The aim of this study was to compare the in-hospital clinical outcomes of minimally invasive, isolated aortic valve replacement vs median sternotomy.
MethodsBetween 2005 and 2012, 615 patients underwent aortic valve replacement at a single institution, 532 by a median sternotomy (E group) and 83 by a J-shaped ministernotomy (M group).
ResultsNo significant differences were found between the E and M groups in terms of age (69.27 [9.31] years vs 69.40 [10.24] years, respectively), logistic EuroSCORE (6.27 [2.91] vs 5.64 [2.17], respectively), size of implanted valve prosthesis (21.94 [2.04] mm vs 21.79 [2.01] mm, respectively), or the incidence of diabetes, hypercholesterolemia, high blood pressure, or chronic obstructive pulmonary disease. Mean cardiopulmonary bypass time was 102.90 (41.68) min for the E group vs 81.37 (25.41) min for the M group (P<.001). Mean cross-clamp time was 77.31 (29.20) min vs 63.45 (17.71) min for the S and M groups, respectively (P<.001). Mortality in the E group was 4.88% (26). There were no deaths in the M group (P<.05). The E group was associated with longer intensive care unit and hospital stays: 4.17 (5.23) days vs 3.22 (2.01) days (P=.045) and 9.58 (7.66) days vs 7.27 (3.83) days (P<.001), respectively. E group patients had more postoperative respiratory complications (42 [8%] vs 1 [1.2%]; P<.05). There were no differences when postoperative hemodynamic, neurologic, and renal complications, systemic infection, and wound infection were analyzed.
ConclusionsIn terms of morbidity, mortality, and operative times, outcomes after minimally invasive surgery for aortic valve replacement are at least comparable to those achieved with median sternotomy. The length of the hospital stay was reduced by minimally invasive surgery in our single-institution experience. The retrospective nature of this study warrants further randomized prospective trials to validate our results.
Keywords
.
INTRODUCTIONThe science of medicine is undergoing constant development and change. For over 10 years, there has been a growing interest in reducing to the greatest possible extent the aggression and trauma to which the organism is subjected during surgical procedures, and this principle has given birth to the so-called “minimally invasive approaches.” Cardiac surgery has not remained on the sidelines with respect to this trend and, as a result, a number of different minimally invasive techniques have been described. In aortic valve surgery, median sternotomy has been the approach of choice since it was introduced into cardiac surgery by Julian et al.1 However, since Cosgrove and Sabik2 described vertical parasternal thoracotomy in 1996, a number of groups have continued to present their experience with different types of minimally invasive approaches for aortic valve replacement: “J” ministernotomy, reversed “C” ministernotomy, “L” ministernotomy, “T” ministernotomy, and minithoracotomies.3–7 Several advantages have been attributed to approaches of this type when compared with the standard techniques: better cosmetic outcome, less postoperative pain, and better and more rapid recovery of respiratory function, as well as a reduction of both the hospital stay and the intensive care unit (ICU) stay. However, the results reported in these studies continue to be controversial.8–16
Our unit began to perform minimally invasive techniques in routine practice in 2005. The purpose of this study is to compare both the intraoperative and postoperative outcomes in the patients subjected to a minimally invasive approach vs the standard approach in aortic valve replacement surgery.
METHODSWe carried out a retrospective study based on data obtained in a single center. The data were collected from the unit's computer database by the first author. In some cases, it was necessary to review medical records to obtain all the necessary data. Between November 2005 and May 2012, after excluding the patients who had required emergency surgery, those who had undergone some other concomitant procedure, and those subjected to reintervention, we studied 615 patients with ages ranging between 25 and 91 years (mean, 69.29 [9.44] years) who underwent consecutive interventions for primary isolated aortic valve replacement. In 532 patients, the intervention involved the standard approach (E group) and in 83, a minimally invasive approach (M group).
