Of 12 patients with sudden death and a high probability of coronary artery disease who underwent cardiac catheterization, 4 (25%) showed coronary arteries without significant obstructive lesions or angiographic signs of instability. The study protocol included an invasive study of coronary vasoreactivity and an intracoronary imaging study with intravascular ultrasound. The coronary reactivity study showed coronary vasospasm in 1 patient. Intravascular ultrasound showed active coronary plaques with images suggesting intraluminal thrombus in all patients. The diagnosis reached was sudden death secondary to ventricular arrhythmias in the context of acute coronary syndrome; the use of an implantable cardioverter-defibrillator was therefore not indicated. In conclusion, in patients with sudden death with a high probability of coronary artery disease but with coronary arteries lacking significant lesions, intracoronary imaging (eg, by intravascular ultrasound) may be essential to establish a diagnosis and appropriate treatment, even in patients with induced coronary vasospasm.
Keywords
Sudden death (SD) is a public health problem of the first order. Its incidence varies depending on the geographical prevalence of coronary heart disease, but it is estimated that it may be responsible for up to 18.5% of all deaths in developed countries.1 Coronary heart disease is the direct or indirect cause of 80% of these deaths in the Western world,1 which renders coronary angiography a compulsory test for establishing or excluding the presence of obstructive atheromatosis or other coronary problems such as congenital abnormality, embolisms, spontaneous coronary artery dissection, intramyocardial bridge, or spasm.1 Despite strong clinical suspicions of coronary heart disease, it is sometimes impossible to establish the cause of SD since none of the tests performed, including coronary angiography, reveal any significant findings. However, establishing the etiology and physiopathological mechanism underlying SD is essential given their prognostic importance and their influence on the choice of therapy, which may range from coronary revascularization alone to the use of an implanted cardioverter-defibrillator (ICD).
This paper describes a consecutive series of patients with SD and a high probability of ischemic heart disease, but with no significant obstructive coronary lesions, who were studied via the vasospasm induction test and intravascular ultrasound (IVUS).
MethodsThe study subjects were patients admitted to our coronary unit in 2009 with SD who underwent cardiac catheterization owing to the suspicion of ischemic heart disease. All catheterizations were performed within 24 h of admission. We identified patients without significant coronary angiographic lesions, defined as <50% stenosis of the reference segment (visual estimate) and no angiographic signs of an acute coronary event such as a Thrombolysis in Myocardial Infarction (TIMI) flow grade of <3 or an angiographic image of a luminal thrombus, distal embolism or coronary artery dissection. All such patients were subjected to an induced vasospasm test to rule out Prinzmetal syndrome, and IVUS to rule out the presence of active atherosclerotic plaques as a cause of the event. The vasospasm test was performed using acetylcholine at increasing doses (boluses of 10, 20, 40 and 100 μg) injected into both the left and right coronary artery systems. Coronary angiographic images and an electrocardiogram were recorded 1min after the administration of each dose. At the end of the test an intracoronary bolus of nitroglycerine was administered to study endothelium-dependent vasoreactivity. Intravascular ultrasound of all three coronary arteries was performed using an iLab system (Boston Scientific) with automatic retraction.
ResultsFrom January to December 2009, 29 patients were admitted with SD. Coronary angiography was performed in 12 owing to suspicion of ischemic heart disease. Of these, 4 showed coronary arteries with no significant angiographic lesions. The induced vasospasm test could not be performed in 1 of these 4 patients owing to homodynamic instability.
Presentation and Clinical CourseTable 1 shows the baseline clinical characteristics of the 4 patients examined and the results of the non-invasive tests. All of these patients were male; their mean age was 52 (38-68) years. Two patients presented with typical chest pain. One patient suffered SD outside of the hospital, and 3 while in the hospital (2 in the emergency room and 1 on a ward). A transitory elevation of the ST segment was seen in 2 patients and 1 suffered a transitory elevation after cardiopulmonary resuscitation and during the hypothermia induced in the coronary unit. No patient received thrombolysis before catheterization; 3 were eventually treated with aspirin. Enzyme markers of myocardial necrosis were seen in all patients. Left ventricular function, as determined by echocardiography, was normal in all patients except in 1 with prior hypokinesia and mild ventricular dysfunction. All patients evolved favorably except for patient 2, who died of severe post-anoxic encephalopathy.
