To the Editor,
Iatrogenic ventricular septal defect (VSD) is a rare complication following septal myectomy that can cause a rapid postoperative hemodynamic deterioration. We report the case of a 76-year-old dyslipidemic, hypertensive woman who presented with a several-month history of progressive dyspnea. The diagnosis was severe degenerative aortic stenosis, severe hypertrophy of the basal septum (22mm) with a subaortic gradient of 30mmHg, and a mild double mitral valve lesion. On the basis of these findings and a EuroSCORE of 6, the decision was made to perform double valve replacement, mitral and aortic, with bioprostheses, as well as septal myectomy.
The postoperative course was indolent and the patient developed complete atrioventricular block that required implantation of a permanent pacemaker. Transthoracic and transesophageal echocardiography (TEE) led to the diagnosis of a VSD measuring approximately 5mm following myectomy. This defect produced severe pulmonary hypertension (85mmHg) with moderate-to-severe tricuspid insufficiency and a situation of low output (Figure 1). Due to the progressive hemodynamic deterioration and the fact that it was not possible to discontinue inotropic drugs or extubate the patient, the decision was made to close the VSD. Because of the high surgical risk so soon after a recent operation, together with the difficulty associated with a percutaneous intervention, we decided to perform a hybrid procedure. The TEE-guided procedure was carried out in the cardiac operating room. Median sternotomy was performed and, using an 18-gauge needle, a puncture was made through a purse-string suture placed in right ventricular free wall. A short (45cm) 0.035” guidewire was then introduced through the needle. The guidewire was directed toward the VSD and through it. A 7-Fr introducer with the dilator was passed through the defect with utmost care in order to avoid perforating the left ventricular wall. Once the introducer was in place and the dilator withdrawn, a 6/4 Amplatzer Duct Occluder II (AGA Medical Corporation) was loaded into the delivery device and implanted into the VSD by means of the 7-Fr introducer, in accordance with the standard technique (Figure 2). The result was satisfactory; there was a minimal residual shunt in the device and, at the end of the procedure, the pulmonary pressure had decreased from 85mmHg to 40mmHg. The patient was discharged with no complications.
Figure 1. A: transgastric view of the ventricular septal defect by transesophageal echocardiography. B: same image with color Doppler ultrasound.
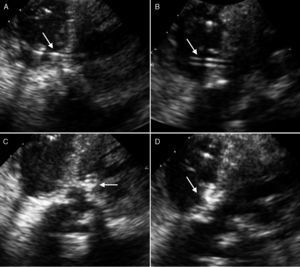
Figure 2. A: passage of the guidewire through the ventricular septal defect following needle puncture of right ventricular free wall. B: position of the introducer after withdrawal of the guidewire. C: placement of the device in the defect with initial release of left disc. D: complete implantation of the device secured to the defect by the discs on either side of the two ventricles.
This hybrid procedure has advantages over surgical closure in that it does not require cardiopulmonary bypass, a circumstance that reduces the risk of myocardial and neurological damage. Another advantage is the continuous monitoring by means of TEE, which enables us to assess and correct, in real time, the position of the device and possible interference with the atrioventricular valves.1
With respect to percutaneous closure, the hybrid procedure offers several advantages such as the fact that it does not require arterial or venous access. Access to the defect and passage of the guidewire through it is simpler with the transventricular approach because the device penetrates at a right angle and the distance from the penetration site is short. This permits better control during delivery of the device, especially in tortuous VSD and those having irregular borders.1 The technique employed in isolated percutaneous closure is complex; it requires access to right ventricle from left ventricle, the creation of an arteriovenous loop with the guidewire, and the use of a snare to trap the guidewire and achieve its externalization through the venous side, to ultimately introduce the delivery system and device into the arterial side from the venous side. In all these steps, difficulties often arise which, under conditions of severe hemodynamic deterioration, can prove fatal. Finally, should closure during the hybrid technique prove impossible or if serious complications develop, there always remains the possibility of immediately incorporating a pump and performing surgical closure.
This case illustrates the fact that a rare complication such as VSD following myectomy can be treated easily and successfully by means of a hybrid procedure, especially in high-risk patients. Moreover, it points out the importance of the collaboration between cardiac surgeons and interventional cardiologists, as well as the need for hybrid operating rooms.
We wish to thank Drs. Raúl Moreno, José M. Oliver, Isidro Moreno, Omar Razzo, Mar Moreno and José L. López-Sendón for their invaluable collaboration in resolving this case.
.
Corresponding author: recalde@secardiologia.es