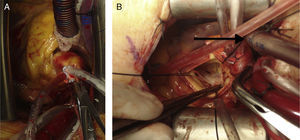
Anesthesia and Surgical TechniqueAll patients were subjected to the same anesthesia and monitoring regimen. The interventions were carried out with cardiopulmonary bypass and mild hypothermia (32°C to 34°C), central venous catheterization, and standard aortic clamping. Of the staff of 5 surgeons in our unit, 4 (80%) performed the minimally invasive interventions, but differed in the percentage carried out by each. Cold (4°C) blood cardioplegia was utilized for myocardial protection. Except for the incision and venous catheterization, the remainder of the surgical technique was similar in both groups. In the E group, an incision measuring 20cm to 25cm was made in the skin, followed by complete median sternotomy; central venous catheterization was performed in right atrial appendage using a 32 Fr venous catheter (Fig. 1A). In the M group, an 8-cm incision was made in the skin starting at the sternal angle and continuing toward the caudal end, followed by a “J” ministernotomy going from the sternal notch to the right fourth intercostal space. The central venous catheter (29 Fr) was advanced through the superior vena cava toward right atrium and inferior vena cava (Fig. 1B). In the M group, continuous CO2 insufflation was utilized during cardiopulmonary bypass to facilitate the removal of air from the cardiac chambers; in contrast, in the E group, this was not routinely employed. When it was necessary to defibrillate the heart after the aortic clamp had been released, conventional internal defibrillator paddles were used for patients in the E group and pediatric paddles were employed in the M group. The choice of the type of approach to be utilized was left exclusively to the discretion of each surgeon.
The criteria for transfusion, extubation, and drain removal were the same in both groups.
Statistical AnalysisThe data were analyzed using the SPSS software package (version 12.0). The values are expressed either in percentages or in means (standard deviation). The Mann-Whitney U test was utilized for the analysis of the continuous variables and the Pearson chi-square test for categorical variables. A P value <.05 was considered to indicate statistical significance.
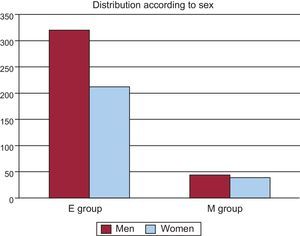
RESULTSWe found no significant differences between the E and M groups with respect to age (69.27 [9.31] years vs 69.40 [10.24] years, respectively; P=.592) or the risk of in-hospital mortality (6.27 [2.91] vs 5.64 [2.17], respectively; P=.148)]; the latter was calculated using the logistic EuroSCORE (European System for Cardiac Operative Risk Evaluation), the system for surgical risk stratification in cardiac surgery most widely used in Europe. Sex distribution (Fig. 2) was also similar, there being 212 women (40%) and 320 men (60%) in the E group and 39 women (47%) and 44 men (53%) in the M group (P=.218). No significant differences were found between the 2 groups with respect to the remaining preoperative characteristics: incidences of obesity, chronic obstructive pulmonary disease, diabetes mellitus, hypertension, renal failure, hypercholesterolemia, and left ventricular ejection fraction, measured by echocardiography. However, peripheral artery disease was more prevalent in the E group: 58 patients (11%) vs 3 patients (3.7%) in the M group (P=.039) (Table 1).
Preoperative Demographic Characteristics, Risk Score, and Cardiovascular Risk Factors of the Patients in This Series
| M group | E group | P | |
| Patients, no. | 83 | 532 | |
| Age, years | 69.40±10.24 | 69.27±9.31 | .592 |
| Sex | |||
| Women | 39 (47) | 212 (40) | .218 |
| Men | 44 (53) | 320 (60) | |
| EuroSCORE | 5.64±2.17 | 6.27±2.91 | .148 |
| Obesity | 14 (16.8) | 107 (20.1) | .456 |
| Renal failure | 8 (9.63) | 38 (7.14) | .444 |
| Peripheral artery disease | 3 (3.75) | 58 (11) | .039 |
| COPD | 7 (8.5) | 62 (11) | .387 |
| Diabetes mellitus | 19 (23) | 150 (28) | .314 |
| Hypercholesterolemia | 43 (52) | 232 (44) | .162 |
| Hypertension | 51 (61) | 328 (62) | .971 |
| LVEF, % | 51.11±17.30 | 50.38±15.50 | .594 |
COPD, chronic obstructive pulmonary disease; E group, median sternotomy; LVEF, left ventricular ejection fraction; M group, ministernotomy.
Data are expressed as no. (%) or mean±standard deviation, unless otherwise indicated.