Table 1. Baseline Clinical Characteristics and Results of Noninvasive Tests
| Patient | Age | Sex | CVRF | Cardiological history | Signs and symptoms | ECG | Troponin I | Echocardiogram |
| 1 | 68 | Male | Smoker | Epigastric discomfort of some months duration | Chest pain and syncope -> CRA | Transitory ST elevation in inferior leads and AVB -> SMVT and VF. After CRA: normalization of the ST segment | 0.10 (initial) | Systolic function of the LV conserved, with no segment alterations |
| 2 | 38 | Male | Smoker, HBP | No | CRA | No ST alterations -> VF. After CRA: normal, transitory ST segment elevation in inferior leads during hypothermia | 1.70 (initial) | Systolic function of the LV conserved, with no segment alterations |
| 3 | 62 | Male | Smoker | Chest pain for 48h previous | Chest pain -> CRA | VF. After CRA: non-specific changes in repolarization | 53.25 (peak) | 50% LV function with anterior hypokinesia |
| 4 | 43 | Male | Dyslipidemia | Chest pain in previous 2 months | Chest pain -> CRA | Transitory ST segment elevation in inferior leads -> VF. After CRA: normalization of the ST | 1.80 (peak) | Systolic function of the LV conserved, with no segment alterations |
AVB, atrioventricular block; CRA, cardiorespiratory arrest; CVRF, cardiovascular risk factors; ECG, electrocardiogram; HBP, high blood pressure; LV, left ventricle; SMVT, sustained monomorphic ventricular tachycardia. VF, ventricular fibrillation.
Table 2 shows the results of the coronary angiography, intracoronary, and functional testing for the 4 patients. The vasospasm test revealed a severe focal spasm in the distal segment of the right coronary artery in 1 patient. Another patient had a mild diffuse spasm in the left coronary artery (a 10% reduction of the caliber at the level of the epicardial artery), and the other 2 patients showed no significant changes.
Table 2. Coronary Angiographic, Intracoronary
| Patient | Artery | Segment | Angiographic findings | Vasospasm test findings | IVUS findings |
| 1 | RCA | Mid | Mild lesion in the mid segment | Focal spasm in distal RCA following administration of acetylcholine. Vasodilation after administration of nitroglycerine | Probable plaque erosion; image compatible with a thrombus. Neutral remodeling |
| 2 | RCA | Mid | Mild lesion in the mid segment | No induction of spasm with acetylcholine, nor changes after administration of nitroglycerine | Ruptured complex plaque; image compatible with a thrombus. Positive remodeling |
| 3 | LMC | Proximal | Mild ostial lesion | Not performed | Ruptured complex plaque; image compatible with acute intracoronary thrombus. Neutral remodeling |
| 4 | ADCA | Mid | Mild lesion in the mid segment | Mild diffuse spasm (<10%) in entire ADCA. Vasodilatation after administration of nitroglycerine | Ruptured complex plaque; image compatible with intraluminal thrombus. Positive remodeling |
ADCA, anterior descending coronary artery; IVUS, intravascular ultrasound; LMC, left main coronary artery; RCA, right coronary artery.
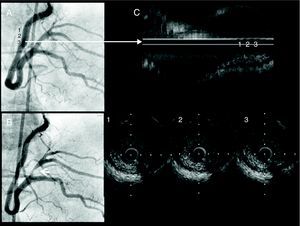
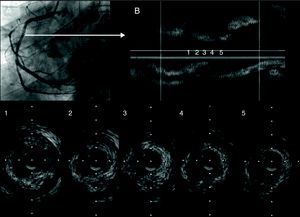
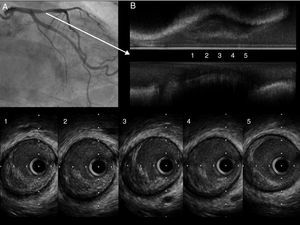
Intravascular ultrasound showed a probable plaque rupture in patient 1, with heterogeneous images possibly compatible with a thrombus at the level of the mid-right coronary artery (Figure 1). The remaining patients presented with ruptured plaques with ulceration and remains of the fibrous capsule, plus abundant intraluminal thrombotic material (Figure 2, Figure 3). Three patients were treated by implanting a stent because they had a minimum luminal area of <4 mm2. Patient 1 was treated conservatively because he had an area of >4 mm2 and his plaque load was <70%.
