional seniority, years | 15.3 (9.4) | 15.2 (9.4) | 15.7 (9.3) | .064 |
| ≤5, % | 23.1 | 23.6 | 21.4 | .199 |
| 5-15, % | 19.4 | 19.3 | 19.6 | |
| >15, % | 57.5 | 57.1 | 59 | |
ACVA, acute cerebrovascular accident (excluding transitory ischemic attacks); AMI, acute myocardial infarction; BMI, body mass index; BP, blood pressure; HbA1c: glucohemoglobin; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; OAD, oral antidiabetic.
Unless specified otherwise, data are expressed as mean (standard deviation).
A missed diagnosis of HT was lower in patients with BP≥140/90mmHg (42.4% compared to 63.1% of those with BP≥130/80mmHg and <140/90mmHg at onset; P<.001), in women (50.5% compared to 58% of men; P<.001), and in those aged 65 or over (51% compared to 59.2% of those under 65; P<.001).
Hypertensive patients ultimately diagnosed by their physician experienced a mean delay of 11.1 (17.7) months. Of these, 63.2% were diagnosed during the first 6 months; 6.1% between 6 and 12 months; 10.4% between 12 and 24 months; and for 20.2% the diagnosis was delayed more than 24 months. The mean delay in patients who had BP≥140/90mmHg was 8.9 (15.4) months compared to 15.2 (19.6) months for those with baseline BP values ≥130/80 and <140/90mmHg (P<.001).
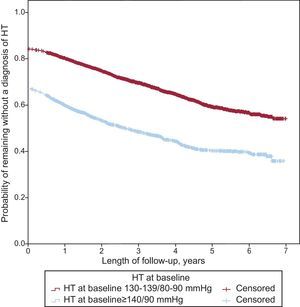
Figure 2 shows the survival curve for the probability of remaining diagnosis-free over time, stratified by BP values at onset of HT. Patients with an initial BP≥140/90mmHg were significantly more likely to receive a diagnosis (log rank test, P<.001).
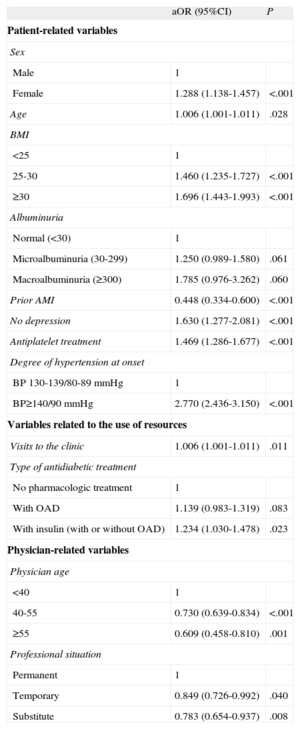
The variables associated with correct diagnosis are shown in Table 2. Patients with initial BP≥140/90mmHg had a probability of receiving a correct diagnosis that was 2.77 (95%CI, 2.44-3.15) times higher than patients with lower initial BP readings. Other strongly associated variables were not having a record of acute myocardial infarction in the EMR (odds ratio [OR]=2.23; 95%CI, 1.67-2.99), obesity (OR=1.70; 95%CI, 1.44-1.99), not having depression (OR=1.63; 95%CI, 1.27-2.08) and receiving treated antiplatelet agents (OR=1.47; 95%CI, 1.29-1.68). There was a nonsignificant trend toward association with microalbuminuria and macroalbuminuria. In addition, women, older patients, those with a more intensive antidiabetic treatment, and those who attended the health center most frequently were more likely to receive a correct diagnosis. Of the physician-related variables, age and professional stability had a significant inverse and direct relationship with correct diagnosis, respectively.