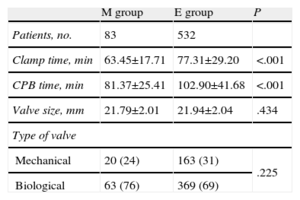
Both the cardiopulmonary bypass time and the aortic clamp time were significantly shorter in the M group compared to the E group: 81.37 (25.41) min vs 102.90 (41.68) min; (P<.001) and 63.45 (17.71) min vs 77.31 (29.20) min (P<.001), respectively. No significant differences were observed between the 2 groups in terms of the type or size of valve implanted (Table 2). At the beginning of the series, 3 patients in the M group required conversion to full sternotomy. In one of the cases, this was necessary to gain a better control of pulmonary artery bleeding provoked iatrogenically with the aortic clamp and, in the other 2 cases, because the surgeon preferred to have a direct view of the entire heart after the removal of the aortic clamp had provoked fibrillation.
Intraoperative Data: Operative Times and Prostheses Implanted
| M group | E group | P | |
| Patients, no. | 83 | 532 | |
| Clamp time, min | 63.45±17.71 | 77.31±29.20 | <.001 |
| CPB time, min | 81.37±25.41 | 102.90±41.68 | <.001 |
| Valve size, mm | 21.79±2.01 | 21.94±2.04 | .434 |
| Type of valve | |||
| Mechanical | 20 (24) | 163 (31) | .225 |
| Biological | 63 (76) | 369 (69) | |
CPB, cardiopulmonary bypass; E group, median sternotomy; M group, ministernotomy.
Data are expressed as no. (%) or mean±standard deviation, unless otherwise indicated.
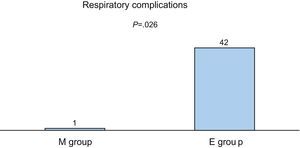
There was no in-hospital mortality in the M group but a rate of 4.88 (26 patients) in the E group, a difference that was statistically significant (P<.05); both rates were lower than the expected mortality according to the EuroSCORE. Although there were fewer reinterventions due to bleeding in the M group (2 cases [2.4%] vs 36 cases [6.7%] in the E group), the differences did not reach statistical significance (P=.125). In contrast, important differences in favor of the M group were found in terms of the days spent in the ICU and the total length of the postoperative hospital stay: 3.22 (2.01) days vs 4.17 (5.23) days (P=.045) and 7.27 (3.83) days vs 9.58 (7.66) days (P<.001), respectively. The M group developed fewer hemodynamic and neurological complications and problems involving the surgical wound, but the difference did not reach statistical significance. However, the incidence of respiratory complications (pneumothorax, pleural effusions, and respiratory failure) was significantly lower in the M group: 1 case (1.2%) vs 42 cases (8%) in the E group (P=.026) (Table 3; Fig. 3).
Postoperative Data: Operative Times and Prostheses Implanted
| M group | E group | P | |
| Patients, no. | 83 | 532 | |
| Mortality | 0 | 26 (4.88) | <.05 |
| Total ICU stay, days | 3.22±2.01 | 4.17±5.23 | .045 |
| Duration postoperative hospital stay, days | 7.27±3.83 | 9.58±7.66 | <.001 |
| Reinterventions due to bleeding | 2 (2.4) | 36 (6.7) | .125 |
| Respiratory tract infections | 3 (3.6) | 37 (6.9) | .251 |
| Hemodynamic complications | 10 (12) | 63 (11.8) | .957 |
| AF | 8 | 59 | |
| AV block | 2 | 2 | |
| Left heart failure | 0 | 1 | |
| IABC | 2 | 10 | |
| AMI | 0 | 1 | |
| Neurologic complications | 0 (0) | 11 (2) | .186 |
| Renal complications | 5 (6) | 27 (5) | .717 |
| ARF with hemodialysis/hemofiltration | 5 | 22 | |
| ARF with hemodialysis/hemofiltration | 0 | 5 | |
| Respiratory complications | 1 (1.2) | 42 (8) | .026 |
| Pneumothorax | 1 | 10 | |
| Pleural effusion | 0 | 12 | |
| Respiratory failure | 0 | 20 | |
| Surgical wound complications | 1 (1.2) | 27 (5) | .116 |
AF, atrial fibrillation; AMI, acute myocardial infarction; ARF, acute renal failure; AV, atrioventricular; E group, median sternotomy; IABC, intraaortic balloon counterpulsation; ICU, intensive care unit; M group, ministernotomy.
Data are expressed as no. (%) or mean±standard deviation, unless otherwise indicated.