Figure 1. Patient 1. A: coronary angiography; basal right coronary artery. B: severe focal spasm in the distal right coronary artery following the administration of intracoronary acetylcholine. C: intravascular ultrasound study, with longitudinal reconstruction and transverse slices showing a possible thrombus adhered to the wall over a probable plaque fissure. No ulceration is observable.
Figure 2. Patient 2. A: coronary angiography; right basal coronary artery. B: intravascular ultrasound shows a complex, ulcerated plaque; image compatible with a thrombus.
Figure 3. Patient 3. A: coronary angiography; basal left coronary artery. B: intravascular ultrasound shows a complex, ulcerated plaque with the remains of the fibrous capsule and a thrombus.
DiscussionThree of the 4 patients examined showed ST segment elevation (2 spontaneously, 1 after the induction of hypothermia). The most common mechanisms involved in the resolution of an acute coronary obstruction are coronary spasm, the rapid rechanneling of a coronary thrombosis over a complex plaque by spontaneous fibrinolysis, or both. These mechanisms may be indistinguishable by coronary angiography, but they differ in terms of patient prognosis and the treatment required. During episodes of coronary ischemia secondary to vasospasm, malignant ventricular arrhythmias can appear, such as ventricular tachycardia and ventricular fibrillation.2 The development of these arrhythmias has been used as justification for the occasional implantation of an ICD for the secondary prevention of coronary spasm in the context of Prinzmetal syndrome.2, 3
Intravascular ultrasound was diagnostic in the present patients, and showed the most likely cause of SD to be an acute, transitory ischemic event occasioned by the rupture or erosion of an atherosclerotic plaque. The patients were therefore treated as for acute coronary syndrome with ventricular arrhythmia in the acute phase; an ICD was not indicated. The role of IVUS in a patient who presented with a focal spasm at the level of the distal right coronary artery should be highlighted. This technique revealed the presence of a plaque rupture with a thrombus that was probably the cause of the event. Prinzmetal syndrome would probably have been diagnosed if IVUS had not been used. A recent anatomopathological study found that two thirds of patients with SD had an organized thrombus that had been present for a few days, and that 40% of the lesions causing SD were not severe, especially when the underlying mechanism was coronary plaque erosion.4
The main limitation of this work is the small sample size, a problem of its single center design. However, this is the first study following a protocol of examining the induction of coronary spasm and the IVUS characteristics of SD in such patients. A further limitation is that ruptured atherosclerotic plaques can be present in patients with stable or even asymptomatic angina.5 In the present study, not only did the patients suffer plaque rupture, they had images compatible with a thrombus. Further, in the 2 patients with electrocardiographic changes, the location of the active lesion corresponded with these latter changes; the possibility that the active plaques were found by coincidence and that they were not related to the SD would seem remote. Finally, compared to other techniques such as optical coherence tomography, the resolution afforded by IVUS for the detection of a thrombus is low, although in the cases described the findings were compatible.
The present study indicates that the presence of complicated atherosclerotic plaques is common in patients with SD with no significant coronary angiographic lesions. Non-specific coronary angiographic findings should not, therefore, be understood as sufficient to rule out coronary disease or an acute, transitory ischemic event as a mechanism of SD – a problem of the clinical practice guides issued by the main scientific societies.1 Thus, when a patient presenting with SD is strongly suspected of having coronary disease but has no significant coronary lesions, IVUS may be of use in arriving at a diagnosis and deciding upon adequate treatment.
Conflicts of interestNone declared.
Received 26 August 2010
Accepted 29 November 2010
Corresponding author: Unidad de Hemodinámica y Cardiología Intervencionista, Planta 1a Diagonal, Hospital General Universitario La Paz, P.o de la Castellana 261, 28046 Madrid, Spain. recalde@secardiologia.es