Variables Associated With Appropriate Diagnosis of Hypertension on Multivariable Logistic Regression Analysis
| aOR (95%CI) | P | |
| Patient-related variables | ||
| Sex | ||
| Male | 1 | |
| Female | 1.288 (1.138-1.457) | <.001 |
| Age | 1.006 (1.001-1.011) | .028 |
| BMI | ||
| <25 | 1 | |
| 25-30 | 1.460 (1.235-1.727) | <.001 |
| ≥30 | 1.696 (1.443-1.993) | <.001 |
| Albuminuria | ||
| Normal (<30) | 1 | |
| Microalbuminuria (30-299) | 1.250 (0.989-1.580) | .061 |
| Macroalbuminuria (≥300) | 1.785 (0.976-3.262) | .060 |
| Prior AMI | 0.448 (0.334-0.600) | <.001 |
| No depression | 1.630 (1.277-2.081) | <.001 |
| Antiplatelet treatment | 1.469 (1.286-1.677) | <.001 |
| Degree of hypertension at onset | ||
| BP 130-139/80-89 mmHg | 1 | |
| BP≥140/90 mmHg | 2.770 (2.436-3.150) | <.001 |
| Variables related to the use of resources | ||
| Visits to the clinic | 1.006 (1.001-1.011) | .011 |
| Type of antidiabetic treatment | ||
| No pharmacologic treatment | 1 | |
| With OAD | 1.139 (0.983-1.319) | .083 |
| With insulin (with or without OAD) | 1.234 (1.030-1.478) | .023 |
| Physician-related variables | ||
| Physician age | ||
| <40 | 1 | |
| 40-55 | 0.730 (0.639-0.834) | <.001 |
| ≥55 | 0.609 (0.458-0.810) | .001 |
| Professional situation | ||
| Permanent | 1 | |
| Temporary | 0.849 (0.726-0.992) | .040 |
| Substitute | 0.783 (0.654-0.937) | .008 |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; aOR, adjusted odds ratio; BMI, body mass index; BP, blood pressure; OAD, oral antidiabetic.
Although the relationship between BP and cardiovascular risk appears continuous up to an SBP of 115 to 110mmHg and a DBP of 75 to 70mmHg,12,13 decision-making in PC practice requires an operational definition. For the adult general population the diagnosis of HT is established as a mean BP measurement in the clinic≥140/90mmHg.5,10 However, because of the increased cardiovascular risk in diabetic patients, many scientific societies have set a lower threshold for these patients of 130/80mmHg,5,10,14 although there is no consensus to establish this threshold. Thus, the Spanish Ministry of Health clinical guidelines for DM215 set the threshold at ≥140/80mmHg and NICE maintained the cut-off at ≥140/90mmHg.11
The reduction in diagnostic threshold to BP values of 130/80mmHg is controversial and remains a moot point. In the 2009 review, the European guidelines on HT management16 increased the cut-off point set in 2007 (130/80mmHg)5 to 140/85mmHg. The results of the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial17 and INVEST (International Verapamil-Trandolapril Study)18 were still unknown at that time; these trials concluded that maintaining SBP below 130mmHg in patients with HT and DM2 does not lead to a cardiovascular benefit.
The debate caused by lowering diagnostic thresholds may have influenced the absence of a HT diagnosis in diabetic patients with BP<140/90mmHg. With this cut-off point, the percentage of patients with HT who remained without diagnosis in 2009 decreased from 23.1% to 8.8%.
For the diagnostic threshold of 130/80mmHg, 23.1% of all diabetic and hypertensive patients in the study area remained without a diagnosis in 2009. This result is slightly lower than the 29% reported in a population sample of 1507 diabetic patients in the United States19 and a little higher than the 20.2%9 and the 20.5%20 in the 2 previous Spanish studies. Irrespective of the differences in methodology between the different studies, our data confirm the low level of HT diagnosis in patients with diabetes.
As in other reports, underdiagnosis of HT occurs mainly in men and younger patients,1,3,21,22 regardless of the diagnostic criteria used.