With the increase in the life expectancy of the general population, due in part to advances in the treatment of many chronic diseases, surgeons are confronted with the need to make decisions involving increasingly complex patients; this makes it necessary to search for increasingly less invasive and less aggressive alternatives for the treatment of certain cardiac diseases. In the area of aortic valve disease, transcatheter aortic valve implantation has recently been presented as an option for patients with very high surgical risk.17–20 However, the procedure is not free of complications, the incidence of which is even higher than in conventional surgery; given these considerations, together with its high cost, it is still not possible to offer it to all patients. Thus, the minimally invasive approach in cardiac surgery becomes seen as a good strategy, especially if some of the benefits attributed to it can be demonstrated.
Different groups have presented their experience with the techniques employed in minimally invasive approaches. However, to date, the results obtained have generated controversy. Although most authors observe advantages in the postoperative results, such as less pain, less bleeding with a decrease in the need for blood product transfusion, shorter ICU and hospital stays, better cosmetic outcome, etc., in favor of the minimally invasive approach, these findings do not reach statistical significance in some reports.15,21–25 One of the causes to which this circumstance is attributed is the small number of patients studied. On the other hand, some reports demonstrate significantly better outcomes with this approach in terms of a better and more rapid postoperative recovery, reduced stays in both the ICU and the ward, as well as a better recovery of respiratory function and less pain.9,16,26,27 Moreover, in descriptive studies of the results obtained with minimally invasive techniques, these approaches are shown to be feasible and safe, without increasing either the rate of postoperative complications or mortality compared to the standard technique.28,29
Our unit has more than 7 years of experience in the use of the minimally invasive approach in aortic valve surgery. The data presented here were obtained retrospectively from our database. In contrast to other groups, we chose the “J” ministernotomy as the only approach for minimally invasive access in aortic valve replacement with central venous catheterization.
LimitationsDespite the limitations of the study, such as the different numbers of patients in the 2 groups, and its retrospective design, the results demonstrate advantages favoring the minimally invasive approach over the standard technique. Since there are no significant differences between the 2 groups in terms of their preoperative demographic characteristics, we consider that they could be comparable. One finding that differs markedly from those reported by most other authors9,15,21,23,24,27,30 is that both the total cardiopulmonary bypass time and the aortic clamp time were significantly shorter in the M group. We consider this to be highly important, as it is known that the prolongation of these times is associated with higher rates of morbidity and mortality. However, this may be explained by a selection bias since, especially at the beginning of the series (the first 20 cases), the patients in whom the minimally invasive technique was used had more favorable demographic characteristics (women over 80 years of age and with valve annuli <20mm were excluded, as were very obese patients of either sex). From patient 21 on, there was no selection bias beyond that related to the choice of surgeon. In the literature, there are reports of series with ministernotomy for aortic valve replacement that show clamp and bypass times shorter than or equal to those of median sternotomy.22,26 With respect to the postoperative variables, we found a clear difference in favor of the M group with respect to the ICU stay and the total duration of the postoperative hospital stay, which were, on average, up to 1 and 2 days shorter, respectively. This coincides with the results reported by different authors.9,16,22,24–26 In a recent meta-analysis that used only randomized prospective studies for the sample,27 the authors also found a reduction in both the ICU stay and the total postoperative hospital stay; however, only the difference in the ICU stay reached statistical significance. In another meta-analysis that included 26 reports, both observational and randomized, the results were similar in that they favored ministernotomy with regard to the hospital stay.30 Nevertheless, those studies in which no differences were observed in these variables did not report longer hospital or ICU stays for the patients who had undergone minimally invasive interventions. In our series, we found no significant differences between the 2 groups in terms of postoperative complications, whether hemodynamic, neurological, renal, or related to the surgical wound, although their incidence tended to be lower in the M group. However, there was a markedly lower rate of respiratory complications, such as pneumothorax, pleural effusion, and respiratory failure. Although the mortality rate was significantly lower in the M group, we should interpret this finding cautiously because of the limited size of our sample and the importance that an uncommon adverse event like death can have. The authors of other series have been unable to demonstrate significant differences in the mortality rate.9,21,22,28
CONCLUSIONSOn the basis of the data obtained in our study, the minimally invasive approach is a safe technique for aortic valve replacement, comparable to the standard approach, that may even offer important advantages, especially with regard to the reduction both in the days spent in the ICU and in the total duration of the postoperative hospital stay. This effect is probably due to the lesser degree of trauma to the thoracic cavity during the intervention, which permits a more rapid recovery on the part of the patients, without increasing the rates of morbidity and mortality. As this is a retrospective report, we consider that prospective studies with adequate numbers of patients are needed to corroborate these findings.
CONFLICTS OF INTERESTNone declared.