In our study, the mean delay in HT diagnosis by PC physicians after diagnostic BP values are recorded is greater in men, younger patients, and those with lower initial BP. To the best of our knowledge, this is the first study that estimates the delay in HT diagnosis, therefore we cannot compare our results with those of other studies.
Variables that were independently associated with a correct diagnosis include known factors related to cardiovascular risk and poor BP control, such as obesity20,23,26 or macroalbuminuria,24,25 which indicates that physicians diagnose HT earlier in patients at higher risk. This hypothesis would seem to be confirmed by the earlier diagnosis in patients with receiving more intensive treatment.
However, other associated risk factors are poor control of HT, male sex,22,26 younger age,26 and a diagnosis of depression. In DM2 patients, depression is an additional risk factor because it is associated with a higher prevalence of complications and mortality.27,28
Patients with a prior acute myocardial infarction were less likely to be diagnosed with HT than those free of myocardial ischemia history, which may be because the follow-up of HT in these patients is recorded in the acute myocardial infarction episode rather than as an independent diagnosis; ie, there may be underrecording rather than underdiagnosing. This hypothesis is supported by the finding that 98% of these patients had a prescription for hypotensive drugs, regardless of whether or not the HT diagnosis was recorded in the EMR. However, we cannot rule out that the lower probability of acute myocardial infarction patients being diagnosed may translate into a lack of awareness of the importance of high BP in patients with ischemic heart disease.
Regarding physician characteristics, it is known that they accept higher BP values than those recommended in clinical guidelines.29,30 This may be because of the “clinical inertia”31 that occurs when the physician recognizes the problem but does not make a related decision.
Our results reveal that greater seniority is related to fewer correct diagnoses of HT; this finding is in accordance with those of other studies showing that higher seniority decreases continuous professional development for physicians and compliance with the recommendations of clinical guidelines.32,33
As in other studies, our results did not reveal a statistically significant relationship between physician sex and the accuracy of the diagnosis.30,34 However, this finding was associated with stability at work, which may be explained by greater knowledge of the population and increased involvement in patient follow-up.
Strengths and LimitationsOur study may have a classification bias, as the definition of HT does not consider whether patients were treated with drugs with a hypotensive effect that are prescribed for HT or other indications.
The definition of delayed diagnosis used in this study (>6 months from the availability of diagnostic BP values) was based on the fact that, for stable diabetics, clinical guidelines recommend a twice-yearly check-up visits. In addition, many PC physicians postpone recording the diagnosis between 3 and 6 months to recommend lifestyle changes for their patients or to assess the damage in target organs; such assessment may take 3 to 6 months.
Another possible limitation arises from the use of a secondary information source, the EMR, which is designed for care purposes. Nonetheless, the variables used appear sturdy and the quality of care partly depends on correct recording of BP readings.
The influence on delayed diagnosis of an improper referral from the nursing consultation to the medical consultation needs to be assessed. According to the visits scheduled in diabetic care programs, nurses follow-up the BP measurements, which are assessed in 6-monthly medical consultations. Only the physician was included in our analysis.
A strength of this study is that it collates available information for the entire diabetic population monitored in health centers and by all professionals, which reduces the bias related to voluntary participation.
Given that the responsibility for the diagnosis, treatment and monitoring of DM and HT falls mainly on PC professionals, this setting was deemed the most suitable to obtain information on real clinical conditions.
Strategies need to be implemented that improve the care of hypertensive patients in general and in the subgroup of younger men in particular, to detect and treat HT early with the goal of reducing their cardiovascular risk.
CONCLUSIONSThe delay in PC diagnosis of HT in patients with diabetes varies according to the diagnostic thresholds used and is greater for the 130/80mmHg diagnostic criteria.
More than half of the patients are diagnosed within the first 6 months.
Older patients, women, and those with initial BP values≥140/90mmHg were more likely to receive a correct diagnosis. In addition, there was an inverse association between correct diagnosis and physician age older than 40 years and working in a less stable professional situation.
CONFLICTS OF INTERESTNone declared.